Introduction
Obesity is considered an important global health problem. In 2014, the World Health Organization (WHO) reported that 2.8 millions of people die each year as a consequence of health complications related to obesity.1 Obesity also affected 42 million children under the age of 5 in 2013. Mexico has the highest prevalence in childhood obesity according information from Ensanut 2012.2,3
Imbalance of consumed/expended calories originates a physical state of obesity where different genetic and environmental factors also contribute.4 Altered ratio of gut microbiota (dysbiosis)5 composed mainly by Firmicutes and Bacteroidetes,6 is another factor that contributes to obesity.7 A high relative abundance (RA) of Firmicutes and a low proportion of Bacteroidetes are found in adults with overweight/obesity (OW/O) compared to lean subjects.6,8 Recent studies including ours have shown similar findings in obese children.9,10,11 The risk of OW/O is associated with the high abundance of Firmicutes that is dependent on the high consumption of simple carbohydrates and saturated fats, and low ingestion of micronutrients and fiber.11
Pro-inflammatory cytokines are known to be increased in serum of subjects with OW/O; particularly, IL-6 and TNF-α (which are also referred as adipokines released by adipocytes), that favor insulin resistance and hypertension.12 In contrast, the anti-inflammatory cytokine IL-10 is decreased in these subjects.13 In order to determine if a pro-inflammatory state associated with a type of gut microbiota is found in obese children, we investigated the correlation of Firmicutes and Bacteroidetes with both pro- or anti-inflammatory cytokines in this population.
Materials and methods
Subject and study design
To accomplish the present study, samples from 890 children residents from Mexico City were obtained from a previous study.11 Participants answered a semi-quantitative food frequency questionnaire (FFQ) that included 107-items. All these options were coded for daily consumption of each item for each individual in the study. The grams per serving of each food included in the FFQ to obtain the total energy consumption per day (k/calories) were based on those used for the National Health and Nutrition Survey (Ensanut).14
Physical activity (PA) was measured as physical activity in leisure time, in which frequency (days per week) and duration were asked (never, minutes per day or hours per day). The answers were expressed as metabolic equivalents by hour per week (Mets: h/wk.). Inclusion criteria for the study were non-relative children of 6 to 14 years old. Exclusion criteria were children who had diagnosis of infectious disease, gastrointestinal disorders, administration of antimicrobial agents (within 6 months previous to study), incomplete questionnaires or biological samples. All parents signed the informed consent. The study was approved by the ethics and research committee of Instituto Nacional de Salud Pública (INSP) CI:1129, No. 1294.
Anthropometric features and blood biochemical parameters
Variables of anthropometric features included weight (kg), height (cm), waist circumference (cm) and hip circumference (cm). BMI (kg/m2) was calculated from weight and height. Measurements were performed by previously trained personnel that used standardized techniques and calibrated instruments. Children were evaluated without shoes and with the least amount of clothing. Condition of NW and OW/O were assessed according to the BMI z-score for age and gender as reported by the WHO:15 Normal weight -2 to -1 SD, Overweight >+1 to 2 SD and Obesity >+2 SD).
Venous blood samples were collected after 12 hours fasting for biochemical studies. Values of fasting glucose, total cholesterol, plasma high-density lipoprotein cholesterol fraction (HDL-c), plasma low-density lipoprotein cholesterol fraction (LDL-c) and triglycerides were obtained by using the ILab 350 Clinical Chemistry System (Instrumentation Laboratory IL. Barcelona, Spain). Insulin (μU/mL) was measured by the IMMULITE Chemiluminescent Immunoassay System, and the insulin resistance was calculated by the homeostasis model assessment (HOMA). Systolic blood pressure (SBP) and dyastolic blood pressure (DBP) were measured with calibrated Sphygmomanometer. Two measurements were taken to obtain a blood pressure average.
DNA purification and quantitative Real-Time PCR (qPCR) assays
A container sterile of polypropylene was provided to the parents for a stool sample collection. Fecal aliquots (180 to 220 mg) were stored in a cryogenic vial at -80 °C until use. DNA extraction from feces was carried out using QIAamp DNA stool kit (Qiagen, Hilden, North Rhine-Westphalia, Germany), according to the manufacturer´s instructions. DNA concentration and purity (260/280) was evaluated using NanoDrop 1000 LITE Spectrophotometer (Thermo Scientific, Wilmington, DE, USA). We used the previously reported16 taxon-specific primers to detect the presence of Bacteroidetes/Firmicutes, and universal primers to amplify all members of the taxon. qPCR was performed in a total volume of 10 μl containing 5 ng of DNA, 5 ml of 2X Maxima SYBR Green/ROX qPCR Master Mix (Thermo Fisher Scientific, Foster City, California, USA), 1 pmol and 5 pmol of forward and reverse primers respectively, and 2 ml of DNase/ RNase-Free Water. The PCR program for all primers was as follows: 5 min at 95°C; 30 cycles of 15 s at 95°C, 15 s at 63°C (Universal and Bacteroidetes primers) or 58°C (Firmicutes) and a final cycle of 20 s at 72 °C. PCR amplifications were performed in an ABI PRISM-7900HT sequence detection system (Applied Biosystems, Foster City, California, USA). The specificity of the amplification products and the absence of primer dimers were determined by performing melting curve analyses in all cases. The standard curve for each primer was generated by 5-fold serial dilutions of bacterial DNA. The efficiency of PCR amplification for each gene was calculated using the standard curve method, E=10(−1/slope) −1. Relative abundance of Firmicutes and Bacteroidetes (RA) were calculated using the following formula: 2-∆CT [2-(CT of the Firmicutes/Bacteroidetes primer- CT Universal primer)].17 The RA of microbiota is an estimation of a phylum density over another expressed as bacterial units. It reveals the distribution difference of bacterial population in certain area.
Cytokines measurement in blood
In the same conditions previously mentioned for biochemical studies, another blood sample was obtained and centrifuged to obtain the serum and stored it at -80 °C until use. Serum concentrations of TNF-α, IL-6, IL-10 were measured by ELISA kits according to the manufacturer’s instructions (Peprotech Rock Hill, NJ,8 USA). The absorbance was determined in a Labsystems Multiskan MS. Results were expressed as pg/ml.
Statistical analysis
Results were organized to generate databases for the different variables. In the first analysis, a descriptive study of quantitative data was performed, obtaining data for qualitative variables, frequencies and percentages. Additionally, the Shapiro-Wilk test was used to determine if data have a normal distribution. A non-parametric analysis was carried out with non-normal distributed data calculated by Kruskall Wallis. Logistic regression models were performed to evaluate the association of RA of microbiota and inflammatory cytokines profile within each category of BMI, which were categorized in NW vs OW/O. All models were adjusted for age, gender, total energy intake and heredofamilial history of obesity (variable of family history was based on one or both parents who were or had been obese). The correlation between cytokine profiles and BMI in relation to tertiles of Firmicutes and Bacteroidetes RA was calculated by the Spearman rank correlation coefficient. Statistical analyses were carried out using the version 13.0 from the STATA SE software (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP.). Statistical significant level was considered as P value <0.05.
Results
Clinical characteristics associated with obesity
According to the z-score BMI children were classified in the category of NW (n=383) and OW/O (n=507). These children had a mean age of 9.1 (± 2.04) and 9.3 (± 1.9) years old, respectively. Waist circumference, a potential indicator of metabolic syndrome, was increased in children with OW/O. SBP, DBP, LDL-c, glucose, triglycerides, insulin, insulin resistance and cholesterol were statistically higher in children with OW/O than in children with NW. In contrast, a low HDL-c was found in OW/O children compared to NW subjects. No statistical differences were identified in total energy intake, the total metabolic equivalent task (METs) and gender (table I).
Table I Anthropometric features, clinics, blood parameters and cytokine levels of normal weight and overweight/obese children
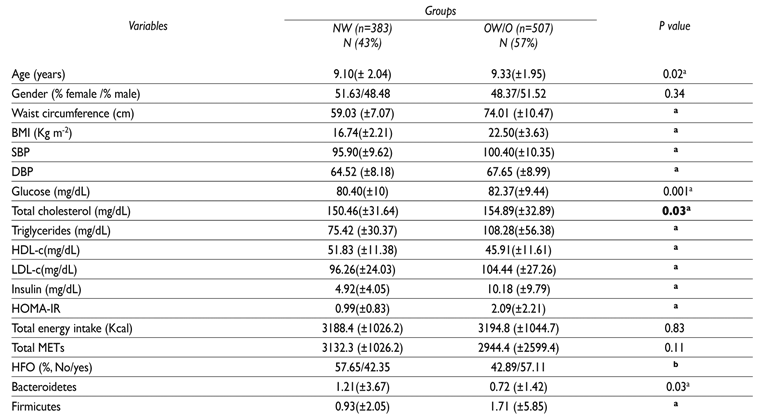
The data are the mean ±S.D. or the percentage. aKruskall-Wallis for continous variables. bX2 test for categorical variables. Normal (NW) or overweight /obese (OW/O); BMI: body mass index; SBP: systolic blood pressure; DBP: dyastolic blood pressure; HDL-c: plasma high-density lipoprotein cholesterol fraction; LDLc: plasma low-density lipoprotein cholesterol fraction; HOMA-IR: homeostasis model assessment of insuline resistance; MET: metabolic equivalent task; HFO: heredofamilial history of obesity; bold text in “P value” column shows significant differences between NW and OW/O; P <0.001
Relative abundance of Firmicutes and Bacteroidetes in obese children
We observed a significant increase in the RA of Firmicutes (1.7±5.9; p <0.001) and a decrease in Bacteroidetes (0.7±1.4; p = 0.03) in children with OW/O compared with NW children (table I).
Association of medium and high RA of Firmicutes in childhood obesity
To evaluate the association of Firmicutes and Bacteroidetes RA with the degree of adiposity, we used a model of multiple logistic regression adjusted for age, gender, total energy intake and heredofamilial history of obesity. RA was classified into tertiles of high, medium and low abundance considering a cut-off based on NW children. We observed a statistically significant association between medium (OR= 2.07) or high (OR=1.69) proportion of Firmicutes and obesity. Furthermore, an inverse association between high tertiles of Bacteroidetes RA was observed in children with OW/O (table II).
Increased TNF-α is related to children obesity
Serum concentrations of TNF-α were significantly increased in the group of obese children (p= 0.01). No significant differences were observed in the levels of IL-6 and IL-10 (table III).
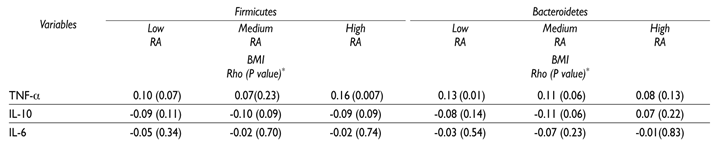
Cytokines and BMI correlation by relative abundance of microbiota in obese children
To evaluate the correlation between cytokine profile and degree of adiposity dependent on gut microbiota RA stratified by tertiles, we calculated the Spearman correlation coefficient. We observed a positive correlation between the concentration of TNF-α with BMI in the highest tertile of Firmicutes (p = 0.02). We also showed a positive correlation of TNF-α levels with BMI in the low tertiles of Bacteroidetes being statistically significant (p = 0.04) (table IV).
Discussion
Gut microbiota plays an important role in the steady state of metabolism and immune responses; thus, an altered ratio of different phyla may lead to diverse health imbalances. In this work, we found a positive correlation between TNF-α serum concentration and the degree of obesity in the highest tertile of Firmicutes RA in children. Other authors have reported an increase in the proportion of Firmicutes in animal models and adults with obesity.18,19 Similar to our results, an increase in the proportion of these phyla was observed in European and African OW/W children compared to NW children.9,10,20 However, several studies in adults have found an increase of Bacteroidetes,21,22 less proportion of Firmicutes, unaltered Bacteroidetes ratio,23 or no differences in the proportions between these two phyla with the obesity degree.24,25 In the present study, we found a high relation of Firmicutes/Bacteroidetes in obese children which is consistent with other studies.7,26,27,28
These controversial results could be explained by lifestyles, ethnic groups,29,30 geographic origin23 and even by the different experimental, bioinformatics and cohort selection methodologies used.31 Diet is considered a trigger of intestinal microbiota diversity by altering the gut microenvironment.32,33,34,35 Recently, we reported that gut microbiota, particularly the phylum Firmicutes and a high fat diet increases the chance of developing obesity.11 This observation is in agreement with our data (table II), where the medium and high tertiles of Firmicutes RA were statistically associated with obesity, suggesting that the amount of Firmicutes RA is important to get a state of obesity. This finding is also related to a previous study where it is suggested that gut microbiota affects the expression of secretory proteins in the gut, which modulate lipid metabolism in peripheral organs.36 Furthermore, metagenomic analysis have shown an overrepresentation of genes involved in energy storage in the obese mice microbiome.26 These results are of great importance since Firmicutes have a greater number of genes encoding for hydrolases and other genes involved in promoting energy uptake from the host diet than Bacteroidetes.26 It was observed in mice that hydrolysis of high concentration of saturated short chain fatty acids is favored by enzymes from Firmicutes. This activity is determinated by the inhibition of intestinal epithelium tight junctions,37 favoring a translocation of LPS to circulation, which is recognized by the Toll like Receptor 4 (TLR4). This receptor activates the NF-kB pathway resulting in overexpression of TNF-α that promotes inflammation.38
A remarkable finding in our study was the presence of inflammation markers associated with microbiota and childhood obesity. We found a positive correlation of TNF-α serum concentrations, with BMI adjusted by age and dependent on the microbiota profile. A correlation of 16% of TNF-α levels was observed in those children with the highest tertile of Firmicutes RA and 13% with the lowest tertile of Bacteroidetes RA. Our findings are consistent with those studies. Although gut microbiota is considered a source of pro-inflammatory molecules that enhance adipose inflammation and macrophage recruitment by signaling through the innate immune system, also is a good source of anti-inflammatory molecules such as the genus Lactobacillus and Bifidobacterium and bacterial species like Faecalibacterium prausnitzii and Lactobacillus plantarum.36,37,38,39
According to our results, we suggest that a constant state of obesity in children is followed by a degree of chronic inflammation with a high expression of TNF-α that may be induced by the altered gut microbiota where Firmicutes phylum prevails. As far as we know, this is the first study that shows a relation between increase of Firmicutes and TNF-α expression in obese children. This study has the limitations of a cross-sectional study to determine the causal effects, however, one of the study strengths is that parameters analyzed were double-blind to avoid bias in measuring.











 nueva página del texto (beta)
nueva página del texto (beta)