Introduction
Primary care is the entry point into the health system; therefore, it is essential to assure the quality and efficiency of the services. Resources and supplies must be sufficient, care quality -operationalized as the appropriate process of technical and interpersonal dimensions of care- should be provided, and adequate response capacity should exist, including coordination mechanisms necessary to obtain the support of more complex levels of care when required.1 A key determinant for care quality is the training and updating of the health personnel,2 based on learning needs.3
In low and middle-income countries, one major problem in primary care services is the allocation of health work force mainly in urban areas; in addition, available health personnel has mixed skills, as well as scarce opportunities for continuing education to provide quality health care.4 In some Latin America countries, this situation has a multifactorial origin influenced by the rigidity and imperfections of the health system in identifying the needs for continuous improvement.5,6
Across the Mexican public health care system, primary care provides ~85% of outpatient care, which in the year 2013 amounted to ~280 million visits,7 i.e. an average of two visits per year per inhabitant. At this level of care, inefficiency in the actions of health promotion and disease prevention, low resolution of acute clinical conditions, and poor control of chronic diseases along with their complications have been extensively documented, and comprehensive strategies including managerial and educational interventions aiming to improve the quality of health care have been recommended.8,9,10
In rural areas, health facilities are nestled in small communities. These centers are staffed by only one or two health care teams (General Practitioner [GP] and a nurse), who are responsible for the care of the population from several localities. The members of this minimal staff must implement promotion and prevention programs while providing curative care. They work in isolation and with scarce resources to meet local demands. In addition, there is often lack of an efficient communication network for timely referral for specialized care of patients with more complex diseases.11
In these remote areas, the opportunities provided by the health care system through continuing education programs are ineffective. Therefore, it is justifiable to implement comprehensive strategies to improve the quality of care through innovative interventions aimed at training and continuous updating of health teams that, by responding to their education needs, can improve care practices, promote integration as working teams, enhance coordination as a network among levels of care, and represent incentives for a sustainable development performance.
The success of such interventions depends on whether or not they are applicable to the context. Thus, it is important to analyze the current conditions of the health services and their potential for improvement, in order to establish the best approach for larger-scale program. Therefore, the objective of this study was to evaluate the feasibility and acceptability of a comprehensive educational strategy designed to improve the quality of care for the main causes of visit in rural health centers in Mexico.
Materials and methods
In 2014, a demonstration study was conducted in two health jurisdictions (technical and administrative departments, responsible for the operation of health programs at district level) belonging to the State Health Services of Veracruz (a State located in the east coast of Mexico, where almost half of the population lives in rural areas). This study consisted of an educational intervention based on academic detailing to healthcare teams of 18 rural health centers consisting of one or two “basic core services” (i.e. functional units of health centers comprised by a GP and one or two nurses) selected by a convenience sampling. The outcome variables were the feasibility and acceptability of the intervention.
The intervention consisted of the following three components:1) development of the contents of the strategy; 2) selection and training of instructors; and 3) implementation of the educational strategy.
1. Development of the contents of the strategy
Six clinical conditions corresponding to the main reasons for primary care visits were included, organized into three pairs according to the following three population groups:
Women: Prenatal care/genitourinary infections
Adults: Type 2 diabetes/hypertension (T2DM/Hypertension)
Children <5 years of age: upper respiratory infections (URI)/well-child monitoring (nutrition, growth and development)
For each clinical condition, evidence-based critical recommendations for primary health care were selected.12All recommendations were according to the Clinical Practice Guidelines (CPG) of the Mexican Health System.13
2. Selection and training of instructors
Two groups of instructors were defined according to their functions and level of care. The first group was comprised of medical specialists and experienced nurses for each pair of clinical conditions per population group -obstetrics and gynecology, internal medicine, and pediatrics-, selected from the referral hospital of the participating health centers. Instructors of this group were chosen due to their high clinical competency in their specialty, teaching experience, interest in voluntary participation in the project, and attitude to encourage discussion and exchange of views with peers. The main purpose of involving hospital specialists in the study was to improve communication between levels of care in order to: 1) facilitate the referral/counter-referral process; 2) afford timely specialist advisory for complicated cases; 3) provide training to field instructors (training of trainers strategy).
The second group of instructors (field instructors) consisted of GPs, nurses and health promoters who represent the supervision team at the jurisdiction level. This team is responsible for monitoring health program activities and care processes at the health centers in a specific area. After obtaining their consent and willingness to participate in the project, three supervision teams for each health jurisdiction were selected. In order to train field instructors, each specialist (according to the pair of clinical conditions to be addressed in the training), together with the research staff, conducted a 1-day (6 h) workshop covering two topics: a) methods for providing the academic detailing strategy with emphasis on interaction with the health care team; and b) strategies for facilitating the implementation of guidelines based on the selected critical recommendations.
3. Implementation of the strategy
The strategy was performed sequentially for each pair of clinical conditions, with a total duration of 6 months. Previously, the strategy plan was presented to all the teams of the chosen health centers, and they were invited to participate in the study. Each jurisdiction team of field instructors was responsible for three health centers and carried out scheduled rotating visits to each health center on a weekly basis, remaining for 2-4 h with the health care team (physician and nurse),who participated in the following successive activities:
Introductory workshops. A 2-h workshop for every pair of clinical conditions was carried out by the corresponding instructor during the first visit. The aim was to facilitate the interaction between the health team and the instructors through review, discussion and agreement on the criteria and recommendations included in the CPG.
Individual tutorial (three visits per pair). The purpose was to strengthen the application of the management criteria in daily practice through personal interaction among instructors, physicians and nurses. For this component of the strategy, joint care was provided (by the health team and field instructors) to patients with the corresponding clinical condition; visits included comprehensive case evaluation and specific management according to CPG: pharmacological, non-pharmacological, health promotion, and timely referral by the health care team. For all activities, the patients were informed by the healthcare team, and their consent was sought for joint care with the counseling of instructors.
Case-review sessions. After each round of visits to the health centers, all health teams with their respective field instructors met with the specialized instructors (medical and nursing hospital instructors of the respective pair) at the corresponding referral hospital, for the discussion of clinical cases selected by the health care center team from their own practice, based on the difficulty to provide a diagnosis or treatment. The round-table case review sessions aimed to compare actual case management with CPG standards, obtain recommendations from hospital instructors, engage in-group learning, and establish a permanent communication channel to organize coordinated processes for referral and counter-referral in those cases needing specialized ambulatory care or hospitalization.
Evaluation
The evaluation was performed using combined (quantitative/qualitative) methods. Measurement of the feasibility was completed using checklists (initial measurement) and direct observation at the health centers (during the intervention) by members of the research team, including three aspects of the management and administrative procedures: 1) material resources required for health care (equipment, drugs, supplies, vehicles and travel expenses for the field instructor teams); 2) process (completing academic detailing activities within the usual operation of the services); 3) human resources (availability of jurisdiction and specialist instructors).
The acceptability of the intervention (final measurement) was evaluated by the health teams and instructors using a self-administered, anonymous questionnaire to obtain information regarding seven areas of intervention:
1) Instructors’ performance
2) Relevance of the topics
3) Relevance of the strategy
4) Health teamwork dynamics
5) Interaction between the health team and instructors
6) Interaction between the health team and services at the referral hospital
7) Effect of the intervention on quality of care
In addition, the questionnaire included two open questions to explore the facilitators and the barriers to the successful implementation and fulfillment of the strategy for improving the quality of health care.
The qualitative component consisted of semi-structured interviews with key informants, with prior informant consent. An interview guide was developed to obtain their perception regarding the facilitators, barriers, areas of improvement after the intervention, and sustainability/escalation. The guide included issues about the overall intervention; CPG; communication and coordination among the health team members and with the instructors; organizational aspects; and care quality. The number of interviews was defined according to convenience. All interviews were audiotaped and transcribed.
Data Analysis
The feasibility and acceptability data were analyzed using simple frequencies and percentages. Analysis of the qualitative component was based on the conventional content analysis.14 The information was grouped according to codes and families in order to organize the testimonies of the interviewees and selected topics and subtopics, including emergent topics not considered in the interview guide. Each respondent had an assigned key in order to ensure anonymity. The information was processed with the Atlas.ti v6.2software.a
Results
Forty-eight participants from health centers were included. There was a similar proportion of physicians and nurses. Physicians were distributed equally between GPs and undergraduate physicians in field professional practices (social service activities). Most of the staff were <36 years of age, and more than half were women; only 10% reported >5 years working at the health center, and one third of the staff had a permanent job contract (table I).
Table I Characteristics of the personnel at the health centers. State Health Services, Veracruz, Mexico. 2014
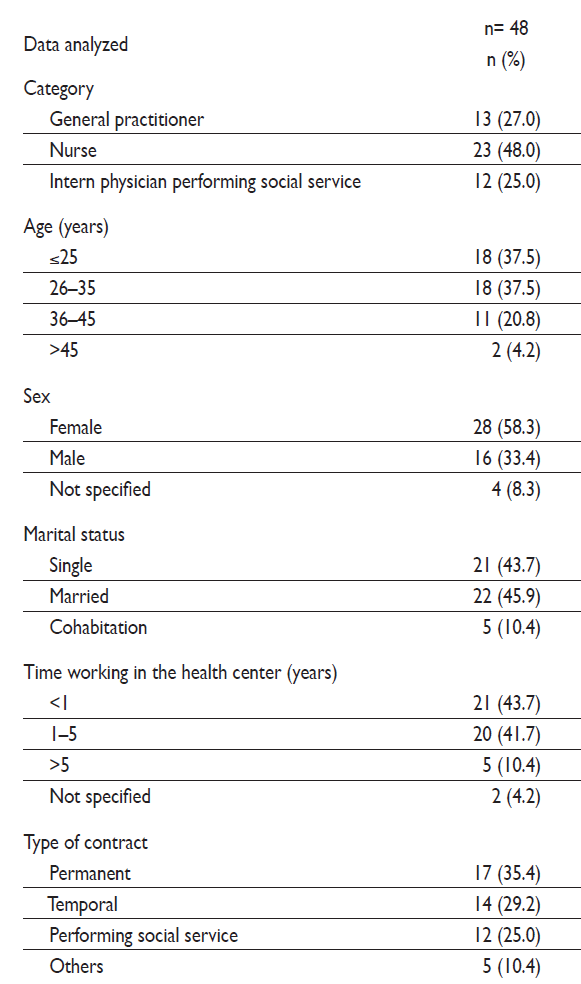
Source: Questionnaires to participants
Feasibility
The infrastructure and equipment of the 18 health centers were variable. Half of these centers had insufficient general conditions regarding facilities, signage and lighting. Cleanliness of the unit was satisfactory; however, only four (22.2%) of the units had supplies for hand washing. Medical care equipment was sufficient in most centers; 83.3% had computer equipment, and only two (11.1%) had radio equipment. At the baseline stage, the supply of medications for the six health conditions included in the study was insufficient or non-existent according to the national CPG. The greatest shortage was of insulin, statins, some antibiotics and vitamin supplements (data not shown in table).
In both health jurisdictions, as in the two referral hospitals, managerial support was obtained for the improvement of the supply of consumables, organization and logistics. Instructor teams had the time required to perform scheduled visits; jurisdiction teams (medical instructors, nurse, and health promoter) and hospital specialists were fully available throughout the project as planned. Despite this, there was difficulty in providing appropriate arrangements for the transportation of field instructors to the health centers, and therefore they often encountered delays and in some cases had to suspend their visit due to the unavailability of vehicles. In health centers, the care process was reorganized according to the program of visits without the usual provision of services being affected. Users accepted the participation of the instructors during care, and health teams collaborated in joint activities of medical consultation and health promotion.
Acceptability
Table II presents the scores that the participants awarded to the training for each pair of selected clinical conditions. The rating given was high for all items except for the working coordination with the referral hospital, which showed lower values. As for the reasons given for quality improvement resulting from the intervention, training through personalized advice by the jurisdiction instructor and teamwork improvement were emphasized ( table III ).
Table II Score provided for the intervention by the participants. State Health Services, Veracruz, Mexico. 2014
* Scale 0–10, where 0 is the worst opinion and 10 is the best
‡ Jurisdiction instructors rated the performance of hospital instructors
GU: Genitourinary
TDM: Type 2 Diabetes
URI: Upper Respiratory Infection
Source: Questionnaires to participants
Table III Motives expressed for improving the quality of care after the intervention. State Health Services, Veracruz, Mexico. 2014
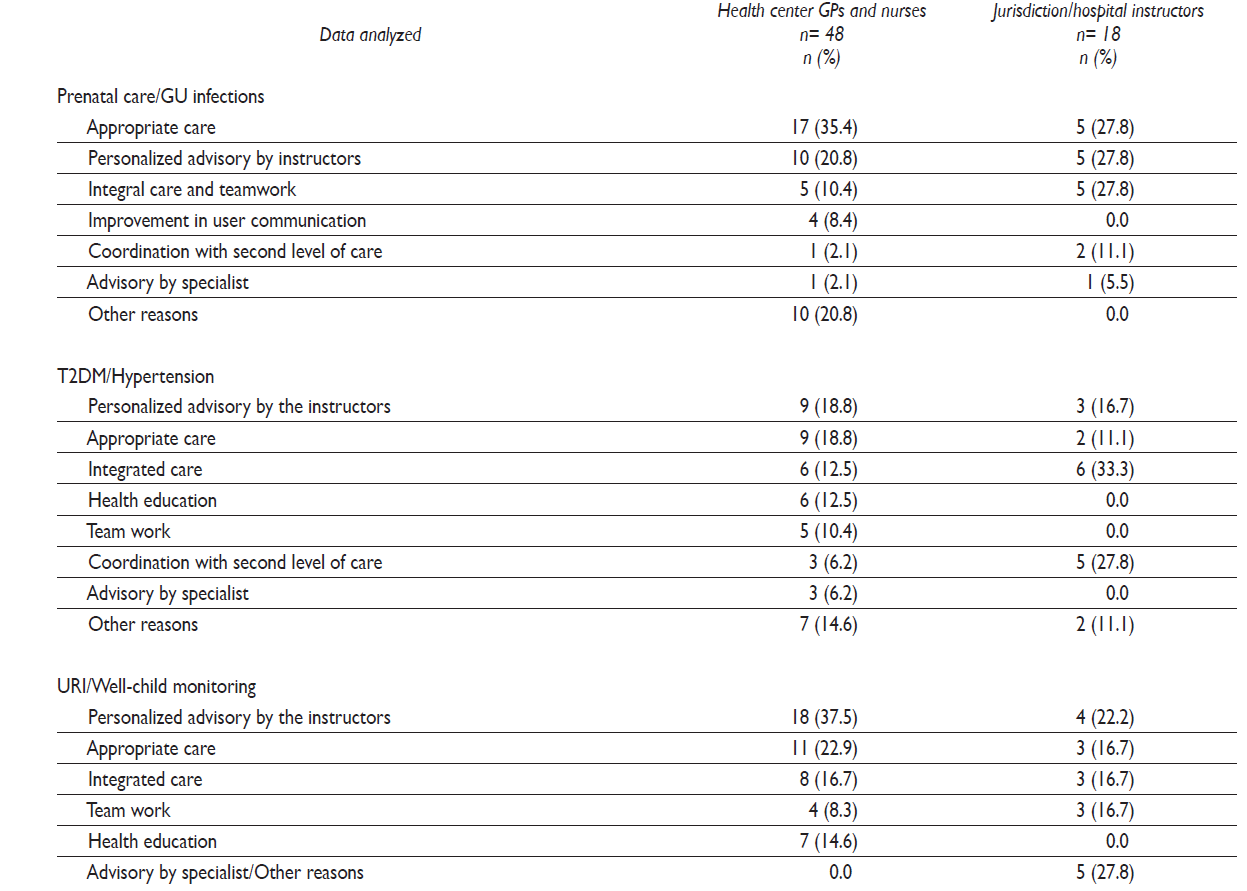
Source: Questionnaires to participants
Barriers mentioned for complying with the intervention activities differed between the health center and the jurisdiction instructor teams: the former highlighted the lack of consumables and the limited time available for comprehensive care, whereas the latter identified transportation problems that arose when visiting health centers as the main obstacle to providing scheduled visits (table IV).
Table IV Barriers to the successful implementation of the strategy identified by the participants. State Health Services, Veracruz, Mexico. 2014
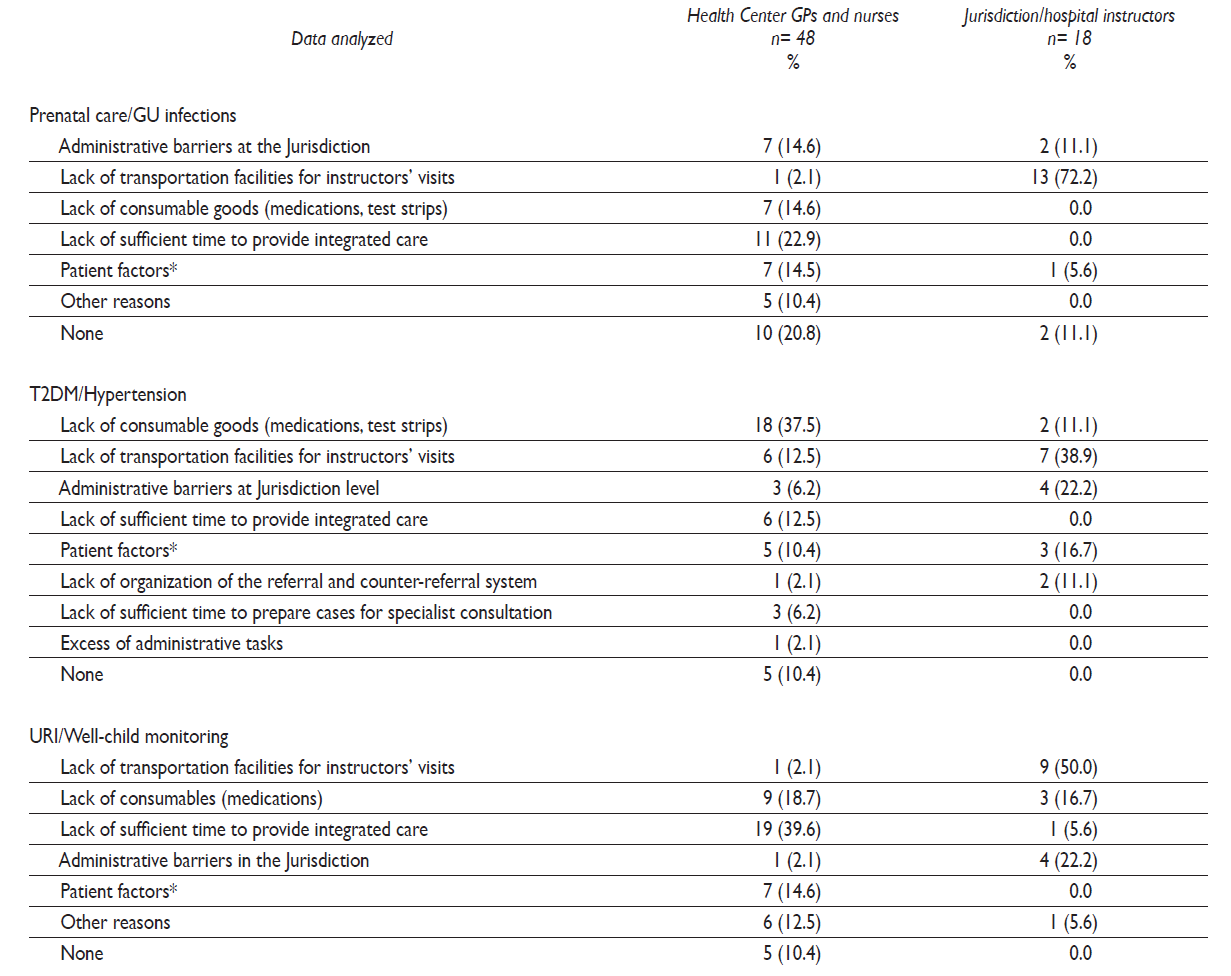
* Lack of confidence in care, lack of adherence to appointments and treatment
Source: Questionnaires to participants
Regarding the qualitative component, 19 interviews were conducted. The age range was 25 to 60 years (average 42.5 years); 11 were men and 8 women, and 63% were physicians. The longest time in the current position was 9 years and the shortest amount of time, <3 months. Codes corresponding to interview topics are shown in table V.
Table V Coding catalog from the interviews. State Health Services, Veracruz, Mexico, 2014.
Source: Prepared by the authors
The general perception of the project was good mainly because it favored a professional upgrade through instruction and advisory activities that replaced administrative supervision (quotes represent selected literal expressions used by participants).
I think it is really strengthening to have an advisory component within the health centers. Rather than becoming supervisors we are becoming instructors. As supervisors we are dedicated to reviewing and auditing processes according to the rules. As instructors, we have the opportunity to review clinical cases, to be in contact with the healthcare personnel and to directly address a patient (Jurisdiction Medical Instructor).
The commitment of jurisdiction instructors and specialists, and their availability to answer questions and to resolve problems in patient care were considered for purposes of counseling and training. The ease of interpersonal relationships among participants was recognized, and so was the improved coordination between levels of care arising from the professional relationship that the project facilitated. As for the usefulness of the CPG, identification of specific recommendations for clinical decision-making was mentioned as important. Organizational improvement was repeatedly expressed as better availability of medications for the clinical conditions included in the project and better communication among managers at different levels:
Actually, this (intervention) helps greatly. Instruction was quite extensive. If we encounter a problem, help is always available for problem resolution (Nurse, Health Center).
Difficulty in regard to CPG usefulness was also expressed as barriers:
I think it would be more helpful to have CPG presented as a flow chart. In this way, we could easily access, in a simple and user-friendly form, the information on how to monitor the patient and proceed with treatment (GP, Health Center).
The main barriers identified were those related to the need for supplies:
I would say lack of medications and diagnostic resources are the main challenges. For example, the diagnostic equipment we have -such as ophthalmoscopes and otoscopes, sphygmomanometers and stethoscopes- is already in poor conditions (Auxiliary Nurse, Health Center).
Regarding the strategy results, it was consistently referred to as successful in updating knowledge through academic detailing, as well as in promoting greater integration among levels of care, and improving interpersonal relationships within the healthcare team:
Another advantage is that multidisciplinary integrated management establishes an actual healthcare team. Before, we used to work individually, not just with different levels of care but within the health center itself (Jurisdiction Medical Instructor).
Finally, challenges in regard to the sustainability and scaling up of the strategy, mainly due to the need for and difficulty in securing supplies and resolving identified organizational barriers, were expressed.
Discussion
The results showed some important issues regarding the feasibility and acceptability of quality improvement strategies to be applied by the health personnel in rural areas. There were positive aspects. First, the participation of local instructors in their own work environment, and the availability of specialists from referral hospitals to provide support for complicated cases by giving advice and care were central factors for achieving teamwork learning among healthcare workers. The effectiveness of continuing education has been widely demonstrated,15,16and the potential long-term effects of educational outreach visits on health professional practice or patient outcomes have been recognized.17Recently, an interprofessional education approach has been considered to be a potential way for improving teamwork, patient-centered care, and care quality,18 also within the rural context.19,20
Second, the acceptability of our approach is also indicative of the importance of the professional relationship among health team members for providing comprehensive care, in which these teams can be health care leaders, and legitimizes their actions.21 To achieve this goal, it is essential to consider the expectations of the health team itself, their perceived needs for innovation and the compatibility with the demands of their job responsibilities.22
However, it is worth to recognize that adopting a new model for continuing education requires a favorable organizational context. As in many other developing countries, the organization of the Mexican health system for the rural population includes the decentralization of health services.23,24Decentralization has been considered by the World Health Organization as a “key pre-requisite” to improve the progress of primary care.25 Even so, there is a need for innovative structural organizational strategies;26 this remains a pending task within the Mexican context. The initiatives described in this study may represent contributions in that direction; similar needs and proposed matching strategies in comparable contexts have also been documented to support the integration of local networks to respond to the priorities of care for the rural population.27
It is important to tackle some organizational barriers, including the burden of daily practice, the isolated practice of each health professional, and a hierarchical culture that limits communication within the healthcare team and with other levels, as has been reported in similar environments.28 Breaking these barriers requires the incorporation of actions to foster an atmosphere of respect and collaboration, build the commitment of all participants, and strengthen shared experiences for the benefit of the population they serve, as well as to achieve job satisfaction. In this regard, the pertinence of incentives to acknowledge the performance of the healthcare staff in order to promote dignified, professional working conditions is still under debate and deserves further exploration.29,30
Although this study has limitations inherent to the exploratory interventions where it is not possible to generalize the findings to draw definitive conclusions,31 the results allow us to identify the potential strengths and obstacles which must be addressed in order to scale up the strategy and could be applicable to other rural contexts. Sustainability will depend on two structural and organizational changes:
1) Establishment of a continuous quality improvement program for primary care in rural areas, including educational outreach visits as a priority in the routine functions of supervision teams, to promote the permanent training of healthcare personnel as well as teamwork;
2) Reinforcement of management for generating local networks through communication and partnership among levels of care, implementing the interprofessional approach.
It will also be necessary to incorporate new components promoting user participation in order to establish their joint responsibility in health care.











 nueva página del texto (beta)
nueva página del texto (beta)


