Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Salud Pública de México
versión impresa ISSN 0036-3634
Salud pública Méx vol.57 supl.1 Cuernavaca 2015
Artículo original
Mortality and its association with chronic and infectious diseases in Mexico: A panel data analysis of the elderly
Mortalidad y su asociación con enfermedades crónicas e infecciosas en México. Análisis sobre adultos mayores con datos de panel
César González-González, PhD,(1) Alberto Palloni, PhD,(2) Rebeca Wong, PhD.(3)
(1) Instituto Nacional de Geriatría. México.
(2) University of Wisconsin, Madison. United States.
(3) University of Texas Medical Branch. United States.
Abstract
Objective. This study examines the relationship between chronic and infectious diseases on mortality risks under conditions of accelerated aging.The main hypothesis is that individuals who report both types of diseases experience higher mortality risks than those reporting only chronic diseases.
Materials and methods. We used a nationally representative sample of 12 128 individuals aged 50 years and over included in the three waves of the Mexican Health and Aging Study. We estimated Cox regression models to assess the combined effect of self-reported chronic and infectious diseases on subsequent mortality.
Results. In the period under study there were 2 723 deaths, 22.5% of the baseline sample. Having reported chronic and infectious diseases significantly increases mortality risks compared to having reported only chronic diseases.
Conclusion. In a context of socioeconomic inequality and a mixed epidemiological regime it is crucial to understand how diseases combine to generate excess mortality risks among the elderly.
Keywords: aging; mortality; chronic disease; infectious disease; longitudinal studies; Mexico.
Resumen
Objetivo. Se examina la relación entre el reporte de enfermedades crónicas e infecciosas y la mortalidad en un proceso de envejecimiento acelerado. El supuesto principal es que las personas que reportan ambos tipos de enfermedades son más propensas a morir que los que informan sólo enfermedades crónicas.
Material y métodos. Se utiliza información de las tres rondas del Estudio Nacional sobre Salud y Envejecimiento en México para estimar la mortalidad a través de modelos de riesgos proporcionales de Cox.
Resultados. Entre 2001 y 2012 se registraron 2 723 muertes, 22.5% de la muestra basal. Haber reportado enfermedades crónicas e infecciosas incrementa el riesgo de morir con respecto a aquellos pacientes que sólo reportaron tener enfermedad crónica.
Conclusión. En un contexto de desigualdad socioeconómica y un régimen epidemiológico mixto, es fundamental conocer cómo la combinación de enfermedades crónicas e infecciosas genera exceso de mortalidad entre adultos mayores.
Palabras clave: envejecimiento; mortalidad; enfermedades crónicas; enfermedades infecciosas; estudios longitudinales; México.
In most modern societies the elderly represent an un-precedentedly high fraction of the total population.1 Mexico is no exception to this rule. Before the year 2000 the population aged 60 years and older in Mexico never exceeded 7%, but the projected population for 2030 is expected to represent 17% and by 2050 its share of the total will have increased to about 28%.2 This accelerated change in the age structure will heighten the importance of safety nets and social welfare programs for the elderly increase the prevalence of chronic disease and disability and alter risk profiles due to exposure and behaviors. The interaction of these factors will influence time spent in illness and disability and old age survival.
In the last ten to twenty years chronic diseases have taken the lead as the main causes of death among the older population. Thus, in 2008 diabetes mellitus ranked as the most important cause of death among the elderly. It was followed by ischemic heart disease and cerebrovascular disease.3 Grouped together these three causes of death account for about a third of all deaths in Mexican older adults.
In contrast to conditions experienced in high income countries at comparable stages of the epidemiological transition, infectious diseases still play an important role in morbidity and mortality among elderly Mexicans. Thus, acute lower respiratory infections rank in 7th place among the leading causes of death and strike with particular virulence highly vulnerable groups such as the elderly, the less educated, and residents of rural areas.4 Influenza is one of the most prevalent infectious diseases in these subgroups, although many of the deaths associated with this disease are due to secondary complications that develop more frequently among the elderly, the poor and rural residents. Recent epidemics of Influenza are associated with increased hospitalizations and higher mortality due to complications such as congestive heart failure, chronic obstructive pulmonary disease, pneumonia and bacterial infections.5
The coexistence of a regime that combines chronic and infectious diseases is not a unique feature of Mexico; quite the contrary, it is generalized in low and middle income countries. These conditions are rooted in high levels of poverty, persistent malnutrition, unsanitary environments, and lack of access and use of modern medical care. This state of affairs departs from expectations held by proponents of various epidemiological transition models and is one that, as we document below, presents unique challenges to public health.6
Older adults in these mixed regimes are exposed to an increased risk of contracting chronic conditions but simultaneously experience higher susceptibility to infectious diseases, in part due to weaker immune function associated with aging and in part due to enhanced exposure to pathogenic environments. Although the jury is still out on this matter, we conjecture that the lethality of both chronic and infectious diseases increases in the presence of the other.7 There is abundant empirical evidence demonstrating that mortality risks associated with infectious diseases increase among older people due to diminished host resistance, delays in diagnosis, poor or inappropriate therapy and complications from chronic ailments.7
Thus there are three main paths through which infectious and chronic diseases may impact mortality in countries like Mexico. First, mortality due to infectious diseases in developed countries is relatively low compared to those in developing countries. In the latter, the influence of infections acquired during young ages may translate into higher mortality in old age due to chronic diseases. Second, in countries such as Mexico, uncontrolled infectious diseases prevail at ages 50 and older, which may cause mortality even without the influence of chronic diseases. Third, the co-existence of infectious and chronic diseases may have an impact on mortality above and beyond what would be expected from the previous two paths.
We use data from the Mexican Health and Aging Study (MHAS), the only source known to us of longitudinal, national level data about diseases and mortality among the elderly. These data enable us to assess mortality risks associated with the coexistence of chronic and infectious diseases over a period of about twelve years. Our conjecture is that those people who report having experienced infectious and chronic diseases at some point during the period of observation experience heavier mortality risks subsequently than those who do not experience diseases or experience only one of them.
Materials and methods
The MHAS is a three-wave panel prospective survey that began in 2001. A second wave was carried out in 2003 and a third follow-up and most recent interview took place in 2012. The main goal of MHAS is to retrieve information on the aging process with a rich socioeconomic perspective, and the impact of disease and disability in the population 50 years and older in Mexico. The sample is representative at the national and local level (100 000 inhabitants or more and under 100 000 inhabitants).8
A total of 15 402 individuals were interviewed in the first wave but our analysis uses information from a subsample of 12 411 individuals who were 50 years or older at the 2001 baseline and with complete interviews in 2001,2003 and 2012.
The dependent variable is defined as survival status in 2003 and 2012. Those interviewed in 2001 and still alive in 2012 were coded with 0 and those who died between 2001 and 2012 were coded with 1. The date of death (month and year) was obtained from a next of kin or proxy. We used this reported dates to calculate the total time of exposure to death risk.
The independent variables are taken from the 2001 baseline, and include seven self-reported chronic diseases. These are answers to the questions "Has a doctor or medical personnel ever told you that you had...": hypertension, diabetes, cancer, lung disease, heart attack, arthritis and stroke, as well as similar self-reports of three infectious diseases during the two years prior to each interview: liver or kidney infection, tuberculosis, and pneumonia. These are represented as dummy variables coded 1 if the respondent reported the presence of the disease and 0 otherwise. Additionally, to examine the combined effect of chronic and infectious diseases, we created a categorical variable of the two types of diseases, with the following categories: a) without disease; b) only infectious diseases; c) only chronic diseases, and d) with chronic and infectious diseases.
The information on diseases is self-reported as long as the individuals are alive, and from the next-of-kin respondents when the individuals have died. The next-of-kin interview gathers information on the last year of life of the deceased, including the report of diseases. Thus the strategy to measure the effect of diseases on mortality using the information from next-of-kin interviews may produce reporting errors and bias in the effect of diseases on mortality, but we consider this strategy as optimal given the data available from the MHAS.
Previous research demonstrates that the risk of death is related to demographic and socioeconomic variables,9 so we include controls for: age (continuous), sex, marital status (single, married or separated and widowed), education (continuous) and locality size (with the cut-off point in 100 000 inhabitants). These are measures from the baseline wave of 2001.
We used preliminary descriptive analysis to examine survival patterns by demographic and health characteristics. We compared groups using bivariate analysis and conventional Chi-square or Student's t-test statistics. We estimated Kaplan-Meier survival curves to compare survival times (in years) for individuals who self-report each of the seven chronic diseases identified above. We also computed log-rank statistics to assess mortality differences by self-reported diseases. We tested proportional hazards assumptions using a number of tests and then estimated effects of disease on mortality risks using standard Cox proportional hazard models.
Results
MHAS has a total 15 402 records at baseline and 3 288 deaths by the end of the follow-up period. After a selection process our analytical sample included 12411 subjects, representing 13 million Mexicans aged 50 years and older in 2001, and 2 723 individuals died in the considered period (2001-2012), representing around 24.2% of the initial population.
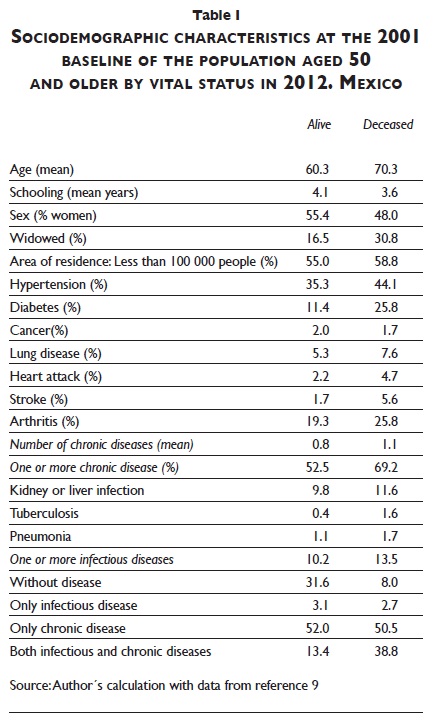
Table I displays the most important descriptive statistics for the sample. Compared to survivors, those who died during the 11-year period were older at baseline, had fewer years of formal schooling, and were more likely to be men and widowed. Two thirds of those who died had reported at least one diagnosed chronic disease at baseline, with hypertension (44.1%) and diabetes (25.8%) as the most prevalent ones. About 13.5% had reported the presence of at least one infectious disease, with liver or kidney infection being the most prevalent. Our analysis also reveals that among those who died 8.0% had reported no chronic or infectious disease, 2.7% had reported only infectious diseases and 50.5% only chronic diseases. Remarkably, 38.8% of those who died are reported to have both types of diseases, compared to only 13.4% among those who survived. This results show that those who are still alive at the end of the study reported better health, were younger, more likely to be women, and better educated than those who died (table I).
About 85% of those who died are reported to have experienced an illness as the principal cause of death (statistics not shown). Of these, in 18.6% cancer was the underlying cause, followed by diabetes (16.2%), stroke (5.6%), heart diseases (20.1%), and other causes (39.2%). The average age of death associated with each of these causes was 75.0 years for cancer, 73.3 for diabetes, 79.3 for stroke and 77.1 years for heart attack.
Estimated Kaplan-Meier survival functions for the seven self-reported chronic diseases considered in this study are shown in figures 1a and 1b. Three diseases stand out because of their substantial contribution to the mortality risk: cancer, heart attack and stroke, and all of these generate significantly different mortality patterns (log rank statistics tests not shown; p<0.001).
The first set of estimates from a Cox proportional hazards regression model are displayed in table II. This table includes estimates to assess the effects of specific chronic and infectious diseases. Those who reported having cancer (HR = 5.87), stroke (HR = 2.16) and diabetes (HR = 2.54) have the highest risk of dying. Regarding infectious diseases, liver or kidney infection (HR = 2.15) and pneumonia (HR = 1.79) have a significant effect on mortality. The results from the model show also that those with higher education and urban residents had a lower risk of mortality, while being a woman, older age and widowhood increased the risk.
Estimates in table III are for models including chronic and infectious diseases combined into a single variable. The estimates show that individuals with combined chronic and infectious diseases have a relative risk that is close to three times as high (HR = 3.09) the risk experienced by those who are reported to have a chronic disease only. Those who experience no illness have a mortality risk that is about one fifth (HR = 0.267) of those reported to have one chronic illness.
Discussion
Patterns of mortality in the presence of both chronic and infectious diseases is a relatively unexplored subject, particularly in vulnerable groups and among elderly in low to middle income countries. The simultaneous contraction of infectious and chronic diseases is a new feature of modern epidemiological regimes in these countries and is more likely to occur among the elderly, the poor and rural residents.9,10
Our results indicate that the joint occurrence of both chronic and infectious diseases increases significantly the risk of mortality among older adults. The sole presence of chronic disease implies by itself an elevated risk of death, but when combining it with an infectious disease this risk trebles. This result has important consequences for countries where infectious and chronic diseases coexist in an uneasy balance and is a rather persistent trait in the population. Mexico is a country with diverse and profound inequalities, high levels of poverty, uneven sanitary conditions and access to health services. If these economic and health conditions were to improve, a significant number of deaths could be prevented or at least postponed. About 60% of the elderly have at least one diagnosed chronic disease of the seven considered in this study (authors' own calculations with MHAS information). This burden of disease alone carries a steep penalty in term of mortality risks. But the penalty gets stiffer in the presence of infectious diseases. The presence of the two types of diseases in adverse social contexts, in societies with high levels of inequalities, and with persistent and highly diverse levels of access to health care, presents a unique public health challenge and is a threat to continuous improvements in longevity.
Despite significant past progress, Mexico is now experiencing an accelerated aging process with the parallel growth of prevalence of chronic conditions and disability that this entails. And yet it is also experiencing high levels of prevalence of infectious diseases particularly among the elderly.7,11 As we showed here, these patterns are consequential for mortality and the potential losses of survival gains at older ages. But the coexistence of chronic and infectious diseases is likely to also impact health and disability conditions of a nature and magnitude that cannot be even guessed from the past experience of higher income countries. These were not examined in this paper but we can only surmise that they could be as consequential if not more than the effects on mortality regimes.
Indeed, our results seem to indicate that the interaction of both types of diseases has an independent effect, in addition to the effect that each may exert on mortality. Hence joint interventions and programs may be justified for management, control and prevention of both types of diseases, as opposed to the traditional programs that address one or the other (chronic or infectious) alone.12
The number of older adults is increasing, and research has shown that the number of diseases increases with age,13 leading to a more intensive use of health care services. The current aging of the population in Mexico also represents a challenge for the socioeconomic and family systems, and in the near future health issues can complicate the situation even more.14
This study has shortcomings that can influence the validity of its conclusions. First, the panel has important attrition due to sample losses and non-response that we did not adjust for. Second, all information on illnesses is self-reported and not clinically confirmed. Third, we have no information on the order sequence of diseases when both types occur simultaneously. We suspect that the body's defenses, overload and recovery potential are different when chronic conditions precede the infection than vice versa. Finally, we are not able to discern between situations where the infectious conditions are a repeated rather than an episodic occurrence, confounding cases where the coexistence may be a more durable affair with those where it is only a transient feature of the course followed by a chronic condition.
Despite these limitations, this study has identified a little known phenomenon that could turn out to be highly consequential in aging populations around the world, and contributes to the design of further investigations that may expand the knowledge on the likely trajectory of the aging process for rapidly-aging developing countries like Mexico.
Aknowledgements
This work was supported by the National Institute on Aging at NIH [grant R01AG025533]. Data for this study comes from the Mexican Health and Aging Study (MHAS), also funded by the National Institute on Aging (R01 AG018016). César González-González is supported in part by a grant from CONACYT/INEGI [ID # 186319]. Alberto Palloni's research is supported by other grants from the National Institute of Aging, the Fogarty International Center and the Robert Wood Johnson Investigator Awards in Health Policy [grants R01 AG016209, R37 AG025216, 5D43TW001586 and Research Grant ID # 67212]. Research at the Center for Demography and Ecology (CDE) and the Center for Demography of Health and Aging (CDHA), University of Wisconsin-Madison is supported by the NICHD Center Grant 5R24HD04783 and by NIA Center Grant 5P30AG017266. Rebeca Wong's research is supported by NIA/NIH (R01 AG018016) and by the Sealy Center on Aging at the University of Texas Medical Branch.
References
1. Satariano W. The aging of human populations: The significance of an epidemiologic perspective. Epidemiol Aging 2006:1 -38. [ Links ]
2. Consejo Nacional de Población. Proyecciones de la población de México 2005-2050. México: Conapo, 2011. [ Links ]
3. Dirección General de Información en Salud. Base de datos de defunciones generales 1979-2007 [sitio de internet]: Sistema Nacional de Información en Salud. México: Secretaría de Salud [consultado 30 de junio de 2013]. Disponible en: http://www.sinais.salud.gob.mx. [ Links ]
4. Muradas-Troitiño MC.Las causas de muerte de los adultos mayores en México: expresión de la desigualdad social. México: El Colegio de México, 2010:376. [ Links ]
5. Thompson WW, Shay DK,Weintraub E, Brammer L, Cox N, Anderson LJ. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA 2003;289(2):179-186. [ Links ]
6. Samper-Ternent R, Michaels-Obregon A Wong R, Palloni A. Older adults under a mixed regime of infectious and chronic diseases. Salud Publica Mex [serie en internet];2012;54(5):487-495. [ Links ]
7. YoshikawaT. Epidemiology and unique aspects of aging and infectious diseases. Clin Infect Dis 2000;(30):931-933. [ Links ]
8. Mexican Health and Aging Study (2013),The Mexican Health and Aging Study: MHAS 2012 data files description, version I, septiembre de 2013 [consultado el 1 octubre de 2013]. Disponible en: http://www.mhasweb.org. [ Links ]
9. Turra CM, Goldman N, Seplaki CL, Glei DAWeinstein M. Determinants of mortality at older ages:The role of biological markers of chronic disease. Popul Dev Rev 2005;31 (4):675-698. [ Links ]
10. Hurd MD, McFadden D, Merrill A. Predictors of mortality among the elderly. En Wise DA ed. Themes in the economics of aging. Chicago, IL: University of Chicago Press, 2001:171 -198. [ Links ]
11. Gavazzi G, Herrmann F, Krause K-H. Aging and infectious diseases in the developing world. Clin Infect Dis [serie en internet] 2004;39(I):83-91 [ Links ]
12. Bygbjerg IC. Double burden of noncommunicable and infectious diseases in developing countries. Science 2012;337:1499-1501. [ Links ]
13. Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med 2002;1162(20):2269-2276. [ Links ]
14. González-González C, Sánchez-García S, Juárez-Cedillo T, Rosas-Carrasco O, Gutiérrez-Robledo LM, García-Peña C. Health care utilization in the elderly Mexican population: expenditures and determinants. BMC Public Health. BioMed Central Ltd 2011; 11:192. [ Links ]
Received on: December 9, 2013
Accepted on: April 29, 2014
 Corresponding author:
Corresponding author:
Dra. Rebeca Wong.
Sealy Center on Aging, University of Texas Medical Branch.
301 University Blvd., Rebecca Sealy Bldg., Room 6.100,
Galveston TX 77555-0177.
E-mail: rewong@utmb.edu.
Declaration of conflict of interests. The authors declare that they have no conflict of interests.













