Introduction
The aging process of the population has become increasingly common in most of the countries in the world as a result of scientific, medical and technological advances in the last decades increasing life expectancy.1 Longevity raises concern about the quality of life of the older population because aging is often accompanied by a decline in physical, cognitive and sensory capacity, which may cause limit physical mobility.1,2,3,4 Mobility is defined as the ability to move independently and safely from one place to another; it represents an essential aspect of daily life and favors the autonomy of older adults.5
Mobility limitations are frequent functional problems in elderly people, especially in the oldest ones (≥80 years old). The World Health Organization (WHO) states that about 20% of people over 70 and 50% of people over 85 have some type of disability or movement limitation.6,7 Although many risk factors and aspects associated with mobility limitations have been described in the literature,5,7 their relative importance and independent contribution to the long-term risk of loss of mobility is still unclear.3
Social, nutritional, and functional factors may be involved with mobility limitations. Mobility restrictions are generally associated with physical deconditioning, and they may have an impact on the functioning of physiological systems. The reduction of physiological reserves in older adults over the years facilitates functional limitations.8 However, mobility limitations may occur in several ways, such as difficulties to move, going up or down stairs. Over time, major restrictions involving the use of wheelchairs (using these with insecurity) or locomotion assistance devices may occur.
Also, these limitations referred as physical immobility by some studies are the opposite of “mobility” and they are the ten most frequent health problems among elderly people of both sexes, having some association with several levels of functional dependence.9 Nevertheless, some gaps need to be filled to understand what types of factors are most closely associated with the phenomenon. Given this context, this systematic review sought to identify evidence of prevalence, incidence, and factors associated with mobility limitations in the older adults.
Materials and methods
This is a systematic review of the last five years (2012-2016). The review investigated the evidence of the prevalence or incidence of mobility limitations in the elderly people and their associated factors.
Identification of relevant studies
Papers were sought in the following databases: PubMed, Scopus, Lilacs (Latin American and Caribbean Health Sciences Literature), SciELO (Scientific Electronic Library Online), PAHO (Pan American Health Organization), MedCarib (Caribbean Health Sciences Literature), Repidisca (Pan American Network for Information and Documentation in Sanitary Engineering and Environmental Sciences), Wholis (WHO Library Information System), IBECS (Spanish Bibliographical Index in Health Sciences), PEDro (Physiotherapy Evidence Database), MEDLINE (Medical Literature Analysis and Retrieval System Online) and Bireme (Latin American and Caribbean Center on Health Sciences Information). They were found by doing a search for the following terms: Mobility Limitation, Walking Difficulty, Dependent ambulation, Aged or Aging, Risk or Etiology, Measures of Association or Outcome.
Selection of studies
Those articles that assessed or identified mobility limitations in older people were included. Papers published in Portuguese, English, and Spanish were accepted. Studies of various types -observational, sectional, longitudinal, prospective, retrospective- and papers published in congress proceedings as well as dissertations were searched; theses and abstracts were excluded.
The instrument known as “Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)” was used to verify the items recommended in observational studies.10 This instrument lists information that should be present in the title, abstract, introduction, methodology, results, and discussion of scientific articles that describe observational studies, contributing to an adequate report of this type of study. Also, the recommendation of the “Main Items for Reporting Systematic Analyses and Meta-Analyses (PRISMA)” was followed to structure the review.11 This recommendation consists of a set of items that help researchers to write systematic reviews and/or meta-analyses appropriately. The bibliographic research was carried out between November of 2015 and December of 2016.
Results
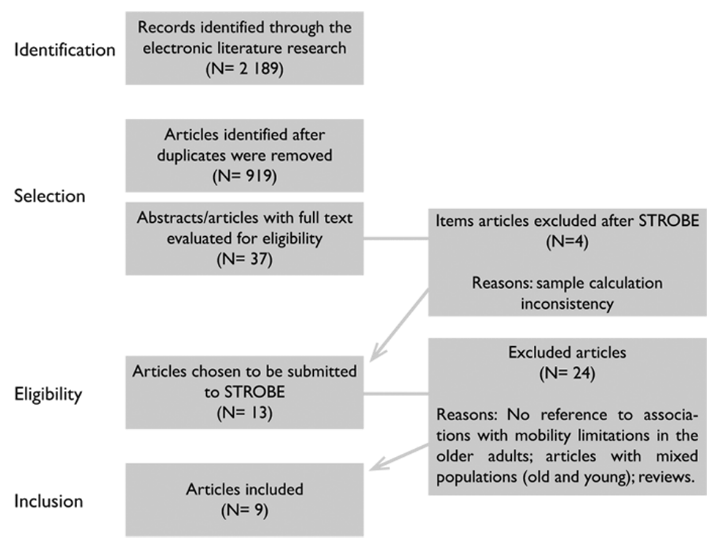
A total of 2 189 articles were found, whose abstracts were read. Whenever there were doubts about the content and subject searched, the article was read in full. Duplicated articles were then excluded, and the list of references of the chosen articles was analyzed for new studies. Thirteen articles were selected and submitted to STROBE10 (figure 1). In the end, nine articles were included in the study (table I).5,7,9,12,13,14,15,16,17
Table I Characteristics of the studies selected by the systematic review
|
First author and year |
Type of study and sample |
Sex Average age (AA) in years |
Study environment and location |
Mobility assessment |
||||
|
(Houston et al., 2013)12 |
Prospective cohort (2099) |
Women (47.9%) Men (34.9%) AA: (74.6) |
Community (USA) |
Interview (difficulty walking a quarter mile or going up 10 steps without rest). |
||||
|
(Alva et al., 2013)13 |
Cross-sectional (90) |
Women (100%) AA: (78.2 ±6.8) |
Hospital (Mexico) |
Guide Euronut-SENECA. |
||||
|
(Murphy et al., 2014)14 |
Prospective population longitudinal (3011) |
Women (51.5%) Men (48.5%) AA: (74.2 ±2.87) |
Community (USA) |
Difficulty walking a quarter of a mile or climbing 10 steps. |
||||
|
(Yeom et al., 2015)15 |
Cross-sectional descriptive (387) |
Women (75.5%) Men (24.5%) AA: (74 ±5.82) |
Nursing Homes (South Korea) |
6-minute walk test (6MWT). |
||||
|
(Gale et al., 2014)16 |
Population longitudinal (5450) |
Non-specified |
Community (United Kingdom) |
Interview; difficulty walking 100 meters, climbing stairs or performing some activity of daily living. |
||||
|
(Dellaroza et al., 2013)17 |
Cross-sectional population (1271) |
Women (59.6%) Men (40.4%) AA: Non-specified |
Community (Brazil) |
Self-report; difficulty in performing various activities and movements, including walking a street (a block), sitting for two hours, getting up from a chair, stooping, kneeling, or crouching. |
||||
|
(Tanjani et al., 2015)7 |
Cross-sectional population (1325) |
Women (52%) Men (48%) AA: (69.14; ±7.37) |
Community (Iran) |
Self-report; Questionnaire; Difficulties in ADLs. |
||||
|
(Stenholm et al., 2015)5 |
Prospective longitudinal population (1013) |
Non-specified |
Community (Italy) |
Self-report; Difficulty walking 400 meters or climbing 10 steps. |
||||
|
(Clerencia-Sierra et al., 2015)9 |
Retrospective observational (924) |
Women (56.8%) Men (43.2%) AA: (82.1 ±7.2) |
Hospital (Spain) |
Barthel Index; Medical records; Decreased ability to perform activities of daily living and impairment of motor functions. |
The studies had varied approaches and a higher percentage of women in their samples, and one study included only females in the sample.13 Sample sizes ranged from 90 to 5 450 individuals, with a mean age between 69.1 and 82.1 years. This demonstrates the scope and extent of these studies, covering several age subgroups within the same life stage. The largest sample was seen in a “longitudinal population” study carried out in the United Kingdom (UK).16
Regarding the location, three studies were performed in North and Central America,12,13,14 one study in South America,17 three studies in Europe5,9,16 and two studies in Asia7,15 pointing out to a variety of population, mostly composed of older individuals.
Mobility assessment
Physical mobility is one of the aspects addressed when assessing functional capacity. It is the independent and safe physical performance of individuals in space locomotion. Individuals who are insecure or have some degree of dependence on locomotion are classified as having mobility limitations. In the review, three studies evaluated mobility based on the difficulty of walking 400 m or climbing and going down 10 steps.5,12,14 One study evaluated the difficulty of walking 100 meters, going up stairs and performing activities of daily living.16 The other studies used the 6-minute walking test (6MWT),15 Barthel index,9 Euronut-SENECA guide,13 self-report,5,7,17 interview12,16 (Houston and colleagues) in 2013,12 questionnaire,7 medical records and ADLs.9
Prevalence, incidence, and factors associated with mobility limitations
The studies indicated a prevalence of mobility limitations in the elderly person ranging from 58.1 to 93.2%, and an incidence varying between 23 and 53.7% (table II). Only one study identified “mobility disability” (22% incidence).
Table II Evidence for the factors associated with mobility limitations in the elderly people based on studies selected by the systematic review
|
Study (First author and year) |
Prevalence/Incidence Mobility limitation |
Statistical tests |
Associated factors |
|||
|
(Houston et al., 2013)12 |
Incidence 36.6% (Mobility limitation) Incidence 22.0% (Mobility disability) |
Chi-square test; Kaplan–Meier method; Tests for linear trends; Cox proportional hazard regression models. |
Low 25-Hydroxyvitamin D |
|||
|
(Alva et al., 2013)13 |
Non-specified |
Analysis of variance (ANOVA); Chi-square test; Fisher exact test; Logistic regression model. |
Sarcopenia |
|||
|
(Murphy et al., 2014)14 |
Incidence 53.7% (Mobility limitation) |
Chi-square test; Spearman’s correlation coefficient (r); Schoenfeld residuals; Logistic regression model. |
High BMI* |
|||
|
(Yeom et al., 2015)15 |
Prevalence 90% (Mobility limitation) |
T-test; Scheffe post hoc test; Multiple regression analysis. |
Sedentary lifestyle; Older age; Low income. |
|||
|
(Gale et al., 2015)16 |
Prevalence 93.2% - Fragile elderly (Mobility limitation) Prevalence 58.1% - Non-fragile elderly (Mobility limitation) |
All prevalence estimates were weighted for sampling probabilities, non-response, and differential sample loss. |
Fragility. |
|||
|
(Dellaroza et al., 2013)17 |
Non-specified. |
Rao-Scott test of association. |
Chronic pain. |
|||
|
(Tanjani et al., 2015)7 |
Prevalence 76% - Women -(Mobility limitation) Prevalence 63% - Men - (Mobility limitation) |
Chi-square test; T-test; Logistic regression analysis. |
Social factors (difficulties of social support: composition of the family and satisfaction with the financial situation and housing possession). |
|||
|
(Stenholm et al., 2015)5 |
Incidence 23% (Mobility limitation) |
Random survival forests (RSFs) method. |
Physiological markers (advanced age in women, restricted hip flexion, the presence of primitive reflexes and tremors). |
|||
|
(Clerencia-Sierra et al., 2015)9 |
Prevalence 89.39% – Overall – (Mobility limitation) Prevalence 91.43% – Women – (Mobility limitation) Prevalence 86.72% – Men – (Mobility Limitation) |
Exploratory factor analysis; Pearson’s correlation coefficient; Tetrachoric correlation matrix. |
Induced Dependency pattern. |
*Body mass index
Most of the studies used a variety of statistical analyses to demonstrate the factors associated with mobility limitations. However, there were logistic regression analyses in most of the research.
The study with the largest sample (5 450 older adults)16 found that fragile older adults had a greater incidence of physical mobility limitation, and the study with the smaller sample (90 older adults)13 showed an association with sarcopenia. Studies with samples of over one thousand elderly people showed association with nutritional, functional and social factors, while those with samples of less than one thousand elderly people showed a stronger association with functional factors (table II).
The social factors that may place the elderly population with mobility limitations at a higher risk of developing disabilities include family composition by other individuals, precarious financial situation and lack of housing.7
According to the review, mobility limitations in advanced ages can act as a cause of illnesses as they affect the reduction of functional reserves in the elderly person (functional dependence)9 and they can also be a consequence when physical and metabolic compromises generate weakness and fragility (sarcopenia, sedentary lifestyle, high BMI, low 25-hydroxyvitamin D).12,13,14,15
Terms used to express the context of the mobility limitations
In the case of physical mobility, most of the studies (eight studies)5,7,12,13,14,15,16,17 used the descriptor “mobility limitation” to refer to the difficulties of locomotion. However, one research also mentions the term “immobility” being treated and understood within the same context as mobility limitations.9
Discussion
Mobility, i.e. the ability to move, is an important indicator of functional independence in older adults. It is inevitable to the instinct of human survival, allowing the organisms to access the means to integrate coexistence and basic health conditions. This review summarized the evidence of the prevalence, incidence and associated factors of mobility limitations in older adults, and showed a high prevalence and incidence of such limitations, expected among older populations.7,9,14,15 However, the variety of forms of mobility evaluation worked as a limiting factor in the study.
Limitations become more significant in older people (aged 80 years or more), indicating that this age group is vulnerable to the development of movement limitations. Aging and diminishing physiological reserves increase the risk of disease and disability through a progressive loss of adaptability to changes during life.18 Regular physical activity reduced daytime fatigue; such activity and improved sleep quality may represent robust strategies to preserve mobility in the elderly population.15,16,17
Women presented a higher prevalence of limitations than men. Moreover, difficulties related to social support (family composition, satisfaction with the financial situation and the housing tenure) proved to be associated with disability and limited physical mobility.7 Social support is important to prevent health implications by providing favorable conditions for the quality of life of both the elderly people and their caregivers. Especially among the less favored financially elderly individuals, lack of support is associated with restrictions on movement and functional dependence.19
Other authors mentioned that sedentary and low-income older adults had a high risk of developing mobility limitations, along with the risk of fatigue, sleep deficit and decreased motor system response to movement.15 Other factors including high BMI and poor physical performance were also shown to be associated with mobility limitations.14 Elderly people with high fat accumulation have more limitations to move and carry out the basic activities of daily living (ADL).20
Both low weight and obesity are associated with a high risk of developing mobility impairments in older people.19 Older people with low weight and malnutrition experience significant levels of movement limitations. On the other hand, the increased intermuscular adipose tissue is positively associated with mobility limitation among the elderly of both sexes.14 Thus, nutritional status is a factor independently and positively associated with functional impairment of mobility and disability.21
In this context, one study pointed out that the incidence of malnutrition is high in elderly patients with sarcopenia, indicating the association of sarcopenia with limited physical mobility, especially with the difficulty of going up stairs.13 Sarcopenia is a common clinical condition among the elderly population. It is a syndrome characterized by progressive and generalized loss of skeletal mass and muscle strength and function, and when this condition coexists with excess body fat, it is defined as sarcopenic obesity.22,23 Both sarcopenia24 and sarcopenic obesity25 are associated with reduced mobility in older people. Thereby, older people with strength and balance restrictions are at a considerable risk of developing mobility limitations.
A prospective cohort study in the United States found an association of mobility limitations in the older adults with low 25-hydroxy vitamin D levels. With this, elderly with 25 (OH) D <50 and 50 to <75 nmol/L presented a higher risk of developing mobility limitation, highlighting that inefficient nutritional intake represents a factor favoring mobility limitations. The prevention or treatment of low 25 (OH) D may provide a way to reduce the burden of mobility impairment among the elderly.12
In the case of physiological mobility markers, the most important predictors are the older age among women, restricted hip flexion, the presence of primitive reflexes, and tremor.5 The prevention of loss of mobility with aging should focus on the prevention and treatment of neuromuscular deficiencies. Therefore, understanding diverse factors is necessary to identify the best means to avoid the onset of deficiencies and disabilities.
In the face of the evidence presented, mobility limitations are perceived to be associated with several levels of functional dependence and they are more often present in older people, even though the possibility of development in younger and comorbid older people cannot be ruled out.9,26,27,28 Limitations may be the cause or consequence of comorbidities acquired throughout life. However, the associated factors are several, ranging from aspects related to loss of strength, balance and muscular power to nutritional inefficiencies and impaired social support.29,30
Conclusions
It was concluded that mobility limitations in older adults are a highly prevalent natural phenomenon of the aging process, and there is evidence of association with nutritional factors and difficulties of social support, as well as functional factors (functional dependence, sedentary lifestyle, among others). Furthermore, mobility limitations can be the cause or consequence of illnesses.
In this perspective, the evidence shows that these limitations must be investigated, studied and understood in a multifactorial approach, in order to allow science to advance in the understanding of their implications for the health of the elderly population.











 text new page (beta)
text new page (beta)