Introducción
Tobacco use is considered one of the largest epidemics of a preventable threat to public health worldwide, killing nearly six million people each year.1 Besides being the main cause of lung cancer, it is also a cause of other types of cancers, including oral, esophageal, laryngeal, and pancreatic cancers, and is a major risk factor for cardiovascular disease, aortic aneurysm, peripheral arterial disease, chronic obstructive pulmonary disease, and stroke.2,3Tobacco use is also associated with oral leukoplakia, oral erythroplakia, tobacco-related pigmentation of the mucosa or dental restorations, periodontal disease, halitosis, and failure of dental implants and bone regeneration.4
In 2005, the World Health Organization Framework Convention on Tobacco Control (WHO FCTC) came into force.5 This internationally binding treaty has been signed by 168 countries, 29 of which belong to the Americas region.6,7,8However, only a few of these countries have been able to fully execute the FCTC through the implementation of effective tobacco prevention and control policies.9 Some nations, such as Argentina, Cuba, Haiti, and the United States (US), have signed the FCTC but have not yet ratified it. Surprisingly, Dominican Republic is the only country in the region that has not yet signed the treaty.6 According to the 2011 WHO report on tobacco control for the Americas region, the prevalence of tobacco use among adults in Latin America is 15 to 40%. Tobacco use prevalence is highest in Chile (35%), Bolivia (30%), the US (29%), Argentina (27%), and Uruguay (27%). The prevalence of tobacco use is higher (21%) among females in Venezuela than in other countries of the region, while in Chile (35%), Brazil (30%), Jamaica (29%), Barbados (29%), Ecuador (29%), Mexico (29%), Colombia (28%), and Argentina (27%), tobacco use prevalence is high among youth.7
Isolated reports10,11,12of an alarming prevalence of tobacco use among healthcare providers and students of health professions in Latin America led, in 2004, to the development of the Global Health Professions Students Survey (GHPSS) by the WHO, the US Centers for Disease Control and Prevention, and the Canadian Public Health Association. The GHPSS is a school-based, self-administered survey that captures information from third-year students who are pursuing advanced degrees in dentistry, medicine, nursing, or pharmacy. It collects data on demographics, tobacco use, secondhand smoke exposure, and intention to quit, as well as attitudes and perceptions about tobacco use and smoking cessation technique training.13,14,15,16 The GHPSS has a standardized method for the selection of schools and uniform procedures for data processing.17 Since 2005, the GHPSS has been administered in 21 countries;18,19 its ultimate purpose is to provide baseline and continuous tobacco use assessments that can be instrumental in incorporating tobacco prevention and cessation training in the curricula of health professional programs at universities and colleges and in developing strategies for assisting students and patients with quitting their addiction.
Industrialized countries have developed a wide spectrum of tobacco prevention and cessation interventions based on educational strategies, counseling techniques, pharmacological treatments, and tobacco regulatory efforts, all with the sole intention of discouraging smoking among the general population, including adolescents and young adults.20,21 For instance, the US Department of Public Health has developed two intervention models: the 5 As (Ask about tobacco use, Advise to quit, Assess willingness to make a quit attempt, Assist in the quitting attempt, and Arrange follow-ups) and the AAR (Ask, Advise, and Refer).22 Both have been proven to provide positive results when used by dental practitioners to help their patients quit tobacco use. However, these efforts need to be disseminated more effectively in low- and middle-resource settings, and even more importantly, they must be culturally adapted to the existing socio-economic and cultural contexts of each country.23,24
Healthcare providers are positioned to offer unique and efficient tobacco prevention and treatment.25 In particular, dentists have an important role in the battle against the tobacco epidemic since most of the early signs of tobacco use are observed in the oral cavity.26,27,28 Furthermore, scientific evidence has shown that behavioral interventions, in addition to oral examinations in dental settings, increase the abstinence rate among patients who are current smokers.29 However, the lack of sufficient opportunities for tobacco prevention and cessation training in many Latin American dental schools is hampering the opportunities for dental professionals to become fully committed in the fight against tobacco use in the region.30 Even more, studies conducted in other regions have shown that smoking among health care providers has a negative impact on their beliefs and attitudes towards tobacco control measures.31 Also, little is known about dental students’ tobacco use prevalence and knowledge on this topic. Therefore, the objective of this study was to examine the association between tobacco-related risk factors (e.g., knowledge and attitudes) and smoking among third-year dental students in Central and South America.
Materials and methods
Study design and population
In this cross-sectional study, we analyzed GHPSS data, collected between 2001 and 2012, on tobacco use and cessation counseling among undergraduate dental students from Argentina (2007), Bolivia (2007), Chile (2008), Costa Rica (2012), Guatemala (2008), Mexico (2006), Panama (2008), Paraguay (2008), Uruguay (2008), and Venezuela (2001). We used the latest wave of GHPSS data for each country.
For the purpose of this manuscript, all data analyses were restricted to third-year dental students aged 15 years or older (n=5 605 individuals) since students in Latin American dental schools begin to function as dental practitioners during their third year. This study was approved by the Institutional Review Board of The University of Texas MD Anderson Cancer Center (Protocol # PA15-0741).
Main outcome
Dental students who responded “Yes” to the question “Have you ever tried or experimented with cigarette smoking, (even one or two puffs)?” and who also smoked for at least 1 day after being asked “During the past 30 days, on how many days did you smoke cigarettes?” were classified as current smokers. This categorical variable was dichotomized as Yes or No. Non-current cigarette smokers were those participants who had never tried or experimented with cigarette smoking (never smokers) as well as those who had tried or experimented with cigarette smoking but did not smoke cigarettes during the previous month (former smokers).
Statistical analysis
Both descriptive and inferential data analyses were performed using SPSS version 22 software, with 0.05 as the level of significance. The frequency distribution, mean, standard deviation, and proportions were calculated, and current smokers and non-current smokers were compared using chi-squared and independent t-test analyses.
Bivariable and multivariable logistic regression model analyses were performed to determine the association between independent variables (e.g., sex, age, country, secondhand smoke exposure, self-perception as a “role model” for patients, belief that health care providers have a role in advising patients or informing them about smoking cessation, belief that health care providers who smoke are less likely to advise patients to quit, and formal training in smoking cessation approaches to use with patients) and current cigarette-smoking. A multiple logistic regression model for estimating the probability of being a current smoker was constructed using a stepwise selection algorithm, with entry and exit p-value criteria of 0.05 and 0.10, respectively. Unfortunately, the question on the enforcement of tobacco-free policies in dental schools was absent from the GHPSS version used in Chile. Therefore, this variable was excluded for this particular analysis.
Results
The study sample consisted primarily of women (64%), the majority of whom (81%) ranged in age from 19 to 24 years. Table I summarizes the descriptive statistics of the study population.
Table I Socio-demographic and behavioral characteristics of third-year dental students from several in Latin American countries (2001-2012), stratified by smoking status (n=5 488)
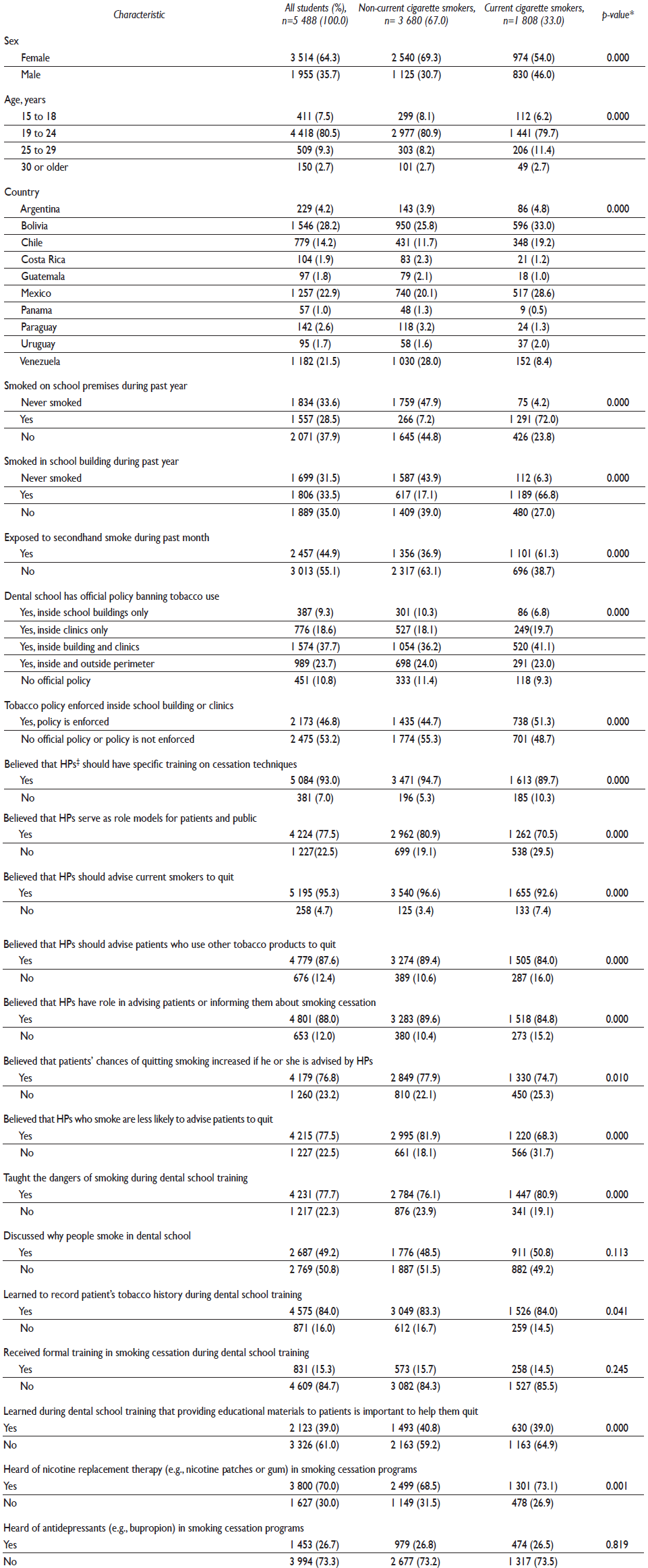
* Significant association (p<0.05)
‡ HP = health professional
Among the 5 488 undergraduate dental students who responded to the questions related to current smoking, 1 808 (33%) reported smoking cigarettes at least one day during the past 30 days, while 2 457 (45%) had been exposed to secondhand smoke during the previous month. Among both former and current cigarette smokers, 67% had smoked in a school building during the previous year. Among the students in our study sample, only 15% had received formal training in smoking cessation.
One finding of particular interest was that, among current cigarette smokers, 42% responded “Yes” to the question “Do you want to stop smoking now?” In addition, 65% of the cigarette smokers indicated that they had made attempts to stop smoking during the previous year. Sixty four percent of these dental students had not received help or advice to assist them in their quitting attempts. These results are not shown in the tables.
The association between cigarette smoking and specific independent variables was examined in a multivariable logistic regression model. The tolerance and variance inflation factor were examined for each variable included in the model; all were > 0.2 and < 3.0, respectively, indicating no concerns with multicollinearity.
Being male (OR adj=1.85; CI=1.600-2.145; p<0.01); Bolivian (OR adj=1.78; CI=1.026-3.085; p<0.05), Chilean (OR adj=2.19; CI=1.273-3.779; p<0.01), or Mexican (OR adj=1.89; CI=1.084-3.294; p<0.05); being exposed to secondhand smoke (OR adj=2.55; CI=2.253-2.896; p<0.01); lacked self-perception of being a “role model” for patients (OR adj=1.42; CI=1.227-1.638; p<0.01); and not believing that health professionals who smoke are less likely to advise patients to quit smoking (OR adj=2.05; CI=1.772-2.367; p<0.01) were factors that were significantly associated with current cigarette smoking (table II).
Table II Risk factors associated with current cigarette smoking among third-year dental students from several Latin American countries (2001-2012) (only variables with statistical significance are shown in the table)
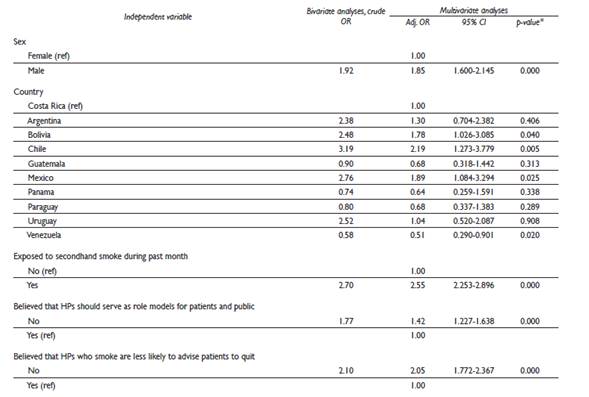
* Significant association (p<0.05)
OR= odds ratio
CI= confidence interval
HP= health professional
MODEL: current smoking vs. non-current smoking. The following variables were adjusted for in this multivariable model: sex, age, country, secondhand smoke exposure, self-perception as role model, belief that HPs have a role in advising patients or informing them about smoking cessation, belief that HPs who smoke are less likely to advise patients to quit, and formal training in tobacco cessation
Discussion
The findings from this cross-sectional study provide a unique opportunity to assess not only tobacco use prevalence but also perceptions and risk factors associated with tobacco consumption among third-year students pursuing an advanced dental degree in several Latin America countries (Argentina, Bolivia, Chile, Costa Rica, Guatemala, Mexico, Panama, Paraguay, Uruguay, and Venezuela).16 Like the findings of Warren and colleagues14 in their analysis of 2005-2007 GHPSS data from countries around the world, our results show a high prevalence of tobacco use among dental students from several Latin American countries (33%). Contrary to the results of previous reports13,32,33,34the overall prevalence of tobacco consumption was higher among female than male dental students in our study sample. However, this sex difference varied by country according to the prevalent beliefs and norms around tobacco use.35
The highest frequency of tobacco consumption among dental students was observed in the group aged 19 to 24 years. Many of the respondents reported trying their first cigarette before age 17. This is consistent with the results of previous reports that indicate that freshman college students who smoke have already begun smoking before they arrive on campus.34 Cigarette smoking was predominant compared to other types of tobacco consumption, which is consistent with the results of previous reports from this region24 but differs from what is observed in other countries, particularly those in the Middle East.14
As in previous studies, we found evidence of a significant association between exposure to secondhand smoke and current smoking status.36,37While many countries have existing policies that prohibit smoking in public and in work places,6,38,39,40these laws are not always enforced with rigor.41 Unfortunately, a trend toward the relaxation of antismoking rule enforcement is occurring, even in academic institutions where health-related careers are offered.13,42,43Adherence to these regulations, asserted Muñoz Escobedo and colleagues,44 must be mandatory in any healthcare institution and followed by everyone involved, including administrative and teaching personnel, students, and patients.
According to Cauchi and Mamo, student smoking adversely affects the beliefs and attitudes of students toward tobacco control policies.37 In this study, we observed that dental students who smoke or have smoked within educational buildings do not consider themselves to be role models for society. Therefore, it is increasingly important for dental education institutions to provide not only training opportunities in tobacco prevention and cessation but also tobacco treatment services for dental students and faculty members who use tobacco products.
According to Weaver and colleagues,45 a high percentage of smokers report having seen a dentist at least 1 time in the previous year. This suggests that dentists are well positioned to play an important role in public health strategies to reduce the morbidity and mortality associated with tobacco use.46
A new generation of dentists in Latin America should be aware of the key role they can play in intervention strategies aimed at battling tobacco consumption, creating awareness among these practitioners about the health risks associated with tobacco use and its impact on the quality of life of their patients.6,47Previous findings13,24,48and the evidence shown in the present study clearly indicate a lack of training for dental students on how to provide effective anti-tobacco counseling as well as successful pharmacological and non-pharmacological strategies to help their patients with smoking cessation.49,50,51We believe that undergraduate and graduate dental programs in the region should adopt a tobacco control strategy that involves the adoption of tobacco prevention and cessation training into their curricula and the inclusion of tobacco prevention and cessation training in the portfolio offered by their continuing education programs. Approaches such as the 5A and 5R models have already been proposed for this purpose.52
Four important caveats should be mentioned as limitations of this study. First, not all of the dental schools and programs in Latin America participated in each wave in which the GHPSS survey was conducted. Second, data from each of the countries participating in this study were collected in different years which, together with variations in national trends of tobacco consumption and the implementation of anti-tobacco policies, make it extremely difficult to compare dental students and the general population or the countries in our sample. Third, this study only included third-year dental students. This could result in a selection bias because for some dental schools, formal training in tobacco prevention and cessation could have taken place in later years. However, we firmly believe that by the third year, dental students should be exposed to this special training to allow subsequent opportunities for increasing levels of self-efficacy. Finally, the number of responses varied considerably by country, and Bolivia (1 546 students), Mexico (1 257 students), and Venezuela (1 182 students) were overrepresented in our study sample. In this sense, dental schools in all Latin American countries should be encouraged to repeatedly participate in future waves of the GHPSS survey so a uniformed and homogenous representation can be obtained. This will make it possible for each country to track changes in tobacco use and associated risk perceptions among dental students over time and to evaluate the impact that any anti-tobacco policy implemented at the institutional or national level has on the performance of these future health professionals.
Dental associations, oral health societies, and other organizations or institutions sponsoring and promoting scientific meetings should include tobacco prevention and control as an important topic for discussion. This exchange of research ideas and practice experiences will undoubtedly benefit dental care professionals who may be facing similar challenges around tobacco prevention and cessation in their dental offices or academic institutions.
We believe that the findings of this cross-sectional study will encourage dental schools in the region to design and implement new tobacco prevention and cessation training programs for dental students. In institutions where these programs already exist, developing continuing education programs for dental practitioners and specialists will guarantee the positive impact of dental professionals in the battle against the tobacco epidemic.











 nueva página del texto (beta)
nueva página del texto (beta)


