Central nervous system (CNS) tumors in adults are the tenth leading cause of estimated new cancer cases and the twelfth leading cause of death worldwide, 1 with an estimated 22 850 new cases and 15 320 deaths in 2015. 2 In the United States, CNS tumors contribute to one of the highest cancer incidence rates. 3 Their degree of malignancy is variable, and although some tumors are classified as benign, the majority are often lethal due to their capacity to infiltrate tissues and to cause malignant transformation over time, 4 causing progressive neurological deficit, motor skill loss, headaches, mental impairment and seizures. 5-8
In Mexico, the epidemiology of CNS tumors is uncertain, as the majority of studies evaluating their frequency include a limited number of cases or focus on specific types of tumors. 9,10 As a result, these cases are not representative of the general population, which makes comparisons with international epidemiological studies difficult. Various studies that describe the frequency of CNS tumors in various hospital settings throughout the country exist, with results published in regional journals. However, they do not provide a comprehensive epidemiological understanding of these tumors. Two prior studies on CNS tumor frequency were conducted in the National Institute of Neurology and Neurosurgery Manuel Velasco Suárez, Mexico (Instituto Nacional de Neurología y Neurocirugía de México, INNN). 9,11 However, neither of these studies analyzed study periods that were as long as that evaluated in the present study. The 1997 Mohar and colleagues study on the distribution of malignant tumors seen in the Mexican National Cancer Institute from 1985 to 1994 reported that nervous system tumors were the 13th most common cancer. 12 However, in Mexico, these tumors caused 2.6% of cancer-associated deaths in 200013 and were the leading cause of head and neck cancer deaths. 14
The exact frequency, age and gender distribution, as well as trends in CNS tumors, in Mexico are unknown. This lack of information makes it difficult to provide inferences about the etiology, the associated risk factors and the magnitude of the health problem that these diseases cause for the purpose of establishing appropriate public health strategies.
The present study analyzes a large number of CNS tumor cases over a period of fifty years in the INNN, a reference hospital center in Mexico where this type of cancer is one of the leading causes of morbidity and mortality. 15 Here, we describe the types of CNS tumors and the age and gender distributions of patients with CNS tumors and estimate their relationship with surgical discharges over the last 20 years to understand trends in this cancer over time.
Materials and methods
Study design
This was a descriptive and retrospective study. Data on CNS tumor frequency were obtained from records from 1965 to 2014 that existed in the clinical records of the Pathology, Neurosurgery and Epidemiology Departments (files) of the INNN. These records contained information on patients' demographics, histological diagnosis and clinical characteristics, and the consistency of information contained within them was corroborated.
CNS tumors were grouped based on the existing international classifications from 1965 to 2014, as follows: 1) Bailey and Cushing16 (from 1965 to 1978), which included tumor histogenesis and took into account tumor types, such as medulloblastoma, astroblastoma, ependymoma and spongioblastoma (subsequently referred to as glioblastoma multiforme); 2) Zülch17 (from 1979 to 1992), whose grouping considered criteria related to the prognostic evaluation of cases; and Kleihues and colleagues18 (from 1993 to 2014), a categorization that introduced immunohistochemistry into the diagnosis and in which the tumor types identified by Bailey and Cushing as gliomas were distributed into specific groups. CNS tumors were identified based on the 2007 World Health Organization (WHO) classification of tumors of the central nervous system, 19 except for gliomas, pituitary adenomas (which are currently considered in an independent classification) and metastatic tumors.
Men and women aged 15 to 96 years with a confirmed histopathological diagnosis of CNS tumor who had a complete clinical record were included in the study. Cases of patients with recurrent cancer were excluded.
The INNN Research and Ethics Committee approved the present study. The data obtained from clinical files were treated with utmost confidentiality, preserving the patients' right to privacy.
Statistical analysis
CNS tumors identified between 1965 and 2014 were grouped according to the 2007 WHO classification of CNS tumors, and their relative frequencies were determined. Subsequently, CNS tumor frequencies were analyzed in three periods, according to classifications used from 1965 to 2014, and the percentages were compared using the Chi square test to identify differences between the proportions.
The distribution of CNS tumors was described by both gender and age quintiles from 15 to 79 years, including an extra category for subjects aged 80 years and older. Age group stratification was created using equidistant categories, 20 which included the wide spectrum of ages at tumor presentation. The incidence rate of tumors of neuroepithelial tissue from 1995 to 2014 was analyzed, and the annual proportions of CNS tumors and overall surgical discharges (CNS tumors/SD) and their 95% confidence intervals were arbitrarily calculated from 1995 to 2014 using surgical discharge records dating back to 1995. This information was coded and included in a database for analysis using the Statistical Package for the Social Sciences (SPSS version 20, IBM Corp. Armonk, NY.).*
Results
Between 1965 to 2014, 16 116 patients with CNS tumors were treated in the INNN. However, 3 320 of those patients had recurrent tumors, an uncertain diagnosis or an incomplete clinical record and were excluded from the study.
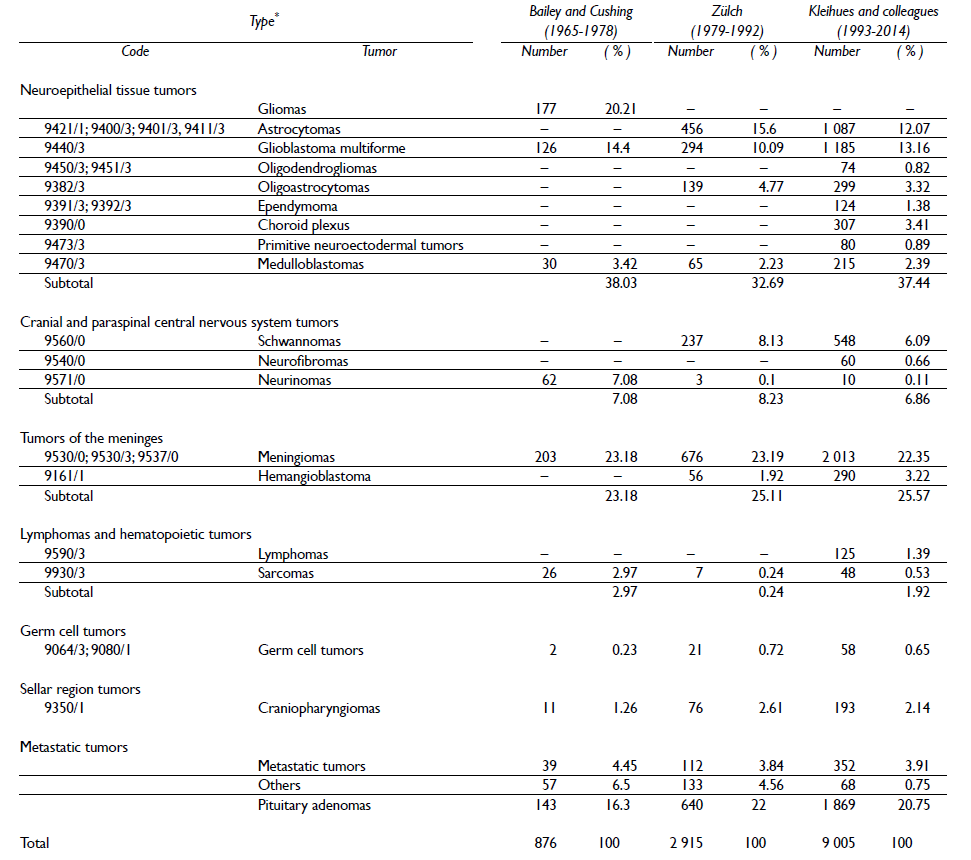
The most common CNS tumors were tumors of neuroepithelial tissue, followed by meningeal and pituitary tumors (figure 1). In the period from 1995 to 2014, the most common tumors of neuroepithelial tissue were astrocytomas (table I). With regard to age, neuroepithelial tissue, meningeal, pituitary, cranial nerve and lymphoid CNS tumors were the most common tumor types in the third and fourth decades of life, while germ cell and sellar region tumors were the most common tumor types in the second decade (figure 2).

Figure I Percent frequencies of central nervous system tumors in the Mexican National Institute of Neurology and Neurosurgery (1965-2014)
Table I Types of neuroepithelial tissue tumors seen in the Mexican National Institute of Neurology and Neurosurgery from 1993 to 2014

* Includes astroblastoma, choroid glioma of the third ventricle and angiocentricglioma
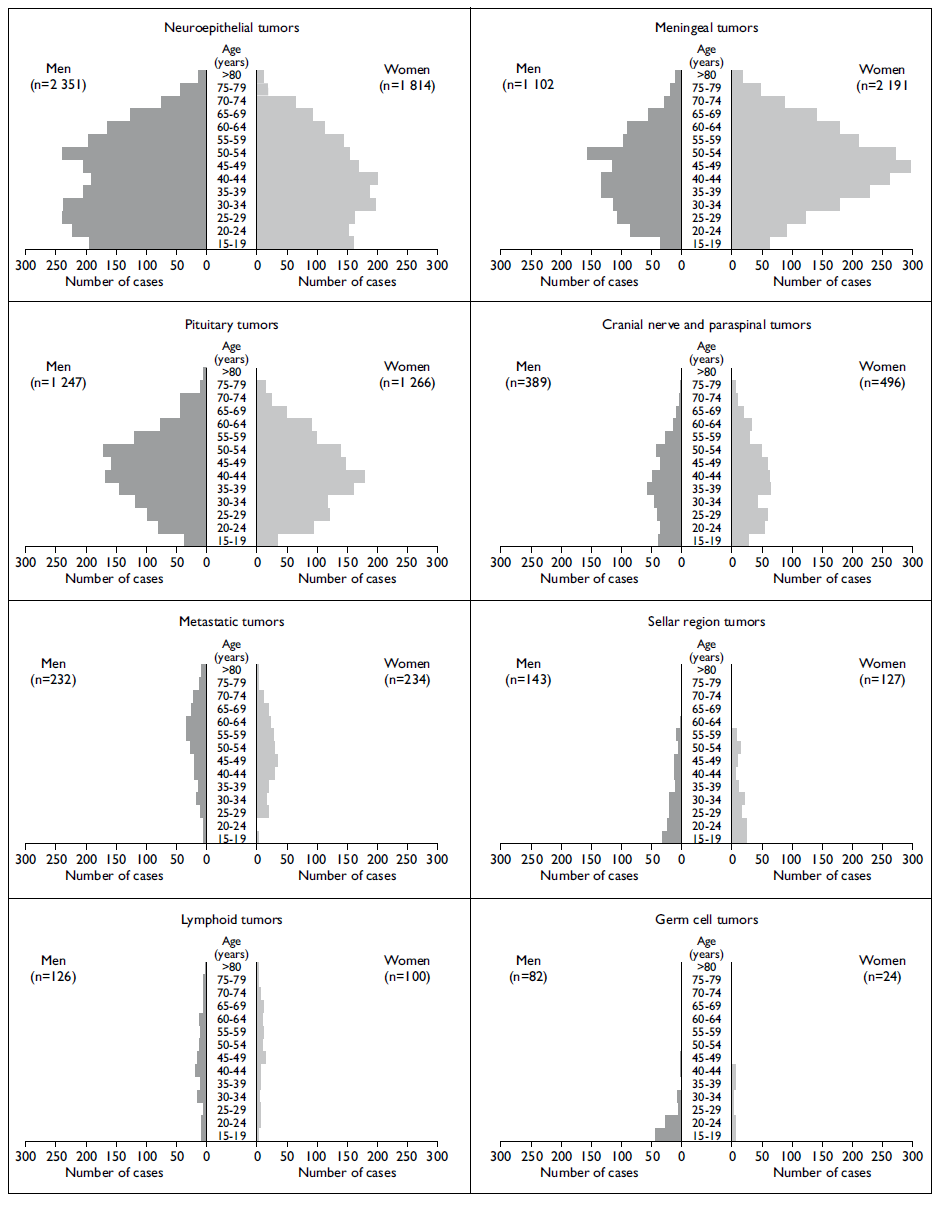
Figure 2 Age and gender distributions of central nervous system tumors in the Mexican National Institute of Neurology and Neurosurgery (1965-2014)
The frequency of CNS tumors was similar with regard to gender (women, n=6 633, 52.6%; men, n=5 977, 47.4%). However, there was an indication of gender predominance with specific tumors, including germ cell and neuroepithelial tissue tumors, which were more common in men than in women, while meningeal tumors were more common in women than in men (figure 2).
Throughout the periods 1965-1978, 1979-1992 and 1993-2014, there was an increase in the number of CNS tumors treated at the INNN (876, 2 915, and 9 005, respectively). With regard to the distribution of the main types of CNS tumors, statistically significant differences were observed in the three study periods (p < 0.001). The number of tumors in the "other" category decreased between the first (6.5%) and third (0.75%) periods (table II).
Table II Percent frequencies of central nervous system tumors from 1965 to 2014 in the Mexican National Institute of Neurology and Neurosurgery, grouped based on the Bailey and Cushing, Zülch, and Kleihues and colleagues classifications*
* The number that precedes the histological type corresponds to the existing classification code for nervous system tumors (WHO, 2007);19 which includes various new aspects that were not considered in previous classifications: Bailey and Cushing (1926),16 Zülch (1979),17 and Kleihues and colleagues (1993).18 In the WHO 2007 classification, pituitary adenomas are not considered to be CNS tumors, but rather pituitary tumors;19 gliomas do not have a classification number as a group, but rather as specific tumors within the group (9421/1; 9400/3; 9401/3, 9411/3, 9440/3,9450/3; 9451/3, 9382/3, 9391/3; 9392/3, 9390/0, 9473/3, 9470/3); and metastatic tumors do not have a classification number19
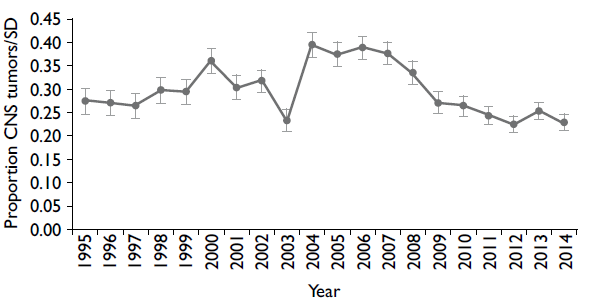
The annual CNS tumors/SD relationship calculated to compare the trend in tumor numbers was similar in the 1995-2014 period (0.22-0.39), although increases in the ratio were observed in two periods (one between 2000 and 2002 and the other between 2004 and 2008) (figure 3).
Discussion
The cases reported here represent the largest sample of CNS tumors analyzed in Mexico.
The number of CNS tumors seen in the INNN increased over time, although the CNS tumors/SD relationship did not considerably vary (figure 3). However, this increase does not necessarily reflect an increase in the incidence of CNS tumors in the general Mexican population, as this trend could be associated with a gradual increase in the number of patients treated at the institute, which is the largest national reference center for patients with neurological conditions. 21,22 Other factors, including the introduction of innovative diagnostic technologies in the 1970s and 1980s using computerized axial tomography and magnetic resonance23-25 and improvements in histopathological diagnosis and recording methods, could also explain the increase. 26,27
The frequencies of neuroepithelial tissue and meningeal tumors were similar to those reported in other countries. 28-31 However, the frequency of pituitary tumors in this study (20%) was two times higher than that reported in Austria, the United States and Egypt, where this tumor represented 8.9, 9.1 and 11% of CNS tumors, respectively. 32-34 This fact could be associated with ethnic factors, 35,36 geographical distribution37 and other risk factors. 38-40
The high frequency of germ cell tumors in the second decade of life was similar to that found in other studies. 41-43 In turn, sellar region tumors occurred in patients at younger ages than have been reported in other studies. 44,45
In general, CNS tumors were most often noted in women, a finding that has also been reported by other groups. 46,47 The predominance of germ cell and neuroepithelial tissue tumors in men and meningeal tumors in women agrees with results that have been previously reported. 48,49 This gender predominance could be attributed to sex hormones and genetic differences between men and women. 50
The differences in the distribution of CNS tumors in the three study periods are likely related to the lack of inclusion of lymphoma cases in the first two periods. The decrease in the frequency of tumors classified as "others" reflects a better categorization and knowledge of these tumors (table II).
In general, the low variability with regard to CNS tumors/SD from 1995 to 2014 suggests that the number of CNS tumor cases has not increased in recent years. However, it is necessary to conduct multicenter epidemiological studies that are representative of the Mexican population and that would allow for the incidence rates of these diseases to be determined.
The primary limitation of the present study is that its results cannot be extrapolated to the general Mexican population, in spite of the fact that the included patients come from various parts of the country. However, our results are noteworthy because the INNN is a neurological reference center in which 90 000 consultations are made yearly, 21 yielding a large number of CNS tumor cases, which is the first or second leading cause of morbidity and mortality in this population. 15
Our results reflect the technical and caregiving capacity of the INNN with respect to CNS tumors and contribute to the evidence regarding the frequency of CNS tumors in developing countries and in other similar hospital centers worldwide. Future studies regarding factors associated with CNS tumor development should be conducted in Mexico.











 nueva página del texto (beta)
nueva página del texto (beta)