Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Salud Pública de México
Print version ISSN 0036-3634
Salud pública Méx vol.57 n.5 Cuernavaca Sep./Oct. 2015
Artículo original
Assessing the physical activity environment in Mexican healthcare settings
Evaluación del entorno de actividad física en el sector salud
Karla I Galaviz, PhD,(1) Rebecca E Lee, PhD,(2) Kim Bergeron, PhD,(3) Lucie Lévesque, PhD.(3)
(1) Hubert Department of Global Health, Emory University. Atlanta, USA.
(2) College of Nursing and Health Innovation, Arizona State University. Phoenix, Arizona, USA.
(3) School of Kinesiology and Health Studies, Queen's University. Kingston, Ontario, Canada.
Abstract
Objective. To assess the informational, educational and instrumental environments among Mexican healthcare settings for their potential to promote physical activity (PA).
Materials and methods. The Environmental Physical Activity Assessment Tool for Healthcare Settings (EPATHS) was developed to assess the PA environments of 40 clinics/hospitals representing the three Mexican healthcare systems in Guadalajara. The EPATHS assessed the presence and quality of PA enhancing features in the informational (e.g. signage), educational (e.g. pamphlets), and instrumental (e.g. stairs) environments of included clinics/hospitals.
Results. 28 (70%) clinics/hospitals had more than one floor with stairs; 60% of these had elevators. Nearly 90% of stairs were visible, accessible and clean compared to fewer than 30% of elevators. Outdoor spaces were observed in just over half (55%) of clinics/hospitals, and most (70%) were of good quality. Only 25% clinics/hospitals had educational PA materials.
Conclusions. The PA instrumental environment of Mexican healthcare settings is encouraging. The informational and educational environments could improve.
Key words: built environment; health promotion; primary health care; physical activity.
Resumen
Objetivo. Evaluar el entorno informacional, educacional e instrumental de clínicas/hospitales en México y determinar su potencial para promover la actividad física (AF).
Material y métodos. Se desarrolló una herramienta (Environmental physical activity assessment tool for healthcare settings [EPATHS]) para evaluar los entornos de AF en 40 clínicas/hospitales de Guadalajara afiliados a los tres sistemas de salud de México. Con el EPATHS se evaluó la presencia y calidad del entorno informacional (pe.: letreros), educacional (ep.: panfletos) e instrumental (pe.: escaleras).
Resultados. Del total de clínicas/hospitales incluidos, 28 (70%) tuvieron más de un piso y escaleras; de éstos, 60% tuvo elevadores. Cerca de 90% de las escaleras eran visibles, accesibles y limpias, lo que contrasta con menos de 30% para los elevadores. En 55% de las clínicas/hospitales se observaron áreas verdes, la mayoría de éstas (80%) de buena calidad. En sólo 25% de las clínicas/hospitales se observaron materiales educativos sobre AF.
Conclusiones. El entorno instrumental en clínicas/hospitales mexicanos es alentador. Los entornos informativos y educativos podrían mejorar.
Palabras clave: ambiente construido; promoción de la salud; atención primaria; actividad motora.
Environments in which people live, learn, work and play can either promote or deter physical activity.1 Because physical activity (PA) levels among Mexican adults remain far from optimal,2,3 attention to, and enhancement of, these environments represent a low-cost and sustainable strategy to promote PA in Mexico. The healthcare setting represents one environment in which PA can be promoted. Both patients and employees can be effectively reached in these settings4,5 and PA can be effectively promoted.6,7 Further, the healthcare context offers resources, infrastructure and a workforce that can be used to promote PA,8 thereby, improving the feasibility of introducing PA programs.
Environments relevant to PA have been categorized into micro- (e.g. doctor's office), meso-, exo- (e.g. social prompts/networks), and macro-environments (e.g. policies, healthcare systems).9 Barriers to PA engagement can be encountered in each of these environments. For instance, a healthcare system may not prioritize PA promotion policies and strategies for its employees and its patients. As a result, these settings may not implement strategies to promote PA within the building or connect people with resources in the community. Finally, a physician may not prompt/support PA in his/her practice (e.g. counseling, prescription), which would mean that patients do not receive encouragement for their PA.
The healthcare setting represents a micro-environment where PA can be promoted through informational, educational, and instrumental strategies. Informational strategies focus on increasing awareness about PA opportunities in the setting; examples include signage and floor stickers promoting stair use, which have been shown to increase stair use.7,10,11 Educational strategies focus on teaching people about the benefits of PA and how to be active; examples include displaying posters and offering brochures or self-help materials, which can help increase regular PA.12,13 Instrumental strategies help make the physical environment supportive for PA. Features of the physical environment such as availability, accessibility, attractiveness, safety, and convenience of stairs, walking paths, and outdoor spaces can enhance PA.7,11,14-17 Examples include building walking paths, improving the conditions of stairs, and limiting access to elevators, which can lead to increases in PA within the setting.11,15,17,18
Strategies for promoting PA within the healthcare environment have been implemented in the United States, Canada and Europe.19-22 In Brazil, primary care units across the country have introduced approaches to promote PA, such as walking groups, communication and informational strategies.23,24 Information about the Mexican healthcare environment is lacking, and whether similar strategies have been implemented within the system is unknown. The Mexican healthcare system is comprised of three sub-systems: the National Institutes for Social Security, the Secretary of Health, and the private sector. The insured seek healthcare within the National Institutes for Social Security (50%), while the uninsured seek healthcare within the Secretary of Health (45%) and the private sector (5%).25 Because Mexican patients see healthcare settings as the place to receive health-related information, and given that Mexican healthcare workers have been found to be insufficiently active,26,27 both patients and healthcare workers could benefit from improved PA opportunities in the healthcare setting.
In order to design environmental strategies for promoting PA within Mexican healthcare settings, it is necessary to assess and document the current features of this micro-environment. Existing tools for measuring PA micro-environments28-30 are not specific to the healthcare setting, and tools to measure the PA healthcare environment are lacking. Because the features of micro-environments influence PA,7,10,11,15,17,18 it is important to develop tools to further explore this link, particularly within healthcare settings. Thus, the purpose of this study was to assess and compare the informational, educational and instrumental environments among the three Mexican healthcare subsystems for their potential to promote PA using a novel observational tool.
Materials and methods
Design and sample. A cross-sectional study was conducted in primary care clinics and hospitals (clinics/hospitals) from Guadalajara, the second largest city in Mexico.31 Using systematic random sampling, 50 clinics/hospitals were selected from a list provided by the Jalisco Secretary of Health containing the names and addresses of all clinics/hospitals in Guadalajara (N=263). The selection of clinics/hospitals was stratified by healthcare subsystem and the proportion selected from each subsystem was based on the proportion of patients attending each: 50% social security clinics, 45% Secretary of Health clinics and 5% private clinics. Eligible clinics/hospitals were those on the list with a valid address located in Guadalajara. The data were collected in the spring of 2012 and analyzed in the summer of that year.
Environmental physical activity assessment tool for healthcare settings (EPATHS). The EPATHS was developed to measure the PA informational, educational, and instrumental environments in healthcare settings via direct observation (figure 1). This tool aims to identify environmental attributes that have been shown to influence PA in other micro-environments. The EPATHS builds on an observational checklist used in a previous study32 to assess the educational environment in a clinical context, and is informed by informational and instrumental elements outlined in the New York Active Design Guidelines.33 The EPATHS was developed and pilot-tested over a three-month period. First, experts in the PA built environment field (n=4) from Mexico, Canada and the United States met to develop the first draft of the EPATHS. Second, the first draft of the EPATHS was tested in one clinic; after this, experts met to discuss the assessment and to revise the tool. The revised EPATHS was tested again where two trained raters independently assessed the same four clinics/hospitals. The inter-rater reliability achieved was kappa=0.81, which reflects substantial agreement.34 In a final meeting, the team of experts examined, discussed, and established the initial face validity of the tool.
The EPATHS is divided into two sections; one section assesses the instrumental and informational environments and the second assesses the educational environment of the healthcare setting. For the instrumental and informational environments, the EPATHS assesses the presence of indoor vertical travel opportunities (e.g. stairs, elevators) and outdoor recreation opportunities (present=1; not present=0). The quality of these areas is then assessed according to the following criteria: available, accessible, visible, clean, safe, and accompanied by signage (yes=1; no=0). The educational environment is assessed by documenting the availability (available=1; unavailable=0) of printed materials such as posters, brochures, leaflets, flyers, magazine articles, and cartels (hand-made posters) about PA. Message framing, the emphasis of a message on the benefits of adopting (gain frame) or the costs of failing to adopt (loss frame) a behavior, can be used in educational materials. Gain framed messages can optimize the persuasiveness of PA messages35 and have been shown to be more effective for the promotion of PA intentions and behavior, than loss framed messages.35-36 Thus, the content (i.e. what information was presented) and message frame (i.e. gain/loss frame) of these educational materials is also recorded. Level of care (primary, secondary, and tertiary), number of floors, and type of healthcare subsystem of the clinic/hospital assessed is also recorded. Operational definitions for each criterion are provided in table I, and instructions for conducting the assessment are provided in a two-page manual. Scoring is based on presence/absence and quality (e.g. visibility, cleanness) of the environmental features relevant to PA.
Assessment procedures. The EPATHS assessment was conducted by the first author following instructions outlined in the manual. Briefly, the availability, visibility, accessibility and signage of the instrumental and informational environments were assessed while standing at an ideal vantage point (e.g. clinic/hospital entrance). The cleanliness, usage, and safety of these areas were assessed by walking through them. The educational environment of two high-traffic areas (i.e. the lobby and one waiting room) was assessed in each clinic/hospital. Finally, all visible PA-related printed materials (e.g. posters, magazine articles, cartels) were recorded. To be included, these materials needed to contain at least one sentence about PA health benefits, or PA recommendations, or advice about ways to be physically active. After completing these observations, the clinic/hospital was left.
Statistical analyses. Frequency counts were used to estimate proportions of the informational, educational, and instrumental environmental indicators present. Fisher's exact tests were conducted to gauge associations between type of healthcare subsystem and level of care with the availability of educational and instrumental environment features. The overall statistical significance was set at p<0.05, and the Bonferroni correction method was used. Analyses were conducted using the Statistical Package for Social Sciences (SPSS) version 18 for Windows.*
Results
From the original 50 randomly selected clinics/hospitals from a list, 40 were found at the anticipated address and included in the study. There were 15 (37%) clinics/hospitals from the Secretary of Health, 14 (35%) from the Social Security Institutes, and 11 (28%) from the private sector (table II).
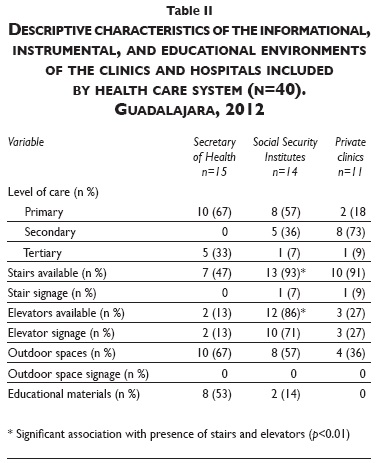
Informational environment. From the stairs assessed (n=28), 7% had signs indicating their location, and none had signs prompting their use. Similarly, from the elevators assessed (n=17), 12% had signs about their location. There were no signs indicating outdoor space locations or promoting their use (table II). No significant associations between indicators of the informational environment with level of care or healthcare subsystem type were found.
Educational environment. From the clinics/hospitals assessed (n=40), 25% had educational PA materials, all of which were primary care clinics from either the Secretary of Health or the Social Security Institutes (table II). The only PA-related educational materials available were posters and cartels. The same generic poster about health promotion that included a single sentence prompting healthcare workers to promote patient PA was available in eight primary care clinics from the Secretary of Health. Cartels were available in two primary care clinics from the Social Security Institutes. These cartels contained detailed information about PA benefits and recommendations for patients (figure 2). The PA messages in all posters and cartels were gain framed, that is, focused on the benefits of adopting PA. There were no significant associations with healthcare subsystem type or level of care.
Instrumental environment. From the clinics/hospitals assessed (n=40), 70% had more than one floor with stairs. Of these multistory clinics/hospitals (n=28), 60% had elevators. Regarding quality, all of the assessed stairs (n=28), were safe, meaning that they had slip-resistant floor, handrails and could fit two people. Nearly 90% of the stairs were accessible, clean and the principal means for vertical travel. About the same proportion of stairs (57%) and elevators (65%) were visible from either the clinic/hospital's entrance or principal path of travel. Only about a third of the assessed elevators were the principal means of vertical travel, and less than these were accessible, clean and safe (table III). A significant association between the opportunity for vertical travel by stairs or elevators with healthcare subsystem type was observed, with more Social Security institutions including these features (p<0.05).
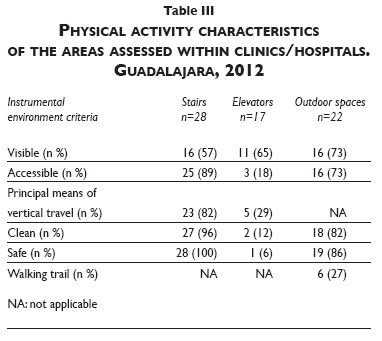
Outdoors, gardens and paved terraces were observed in 55% of the assessed clinics/hospitals. Of the 22 outdoor spaces inventoried, more than 70% were visible, accessible, clean and safe, and 30% had walking trails (table III). The outdoor recreation spaces available were grassed gardens and paved terraces with no PA specific features (e.g. equipment, floor painting.
Discussion
The EPATHS instrument was found to be a promising and feasible tool to systematically assess the availability and quality of environmental features hypothesized to influence PA within healthcare settings. Using the EPATHS, we found that the PA instrumental environment of Mexican healthcare settings is encouraging, but the informational and educational environments could be improved.
This is the first study to examine the PA environment in healthcare settings within a middle-income country. Overall, the instrumental environment in the assessed clinics/hospitals included some encouraging features, namely stairs and outdoor spaces. The majority of the stairs and outdoor spaces available were of good quality (accessible, clean and safe), although around half of the stairs were not visible from the entrance or principal path of travel. The informational and educational environments were poor. Signs indicating stair location were seldom present, and nonexistent for outdoor spaces. Few posters and cartels were observed only in primary care clinics but the PA information presented was insufficient.
The present findings suggest that there is room for improving the informational and educational environments within the Mexican healthcare context. Existing evidence14-16 may provide insight into promising, simple, and low-cost strategies to enhance PA opportunities in Mexican healthcare settings. For example, given that stairs are already available and accessible in many clinics and hospitals, encouraging stair use represents a feasible strategy for promoting PA among healthcare professionals and patients. It has been shown that relatively modest increases in stair use can have positive fitness effects in healthcare professionals.7 Effective strategies for promoting stair use include implementing signs indicating stair location, posters and floor stickers to promote stair use and making physical improvements to existing stairs to enhance safety and aesthetic appeal.7,10,15
Although findings show that elevators were less accessible and less frequently used for vertical travel compared to stairs, when they were present, they were highly visible. Given that the presence of elevators deters stair use,17,18 strategies for promoting stair use over the elevators may be warranted. Effective strategies include having fewer elevators working in the building (e.g. three out of four) or programming elevators to only stop on every other floor.17,18 These strategies can be directed at healthcare staff and patients who are able to use the stairs. These strategies are feasible and can be implemented to the extent that they do not jeopardize vertical travel accessibility for patients who may need the elevators.
Within workplaces, the availability of recreational areas such as outdoor spaces, fitness facilities, and walking paths promotes PA.11,37 In this study, half of the hospitals and clinics had an outdoor recreation space; however, there were no signs indicating location, the quality of spaces was poor, and few had a walking path. It has been suggested that by improving the accessibility and the visibility of outdoor spaces from the main building circulation system, the use of these spaces might improve.38 Further, the inclusion of a walking path has the potential to increase PA.37 Thus, building a walking path where none exists, or improving access to, and conditions of, existing outdoor spaces represent additional ways in which to enhance the PA opportunities in Mexican healthcare settings.
In this study, only primary care clinics from public institutions had educational PA materials (i.e. posters and cartels). This is not surprising given that most preventive and health promotion strategies are implemented in primary care. Although posters were available in some clinics, the information they contained about PA was minimal (i.e. a single sentence in the poster) and directed at patients. Cartels were more encouraging as they had more information about PA benefits and recommendations, but these were present in only two clinics and targeted patients. Promoting PA among healthcare professionals has the potential to not only improve their own health but also their health promotion practices towards patients. For instance, physically active Mexican primary care physicians are more likely to prescribe PA to their patients.27 The use of posters for promoting PA in hospitals has been shown to increase stair use among healthcare workers,7 and the use of motivational brochures and self-help materials delivered in the workplace have been shown to promote weekly PA among employees.12,13 Further, it has been suggested that tailored messages, gain-framed messages, and self-efficacy change messages are promising formulations of PA messages.36 Employing health promotion posters or cartels is a simple and low-cost strategy that some Mexican clinics are already implementing and which could easily be transferred to other clinics and hospitals across Mexico, including patients and healthcare professionals as an audience for the messages.
Although attention to the PA-promoting qualities of several micro-environments has increased, a limited number of tools for measuring these environments have been developed and are not specific to PA behavior or the healthcare environment.28,29 The EPATHS was developed to address this gap and represents the first tool focused on measuring the PA environment specific to the healthcare setting. Although the EPATHS was developed within the context of Mexico, it can be easily adapted to fit the characteristics of other healthcare contexts. In this pilot test, the EPATHS was found to have face validity and good inter-rater reliability. The test-retest reliability as well as the predictive validity of the EPATHS are yet to be established. The EPATHS offers a promising tool for measuring the PA environment within healthcare settings and for linking it to PA behaviors or intervention effects. This study provides preliminary evidence of the usefulness of the tool but further testing and refinement are warranted.
This was a descriptive study where no causal relations were examined. Findings from this study only provide a snapshot of the existing PA environmental features present in clinics and hospitals in Guadalajara, Mexico; further research is required to understand the PA environment in other clinics and hospitals in the country. Another limitation was that PA behaviours of patients and healthcare professionals were not measured, which prevents us from linking the healthcare environment features with PA behaviour. The test-retest reliability and the predictive validity of the tool were not established, which limits conclusions about the reliability and validity of the tool. Further, the availability and accessibility of PA-related equipment/facilities (e.g. lockers, bike racks, gyms) were not measured, a limitation that will be addressed in future studies using the EPATHS. Finally, given that the time of the day when the assessment was conducted varied across clinics/hospitals and that the number of stair/elevator users was not recorded, conclusions about vertical travel by stairs should be interpreted cautiously.
Conclusion
The PA instrumental environment of Mexican healthcare settings is encouraging. However, there is room for improvement as informational and educational strategies that inform patients and healthcare professionals about what they need to do and how they can be physically active are lacking. The infrastructure to increase opportunities to be physically active within the healthcare settings, which is the most expensive feature to intervene on, is in place. Evidence-based, cost-effective, and feasible strategies that focus on promoting the use of such infrastructure are available and could be implemented on a wide scale across Mexican healthcare settings. PA should be promoted in every environment in which people live, work and play, and the healthcare setting offers a unique opportunity to promote PA among adults.
References
1. Sallis JF, Glanz K. Physical activity and food environments: solutions to the obesity epidemic. Milbank Q 2009;87:123-154. [ Links ]
2. Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012;380:247-257. [ Links ]
3. Gutiérrez JP, Rivera-Dommarco J, Shamah-Levy T, Villalpando-Hernández S, Franco A, Cuevas-Nasu L, et al. Encuesta Nacional de Salud y Nutrición 2012. Resultados nacionales. Cuernavaca, México: Instituto Nacional de Salud Pública, 2012. [ Links ]
4. Proper K, van Mechelen W. Effectiveness and economic impact of worksite interventions to promote physical activity and healthy diet. Geneva: World Health Organization, 2008. [ Links ]
5. Tulloch H, Fortier M, Hogg W. Physical activity counseling in primary care: who has and who should be counseling? Patient Educ Couns 2006;64:6-20. [ Links ]
6. Patrick K, Pratt M, Sallis RE. The healthcare sector's role in the U.S. National Physical Activity Plan. J Phys Act Health 2009;6:S211-S219. [ Links ]
7. Meyer Pl, Kayser B, Kossovsky MP, Sigaud P, Carballo D, Keller PF, et al. Stairs instead of elevators at workplace: cardioprotective effects of a pragmatic intervention. Eur J Cardiovasc Prev Rehabil 2010;17:569-575. [ Links ]
8. Lobelo F, Stoutenberg M, Hutber A. The Exercise is Medicine® Global Health Initiative: a 2014 update. Br J Sports Med 2014;48(22):1627-1633. [ Links ]
9. Spence JC, Lee RE. Toward a comprehensive model of physical activity. Psychol Sport Exerc 2002;4(1):7-24. [ Links ]
10. Bungum T, Meacham M, Truax N. The effects of signage and the physical environment on stair usage. J Phys Act Health 2007;4(3):237. [ Links ]
11. Crespo NC, Sallis JF, Conway TL, Saelens BE, Frank LD. Worksite physical activity policies and environments in relation to employee physical activity. Am J Health Promot 2011; 25(4):264-271. [ Links ]
12. Plotnikoff RC, Brunet S, Courneya KS, Spence JC, Birkett NJ, Marcus B, et al. The efficacy of stage-matched and standard public health materials for promoting physical activity in the workplace: the Physical Activity Workplace Study (PAWS). Am J Health Promot 2007;21(6):501-509. [ Links ]
13. Marcus BH, Emmons KM, Simkin-Silverman LR, Linnan LA, Taylor ER, Bock BC, et al. Evaluation of motivationally tailored vs. standard self-help physical activity interventions at the workplace. Am J Health Promot 1998;12(4):246-253. [ Links ]
14. Nicoll G. Spatial measures associated with stair use. Am J Health Promot 2007; 21(4s):346-352. [ Links ]
15. Kerr NA, Yore MM, Ham SA, Dietz WH. Increasing stair use in a worksite through environmental changes. Am J Health Promot 2004;18(4):312-315. [ Links ]
16. Dodson EA, Lovegreen SL, Elliott MB, Haire-Joshu D, Brownson RC. Worksite policies and environments supporting physical activity in midwestern communities. Am J Health Promot 2008;23(1):51-55. [ Links ]
17. Nicoll G, Zimring C. Effect of innovative building design on physical activity. J Public Health Policy 2009;30:S111-S123. [ Links ]
18. Olander EK, Eves FF. Elevator availability and its impact on stair use in a workplace. J Environ Psych 2011;31(2):200-206. [ Links ]
19. Centers for Disease Control and Prevention. Healthy hospital practice to practice series (P2P) [internet doccument] [accessed: January 2014]. Availavle at: http://www.cdc.gov/nccdphp/dnpao/hwi/resources/hospital_p2p.htm. [ Links ]
20. Ontario Health Promoting Hospital and Health Service Network. Availavle at http://ontariohph.com/
21. World Health Organization. Putting health promoting hospitals' policy into action. Working paper of the WHO collaborating centre on health promotion in hospitals and health care (report). Vienna: WHO, 2006. [ Links ]
22. Groene O, Garcia-Barbero M. Health promotion in hospitals: evidence and quality management (report). Copenhagen: Country Systems, Policies and Services Division of Country Support WHO Regional Office for Europe, 2005. [ Links ]
23. Ramos LR, Malta DC, Gomes GA, Bracco MM, Florindo AA, Mielke GI, et al. Prevalence of health promotion programs in primary health care units in Brazil. Rev Saude Publica 2014;48:837-844. [ Links ]
24. Gomes GA, Kokubun E, Mieke GI, Ramos LR, Pratt M, Parra DC, et al. Characteristics of physical activity programs in the Brazilian primary health care system. Cad Saude Publica 2014;30:2155-2168. [ Links ]
25. Frenk J, Gomez O, Knaul FM. The democratization of health in Mexico: financial innovations for universal coverage. Bull World Health Organ 2009;87:542-548. [ Links ]
26. Fanghänel-Salmón G, Sánchez-Reyes L, Arellano-Montaño S, Valdés-Liaz E, Chavira-López J, Rascón-Pacheco RA. The prevalence of risk factors for coronary disease in workers of the Hospital General de Mexico. Salud Publica Mex 1997;39(5):427-432. [ Links ]
27. Galaviz KI, Jauregui E, Fabrigar L, Latimer-Cheung A, Lopez y Taylor J, Lévesque L. Physical activity precription among Mexican physicians: a structural equation model testing the theory of planned behavior. Int J Clin Pract 2015;69(3):375-383. [ Links ]
28. Oldenburg B, Sallis JF, Harris D, Owen N. Checklist of Health Promotion Environments at Worksites (CHEW): development and measurement characteristics. Am J Health Promot 2002;16(5):288-299. [ Links ]
29. Fisher B, Golaszewski T, Barr D. Measuring Worksite Resources for Employee Heart Health. Am J Health Promot 1999;13(6):325-332. [ Links ]
30. Lee RE, Booth KM, Reese-Smith JY, Regan G, Howard HH. The physical activity resource assessment (PARA) instrument: evaluating features, amenities and incivilities of physical activity resources in urban neighborhoods. Int J Behav Nutr Phys Act 2005;2(1):2-13. [ Links ]
31. Instituto Nacional de Estadística y Geografía. Censo de poblacion y vivienda 2010 [documento en internet]. México: Inegi, 2010 [accessed: January 2012]. Available at: http://www.censo2010.org.mx/ [ Links ]
32. Anis NA, Lee RE, Ellerbeck EF, Nazir N, Greiner KA, Ahluwalia JS. Direct observation of physician counseling on dietary habits and exercise: patient, physician, and office correlates. Prev Med 2004;38(2):198-202. [ Links ]
33. Lee KK. Developing and implementing the active design guidelines in NewYork City. Health Place 2012;18:5-7. [ Links ]
34. Landis JR, Koch GG. The Measurement of observer agreement for categorical data. Biometrics 1977;33(1):159-174. [ Links ]
35. Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science 1981;211(4481):453-458. [ Links ]
36. Latimer A, Brawley L, Bassett R. A systematic review of three approaches for constructing physical activity messages: what messages work and what improvements are needed? Int J Behav Nutr Phys Act 2011;7(1):36. [ Links ]
37. Matson-Koffman DM, Brownstein JN, Neiner JA, Greaney ML. A site-specific literature review of policy and environmental interventions that promote physical activity and nutrition for cardiovascular health: what works? Am J Health Promot 2005;19(3):167-193. [ Links ]
38. Zimring C, Joseph A, Nicoll GL, Tsepas S. Influences of building design and site design on physical activity: Research and intervention opportunities. Am J Prev Med 2005;28(2, suppl 2):186-193. [ Links ]
Received on: February 3, 2015
Accepted on: July 23, 2015
 Corresponding author:
Corresponding author:
Lucie Lévesque.
School of Kinesiology and Health Studies Queen's University.
Division Street 28. K7L 3N6 Kingston, Ontario, Canada.
E-mail: levesqul@queensu.ca
Declaration of conflict of interests. The authors declare that they have no conflict of interests.
* IBM, Armonk NY.













