Perinatal depression (PDN), a depressive episode occurring during pregnancy or the first year postpartum, is a serious public health concern given increased morbidity risk for mother and baby. In Mexico, 4.6 million children live with mothers with clinically significant depressive symptoms.1 Prevalence of depressive symptoms in one sample of Mexican women was 16.6% during pregnancy and 17.1-20.0% postpartum.2
Perinatal depression can be addressed,3 particularly when health system guidelines for detection and treatment of mental disorders are in place.4 In Mexico, however, the likelihood of adults receiving mental health services is poor. On average fourteen years pass from an adult's first onset of a mood disorder like major depression to initiating treatment, in Mexico.5 Mexican women 18-29 years are the age group least likely to receive needed mental health services, suggesting a lack of guidelines to address mental health care for reproductive age women.6
Here we aim to describe national and regional prevalence of mental healthcare and of existence of protocols or guidelines for detection and care of depression during or after pregnancy within public obstetric units in Mexico.
Materials and methods
A probabilistic, stratified sampling design was used to select a representative sample of 926 public (Ministry of Health, ISSSTE, IMSS, IMSS-Oportunidades) health care units across primary, secondary, and tertiary care throughout Mexico. A sub-sample of 211 secondaryand tertiary-level hospital obstetric units (excluding general hospitals) representative at the national, regional and urban/metropolitan level were selected. After signing informed consent, either the obstetrics and gynecology (OBGyn) lead physician/surgeon or OBGyn unit chief were interviewed in-person using a structured questionnaire (applied with a portable computer) to assess the following three issues:
Are mental health care or counseling services offered?
Are there any protocols or guidelines for the detection of depression during or after pregnancy?
Are there any protocols or guidelines for the care of depression during or after pregnancy?
Unit directors provided information on the number and profession of healthcare providers in the unit. The study, conducted from August to October 2012, was approved by the ethics committee of the National Institute of Public Health.
Response options for the three questions assessing the context of mental health services were: "yes", "no", "I don't know". Adjusting for survey design and sample weights, we used percentages and 95% confidence intervals and explored differences between geographic and urban/metropolitan regions using chi2 tests. Using Stata v.13.0 we compared average mean number of providers in units with and without mental healthcare or PND detection and care guidelines/protocols, with statistical significance at 0.05 or lower (StataCorp).
Results
In Mexico, 64.0% of public obstetric units offer mental health care while 37.1 and 40.3% of units have protocols or guidelines for detection or care of PND, respectively (Table I). Almost all (96.7%) obstetric units in Mexico City and adjacent Mexico State offered mental health care and higher percentages of units had protocols/guidelines for detection and care of PND. In contrast, mental health care was offered by under 50% of units located in the southern region of Mexico (p<.05). Southern Mexico had the lowest percentage of units with protocols/ guidelines for PND detection (26.5%), followed by Northern (27.3%) and Central Mexico (50.0%) and finally the Mexico City-Mexico state region (76.7%). The North had the smallest percentage of units with protocols/ guidelines for PND care (28.1%).
Table I Percentage and 95% confidence intervals of public obstetric units* with (1) Mental health care, (2) protocols or guidelines for PND detection, (3) protocols or guidelines for PND care by region and population size. Mexico, 2012
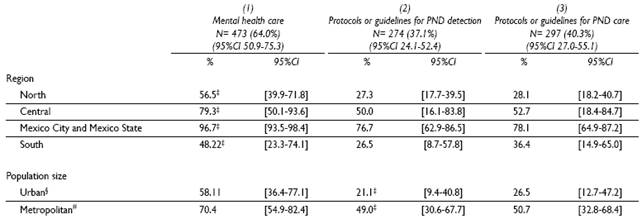
* 211 surveyed obstetric care units (secondary and tertiary level)
‡ p<.05
§ Population size = 2 500 to 99 999 inhabitants
# Population size = 100 000 or more
PND: perinatal depression
A higher percentage of units in metropolitan areas offered mental health care (70.4 vs. 58.1%) and had protocols/guidelines for the detection of PND (49.0 vs. 21.1%) and care for PND (50.7 vs. 26.5%), as compared to urban areas.
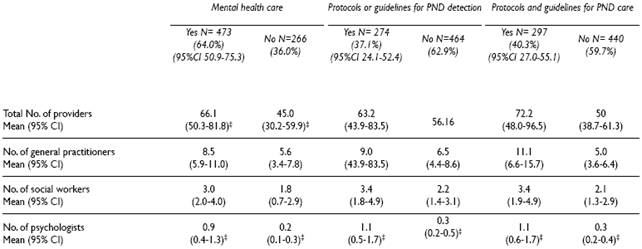
There were a significantly higher total number of providers in units offering mental health care than in those that did not (66.1 vs. 45.0) (Table II). Likewise, there was a significantly higher number of psychologists in units reporting provision of mental health care (0.9 vs. 0.2) and use of protocols/guidelines for PND detection (1.1 vs. 0.3) and care (1.1 vs. 0.3), compared to units without.
Discussion
These findings indicate the need for implementing institutional support for systematic detection and treatment of PND. A brief twoto three-question screening tool can be useful and feasible for initial screening protocols in both antenatal and postnatal periods.7,8 If a woman's score exceeds an established threshold, appropriate care pathways should be activated, including referral to mental health clinicians.
Although our results suggest investing in increasing the number of psychologists in obstetric units, there might not be enough trained psychologists to cover existing needs.9 Non-clinical personnel who deliver non-pharmacological interventions in low-resource settings can be successful in reducing symptoms of perinatal mental health problems. Activities such as home visits, empathic listening, and cognitive-behavioral techniques carried out by community health workers have successfully demonstrated a decline of depressive symptoms among women.10 Feasibility of implementation of such strategies in Mexico should be explored. A psycho-educational intervention to prevent postnatal depression among high-risk women was implemented in one public-sector hospital in Mexico with results suggesting participants in the intervention group had a larger reduction of depression at 6 weeks and 4 to 6 months postpartum compared to participants receiving usual care.11 Public and facility-specific policies that support these and other PND interventions are needed.12
This study's main strength is the nationally representative sample of obstetric units, allowing generalization of results to inform national policy. The main limitation is that the questions addressed the infrastructure for detection and treatment for PND, not the actual interventions themselves. Future research is needed to elucidate detection and care procedures in primary level units and other specialties such as pediatrics, as well as to evaluate pilot studies testing stepped-care protocols and community-based interventions. Because of PND's extensive negative consequences on women and infants' health, its detection and care warrant major public health initiatives.











 nueva página del texto (beta)
nueva página del texto (beta)