Cervical cancer mortality is a reflection of social inequity in health care. Globally, 266,000 women die from cervical cancer annually, and 85% of these deaths occur in low- and middle income countries (LMIC).1,2 Persistent infection with high-risk human papillomavirus (hrHPV) is a necessary cause of cervical cancer.3,4 HPV16 and HPV18 are responsible for 70% of squamous cell carcinomas, and in conjunction with HPV45, cause 94.2% of cervical adenocarcinomas.4
The introduction of HPV vaccines will change the epidemiology of HPV-related cancers. However, it may take 30 years to observe the desired benefits of widespread vaccination when vaccinated cohorts reach the peak ages at which cervical cancer cases currently occur (e.g. women aged 40-50 years).5 As of August 2015, 84 countries and territories had national public-sector HPV immunization programs and 38 had pilot programs.6 These programs mainly target adolescent girls to obtain the greatest cost-benefit ratio,7 considering the initial price of the vaccine (>$100 US per dose).8,9 Women older than age 25 are also vulnerable to new HPV infections10 and could also be vaccinated depending on country-specific resource availability.
Recent results of Phase III HPV vaccination trials documented that the vaccine's efficacy among adult women is excellent (efficacy >80% to prevent resultant HPV-related cervical intraepithelial neoplasia).11,12 Additionally, current vaccines protect against both HPV16 and HPV18 as well as provide cross-protection against other HPV types, particularly types 31 and 45.13 Broad-spectrum protection such as this may lower the need for subsequent screening, warrant longer screening intervals than those currently used, and offer novel prevention policies against HPV-related cancers. The combination of vaccination and screening strategies to prevent cervical cancer may be particularly appropriate in countries with high incidence of cervical cancer that have already implemented hrHPV-based screening programs. These criteria are satisfied in Mexico. A broader age range of females in population-based HPV vaccination programs could have direct benefits for vaccinated females, and indirect benefits for non-vaccinated females and male sexual partners via increased herd immunity to reduce HPV-related cancers.14
Based on the high efficacy of the HPV vaccine in older women, a novel strategy combining vaccination and screening, HPV FASTER, has been proposed.15 In accordance with this proposal, HPV vaccination of women in a broad age range can offer protection to women who are not currently infected, but also can protect against subsequent re-infection.15 As a result, a combined strategy of HPV vaccination and screening may reduce the lifetime number of screens used by the current hrHPV-based screening programs. If a screening and vaccination strategy is widely adopted, we expect promising results. This strategy has the potential to: 1) mitigate the screening demand on both women and health services by extending screening intervals; 2) improve the cost-benefit balance of screening programs; and 3) provide greater protection and quality of life to a large number of women through a reduction in cervical cancer.16 An intervention such as this may not only save many lives in the next 30 years but also be cost-effective.
However, the data on efficacy of HPV vaccination in older women to reduce cervical cancer risk, and not just the risk of precancerous lesions, are lacking. That is, there is currently insufficient knowledge regarding the role of HPV vaccination in older women to permit screening intervals to be extend safely following a negative screen (figure 1).
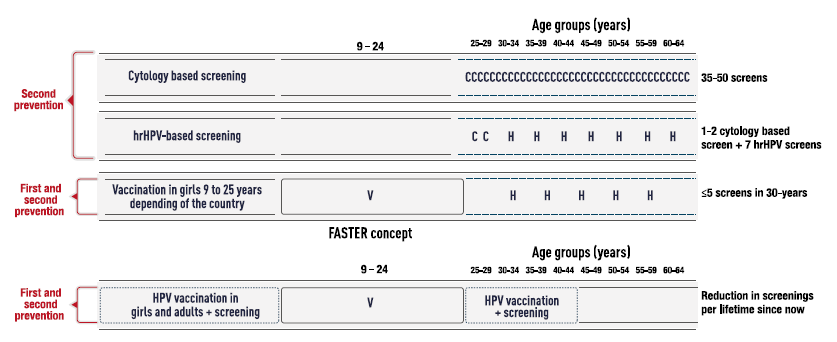
The figure shows exemplary cervical cancer prevention strategies based on cytology, HPV testing, and HPV vaccination with the effective total number of screens among screen-negative women per lifetime. Modified from Schiffman M, Wentzensen N. Human papillomavirus infection and the multistage carcinogenesis of cervical cancer. Cancer Epidemiol Biomarkers Prev. 2013; 22(4):553-60.9
Figure 1 Evolution of cervical cancer prevention
A significant challenge for HPV-vaccine uptake is the number of doses in the standard vaccine schedule. Although licensed in some countries for use among older individuals, national HPV vaccination programs target teenagers and young adults. Recent studies found that fewer than three doses of the two commercially available prophylactic HPV vaccines seem to provide similar protection against cervical HPV16 and HPV18 infections as the three-dose schedule in women younger than 25 years old. 17,18
Herein we propose a population-based study to assess the efficacy of a 2-dose HPV vaccination with [HPV16/18 AS04-adjuvanted vaccine (Cervarix (r)) and HPV 6/11/16/18 vaccine (Gardasil(r))] against HPV-persistent infection and HPV-related cervical disease in older women between 25 and 45 years of age attending clinics for hrHPV-based screening.
Primary objectives
To evaluate the impact of HPV vaccination in a hrHPV-based primary screening program to extend the screening interval from five to ten years.
Secondary objectives
To evaluate the efficacy of the HPV16/18 AS04-adjuvanted vaccine (Cervarix(r)) and HPV6/11/16/18 vaccine (Gardasil(r)) to prevent incident 6-month persistent infection of HPV16 or HPV18 over a ten-year study period, measured every 30 months after baseline hrHPV-based screening in women aged 25-45 years.
To evaluate the efficacy of the HPV16/18 AS04-adjuvanted vaccine (Cervarix(r)) and HPV6/11/16/18 vaccine (Gardasil(r)) to prevent incident histologically confirmed cervical intraepithelial neoplasia of grade 2 or higher (CIN2+) 5 and 10 years after baseline hrHPV-based screening in women aged 25-45 years.
To estimate the cost-effectiveness and associated cost reductions within the cervical cancer prevention program following implementation of a combined strategy of HPV vaccination and hrHPV-based primary screening program.
Materials and methods
Endpoints
We consider two main endpoints, a 6-month persistent infection as a surrogate of cervical intraepithelial neoplasia and CIN2+ occurrence at 5 and 10 years following baseline according to the following definitions:
6-month persistent infection (Time Frame: At month 30, 60 and 90 after baseline screening)
Occurrence of 6-month persistent infection of HPV16/18 every 30 months over 10 years of follow-up. [6-month HPV16/18 persistent infection defined as the detection of the same HPV type(s) assessed in urine samples at two consecutive evaluations over an interval of 6 months.].
Occurrence of 6-month persistent infection of hrHPV types (alone and as groups) excluding HPV16/18, every 30 months over 10 years of follow-up, [6-month high risk persistent infection defined as the detection of the same HPV type(s) assessed in urine samples at two consecutive evaluations over an interval of 6 months.].
CIN2+ occurrence (Time Frame: At month 60 and 120 after baseline screening).
Vaccination/screening strategy efficacy against CIN2+ according to vaccine administered (either Cervarix(r) or Gardasil(r)) [CIN2+ histological confirmed lesions].
Hypotheses
The combined strategy of HPV vaccination (Cervarix(r) /Gardasil(r)) and hrHPV-based screening can safely extend the interval between screenings from 5 to 10 years.
The efficacy of the combined HPV vaccination and hrHPV-based screening of women DNA-negative for hrHPV aged 25-45 years to prevent incident 6-month persistent infection of HPV16/18 at intervals of 2.5 years is above 80%.
The efficacy of the combined HPV vaccination and hrHPV-based screening of women aged 25-45 years to prevent the occurrence of CIN2+ lesions is above 95% at five years of follow-up.
Study design
This study consists of a randomized, non-blinded trial with three parallel groups that will be conducted in one primary health care center in Mexico City. The overall design is shown in detail in Fig. 2. Eligible participants will be assigned with equal probability to one of the three comparison groups: 1) hrHPV-based screening and HPV16/18 L1 VLP AS04 vaccine (Cervarix(r)) group according to a two-dose schedule (0-12 months); 2) hrHPV-based screening and Quadrivalent Human Papillomavirus (Types 6, 11, 16, 18) (Gardasil(r)) vaccine group according to a two-dose schedule (0-12 months); and 3) Control group who will receive only hrHPV-based screening.

Notes. The cervical cancer screening at month 60 will be performed in participants from both HPV vaccine arms who have been randomized to 5 years screening visit. The 6-month persistent infection assessment at month 60-66 will be carried out in participants assigned to 10 years screening visit.
Figure 2 Study design
Duration of the study for each participant: 120 months.
Study population
Women aged 25 to 45 years, living in the borough of Tlalpan, Mexico City, attending the Jurisdiction No. 8 of Healthcare services in Mexico City. For the present study, we plan to enroll 18,000 women of the target age group over a period of 18 months.
Inclusion criteria:
Female aged 25 to 45 years at the time of the first vaccine dose.
Willing to comply with the requirements of the protocol (e.g., return for follow-up visits).
Written informed consent prior to enrollment.
Exclusion criteria:
Pregnant or breastfeeding. Women must be at least 3 months post-pregnancy and not breastfeeding to enter the study.
Planning to become pregnant or planning to discontinue contraceptive precautions during the first twelve months of the study (months 0-12).
History of allergic disease, suspected allergy or reactions likely to be exacerbated by any component of the vaccine.
Any other medical condition or disease that could compromise the life of the participant during enrollment in the study.
Use of any investigational or non-registered product (drug or vaccine) other than the study vaccines within 30 days prior to the first dose of the study vaccine.
Previous vaccination against human papillomavirus.
History of cervical cancer or hysterectomy.
Setting
Tlalpan is one of the 16 administrative boroughs of the Federal District of Mexico City. This borough, which is comprised of 21 primary health care centers,19 is covered by the public healthcare services of Mexico City and is organized by the sanitary jurisdiction number 8.
In the 2010 Mexican national census, the borough of Tlalpan had a population of 650,567, of which 338,428 were women and 106,797 of whom were aged from 25 to 45 years, comprising the target population for this research study.19 The borough of Tlalpan has 144 neighborhoods. Study participants will be recruited from the population attending the health care center Dr. José Castro Villagrana, which has a target population of approximately 32,000 women. This center is responsible for clinical care and community health activities, offering preventive health care services, including cervical cancer screening.
Study procedures
The target population of the health care center will be randomly assigned into three arms: 1) HPV16/18 vaccine and hrHPV-based screening; 2) the HPV6/11/16/18 vaccine and hrHPV-based screening; and; 3) the control arm (hrHPV-based screening), as illustrated in figure 2. We estimated a balanced age distribution, with approximately 51% of participants in the 25-34 year stratum and 49% in the 35-45 year stratum.
As part of the regular care offered by the cervical cancer-screening program, women between 25 and 45 years of age will be invited to participate in the study. A detailed description of the study will be provided before consent.
At each screening visit (months 0, 60 and 120), a set screening format will be administered to the participant through an interview with a doctor or nurse from the health center to collect data pertaining to demographic information, smoking habits, past and current sexual history and reproductive status.
Vaccination
According to the study design, the control group will not receive the HPV vaccine. The two remaining groups will receive one of the study vaccines:
- HPV16/18 L1 VLP AS04 vaccine (Cervarix(r)) group according to a two-dose schedule (0-12 month). This group will receive the HPV16/18 vaccine containing HPV16 and HPV18 L1 virus-like-particles (20 μg of each) adjuvanted with 50 μg 3-O-desacyl-4'-monophosphoryl lipid A and 0.5 mg aluminum hydroxide (GlaxoSmithKline Biologicals, Rixensart, Belgium). A 0.5-mL dose of the vaccine will be administered in the non-dominant arm.
- Quadrivalent Human Papillomavirus (Types 6, 11, 16, 18) (Gardasil(r)) recombinant vaccine according to a two dose schedule (0-12 month). This group will receive amorphous aluminum hydroxyphosphate sulfate adjuvanted quadrivalent HPV (types 6, 11, 16, 18) L1 VLP vaccine (Merck Sharp & Dohme Corp. Whitehouse Station, NJ, USA). A 0.5-mL dose of the vaccine will be administered in the non-dominant arm.
During the baseline hrHPV-based screening visit, all participants in the intervention group will receive the first dose of either vaccine (figure 2). The administration of the vaccine will be in the area assigned by the staff of the health center, and preferably carried out by the nursing staff. After the vaccine administration, the patient will proceed to the doctor's office to continue the study procedures; any immediate post-vaccination adverse reactions will be recorded. Women who have received the first dose of either vaccine will be offered a second dose at month 12 to complete the vaccination protocol (figure 2).
hrHPV-based screening procedures
For all participants, a doctor or nurse properly trained in cervical sampling will perform a pelvic exam to obtain a cervical sample, which will be collected using the sampling device provided and transported in a vial with transport medium. This sample will be used for hrHPV testing including HPV 16/18 typing. All hrHPV positive women will have a reflex triage testing with cytology.
The cervical specimens will be delivered to the laboratory on a weekly basis and will be processed within one week. All HPV testing procedures will be centralized at the reference HPV laboratory at the Public Health Laboratory of Mexico City. All cervical specimens will be evaluated for hrHPV using a clinically validated test for the detection of 14 hrHPV types and to identify HPV types 16 and 18.
As part of the triage tests, a cytology evaluation will also be performed on all hrHPV-positive cervical specimens. Cytology slides will be prepared at one central cytology laboratory; slides will be prepared with either a conventional Pap or liquid-based cytology (depending on the availability of resources). We will use the Bethesda 2001 criteria for the diagnostic classification of standard cytology.
All results of the hrHPV testing, as well as all molecular and cytological triage results, will be available within 60 days. The staff responsible for the program in the health center will report the results to every participant.
All women with positive triage results for HPV16, HPV18 or atypical squamous cells of undetermined significance or worst (ASCUS+) will be referred for a colposcopy for further evaluation and treatment if necessary.
Women in the control group will be scheduled for a gynecological examination to collect cervical samples for hrHPV-based screening at five and 10 years (according to the routine five-year screening interval in the local practice) after the baseline screening following the same procedures described above. The two arms who were vaccinated (HPV vaccine/screening) will be randomized again before the programed screening at year five. Hence, each of the two vaccine arms (Cervarix and Gardasil) will be randomized within the arms into two arms comprised of equal numbers of women. Therefore, after the second randomization, four groups will be formed: 1) women who received Cervarix(r) that have to follow the routine five and 10 year screening interval; 2) women who received Gardasil(r) that have to follow the routine five and 10 year screening interval; 3) women who received Cervarix(r) that will receive the HPV screening at year 10; and 4) women who received Gardasil(r) that will receive the HPV screening at year 10. Figure 2 also shows the randomization of the two vaccine arms to evaluate the possibility of extending the screening interval for HPV.
Diagnosis confirmation and management
All women with a positive triage test at baseline, at the five-year screening, and at the 10-year screening will be referred to colposcopy evaluation for diagnosis confirmation and treatment if necessary. All women will have a systematic collection of cervical biopsy (at least one per quadrant) from the most significant abnormal areas, and an endocervical sample will be collected (with Rovers(r) EndoCervex-Brush(r)). Colposcopists will undergo training prior to the beginning of the study in order to standardize procedures.
Histological reports on biopsy and excision specimens will be used to classify the findings, following the Mexican Official standards for cervical cancer diagnosis. Two pathologists will conduct a histological evaluation of all samples (biopsies and/or endocervical samples). If both results are the same, this will become the final diagnosis, otherwise a third pathologist will review the specimen. If the third pathologist agrees with one of the two first pathologists this will be the final diagnosis. Remaining discrepancies will be solved by consensus by expert international pathologists who will review digital images of the slides.
Participants will receive appropriate treatment according to histological results; CIN2, CIN3 will be treated by conization, while invasive squamous cancer or adenocarcinoma will be referred for cancer management.
Assessment of 6-month persistent infection
All participants will have a urine collection sample at entry (visit 1) in order to validate a PCR-based urine assay by comparing detection and genotyping of human papillomavirus (HPV) DNA in urine samples and matching cervical specimens of women. The validation of the assay and procedures will then be used to decide on the future components of the plan to the assessment of 6-month persistent infection.
Assuming validation of HPV DNA detection in urine samples, all participants will have a urine collection sample at Month 30, 36, 84 and 90 to assess the prevalence of hrHPV infection and 6-month HPV 16/18 persistent infection. Additionally, the two vaccinated arms receiving the HPV screening at year 10 will have an extra urine collection at month 60 and 66 (figure 2).
Urine samples will be collected for molecular identification of hrHPV and genotyping of the 14 high-risk viral types individually. All urine-based testing will be centralized at the National Institute of Genomic Medicine (INMEGEN). The procedures of urine sample collection as well as DNA extraction and HPV DNA detection will be described more fully in future manuscripts after validation of the urine-based HPV DNA detection method.
The urine samples will be used only for surveillance; therefore, the results will not be provided to the study participants and the results will not be used for clinical decisions.
Safety stopping rules
One important aspect of the study is to assess the safety of women undergoing an extended screening interval from five to ten years with the combined strategy of HPV vaccination (Cervarix(r) /Gardasil(r)) and hrHPV-based screening. In order to demonstrate with a high level of confidence that the combination of HPV vaccination and hrHPV-based screening has a clinically acceptable safety profile to extend the routine five-year screening interval to 10 years, three criteria need to be met in the two intervention arms screened at five years:
No cases of invasive cancer diagnosed.
Less than 10% of histologically confirmed CIN2/3 cases detected in vaccinated arms compared to cases found in non-vaccinated arm.
If these criteria are met, the combined strategy of vaccination and screening every 10 years will be considered safe and warrant study continuation. Otherwise, the study will be suspended at five years of follow-up and immediate screening will be offered to all participants.
Statistical considerations
Efficacy trials for the prevention of cervical cancer precursors have already documented the efficacy of HPV vaccination for women older than 25 years.11,12 The aim of the present study is to document the benefit of a massive HPV vaccination program within a cervical cancer-screening program to extend the HPV screening interval from five to 10 years through the prevention of 6-month persistent infection as well as the prevention of CIN2+ incidence.
As observed in the Viviane Study,11 the annual attack rate of HPV16/18 6-month persistent infection in women aged 36-45 years in the control group was 0.44%. Therefore, it is expected that the overall attack rate in our population of women aged 25-45 years will be at most the same as the attack rate observed in the 36-45 years strata of the Viviane study considering that the attack rate for persistent infection diminishes with age.20
Hence, for the primary virological objective, we intend to target a sample size of approximately 3,000 enrolled participants in the older age stratum, which should yield 2,627 evaluable participants, assuming a non-evaluable rate of 20% and an annual attack rate of 0.44% for HPV 16/18 6-month persistent infection. Based on these estimates, we proposed sample sizes of 3,000 by age stratum with 80% power to show 80% vaccine efficacy against the primary endpoint 6-month persistent infection of HPV16/18. The sample size was computed using the GPower Statistical Power Analyses.
Study vaccines safety
HPV vaccines are approved for use in more than 100 countries, with more than 190 million doses distributed worldwide. Extensive clinical trials and post-marketing safety surveillance data indicate that both Cervarix(r) and Gardasil(r) are well tolerated and safe. The main side effects of the vaccines are local reactions at the injection site (pain, redness and swelling), which occur in approximately 80% of vaccine recipients. Meta-analyses on pooled data from multiple clinical trials on both HPV vaccines have shown no increase in the risk of serious adverse events among vaccine recipients compared with control/placebo recipients.21,22
Given that in Mexico, both HPV vaccines, Cervarix(r) and Gardasil(r), are commercially available and are approved for use in females older than 9 years old (up to 45 for Gardasil(r) vaccine), safety assessment is not an objective of this study.23
The health care centers are responsible for the notification of adverse reactions that may occur after the vaccine administration, according to the local regulatory authority. Each participant will be instructed to contact the health care center immediately if they show any signs or symptoms perceived as serious. In those cases, the standard notification form "Formato para el aviso de sospecha de reacciones adversas de los medicamentos" should be completed and sent to the Centro Nacional de Farmacovigilancia.
Ethical aspects
Applicable standards: The trial will be conducted according to the Declaration of Helsinki and Good Clinical Practice.
The proposal will be submitted to the IRB of the National Institute of Public Health, the Research Committee of the Servicios de Salud de la Ciudad de México, and the Federal Commission for the Protection against Sanitary Risk (COFEPRIS).
All participants will provide written informed consent prior to the performance of any study-specific procedures.
We will ensure protection of data privacy and respect of medically sensitive data of study participants.
The research and ethics committees of the National Public Health Institute and the Distrito Federal Ministry of Health will review the protocol and provide final approval. We will register the protocol with the International Committee of Medical Journal Editors (ICMJE) as well as in ClinicalTrials.gov.
The procedures described in this protocol comply with the ethical principles for medical research involving human subjects laid out in the 1989-amended version of the 1975 Declaration of Helsinki, and with the laws and international standards for good practice in clinical research.
As previously mentioned in the methods section, stopping rules will be applied in this trial. Women will be informed that they have the opportunity to be vaccinated after the completion of the trial or interruption of the trial if they had been assigned to the control arm.











 nueva página del texto (beta)
nueva página del texto (beta)


