Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Salud Pública de México
versión impresa ISSN 0036-3634
Salud pública Méx vol.56 supl.2 Cuernavaca 2014
Artículo original
Effects of an intervention strategy for school children aimed at reducing overweight and obesity within the State of Mexico
Efecto de una intervención en escolares del Estado de México para reducir el sobrepeso y la obesidad
María del Carmen Morales-Ruán, MSc,(1) Teresa Shamah-Levy, PhD,(1) Claudia Isabel Amaya-Castellanos, MPH,(1) Araceli Apolonia Salazar-Coronel, MPH,(1) Alejandra Jiménez-Aguilar, MSc,(1) Maritza Alejandra Amaya-Castellanos, MPH,(1) Ignacio Méndez-Gómez Humarán, MSc.(2)
(1) Centro de Investigación en Nutrición y Salud, Instituto Nacional de Salud Pública. Cuernavaca, México.
(2) Centro de Investigación en Matemáticas, A.C. Aguascalientes, México.
Abstract
Objective. This study explored the intervention effect of the "Nutrition on the Go" strategy on the prevalence of overweight and obesity (OW+O), according to the role played by different patterns.
Materials and methods. Pattern Groups (PG) were determined based on schools' food availability and other variables at individual level: nutrition knowledge, physical activity, socioeconomic level and self-efficacy, using an ecological approach. The PG classification was achieved using Ward's cluster method.
Results. The prevalence of OW+O was higher in PGI (intermediate food availability and high socioeconomic index [SEI]) compared to PG 2 (high availability of food and lower SEI) and PG 3 (low availability of food and medium SEI) with a lower prevalence (p<0.00I). The PG-intervention interaction showed differences for PG 3 (p=0.066), the stage-PG interaction showed differences between PGs I and 3 (p=0.014) and between PGs 2 and 3 (p=0.055).
Conclusions. Differences between PGs have important implications for the prevalence of OW+O.
Key words: intervention studies; physical activity; health promotion; schools; Mexico.
Resumen
Objetivo. Explorar el efecto de la intervención "Nutrición en movimiento" en el sobrepeso y obesidad (SO+O) en escolares, de acuerdo con diferentes patrones.
Material y métodos. Los grupos de patrones (GP) fueron determinados con base en alimentos disponibles en la escuela y variables de conocimientos, actividad física, nivel socioeconómico y autoeficacia a nivel individual, usando un enfoque ecológico. La clasificación en GP se construyó por conglomerados con el método de Ward.
Resultados. La prevalencia de SO+O fue mayor en el GP I (mediana disponibilidad de alimentos e índice socioeconómico [ISE] alto), más baja en los GP 2 (alta disponibilidad de alimentos e ISE bajo) y 3 (baja disponibilidad de alimentos e ISE medio) (p<0.00I). La interacción entre GP e intervención muestra diferencias para GP 3 (p=0.066), la interacción GP con etapa mostró diferencias entre GP I contra 3 (p=0.014) y 2 contra 3 (p=0.055).
Conclusiones. Diferencias en GP tienen implicaciones importantes en la prevalencia de SO+O.
Palabras clave: estudios de intervención; actividad física; promoción de la salud; escuelas; México.
In recent years, the rate of overweight and obesity (OW+O) in school-age children has increased alarmingly. The increase in overweight is particularly significant among African-American and Latin American children1, especially among Mexican school-age children, in whom the prevalence has increased over recent years and now affects approximately one out of every three school-age children.2
The influence of the environment and its correlation with obesity and unhealthy lifestyles in diverse populations has been described previously.3 It has been documented that the availability of energy-dense foods and drinks and few opportunities for physical activity are elements that are directly related to the increase in OW+O.3
The term "obesogenic environment" refers to "an environment that promotes gaining weight and one that is not conducive to weight loss" within the home or workplace.4 In other words, the obesogenic environment refers to an environment that contributes to obesity.4
In Mexico the "obesogenic environment" is also a prevalent characteristic of schools. Some studies conducted in elementary schools indicate that school-age children have opportunities for food consumption as many as five times within a 4.5-hour period during school hours,5 which may be equivalent to 50% of the total daily requirements (840-1259 kcal). Also, while there is a high availability of energy-dense products, access to performing both systematic and recreational physical activity is limited.6
The objective of the present study was to explore the effect of the "Nutrition on the Go"7 strategy on the prevalence of overweight and obesity among school children with different environment-individual patterns.
Materials and methods
A randomized cluster design was used to study an intervention effect on the prevalence of overweight and obesity in Mexican children. A simple random sample of 60 schools was selected from a total of 2 969 public elementary schools receiving breakfasts, which represent 125 municipalities in the State of Mexico. The experimental group was created with 30 schools randomly assigned to the intervention, and other 30 were used as controls.
The present study included 5th grade children from each selected school. Body mass index (BMI) was used as the main variable to determine a sample size. From a previous study in the same population, the estimated BMI standard deviation was 2.79 and the design effect was 1.68. The expected statistical difference in BMI between intervention and control groups was fixed at 0.45; with 95% confidence and a sample power of 80%, a sample size of 1 000 children was obtained.8 We selected a random sample of 17 children from each school to collect statistical data, adding up to a total of 510 children for the intervention group and 510 for the control, in order to have a sufficient sample size at follow-up. The non-response rate expected in this study was ≤ 5%.
Two stage transversal measurements -baseline and final- were conducted during the study. The baseline assessment was conducted in early November 2010; the intervention strategy was implemented between November 2010 and the first half of May 2011, and the final evaluation was conducted between late May and early June 2011.
Intervention
The "Nutrition on the Go" strategy is described elsewhere,9 including the analysis of its effectiveness. The intervention was conducted during a 6-month period in the schools and included the following activities:
• Nutrition and physical activity workshops—these were divided into six sessions that included participatory recreational activities for children to gain knowledge and skills to properly select healthful foods and to promote physical activity.
• Puppet theater: A puppet theater was developed, based on the peer learning theory, in which fifth grade students presented the play "Saving Sanopolis" to younger children at school. The script for the play was previously developed and validated by those in charge of the project. Didactic resources provided to each school included the play's script, the puppets and the curtain. Performances took place once a week.
• Physical activity: Organized activities involving motion were conducted and performed each day prior to the start of classes and included warm-ups, physical activity and relaxation.
• Physical activation: To provide incentives to perform physical activity in the school environment, the campaign planned an exercise routine, beginning gradually with two days per week for 15 minutes before the beginning of classes, in order to create a habit of daily exercise. Didactic resources used included a manual of routines and a music CD.
• Organized games during break time (twice a week): Active and safe participation of teachers and children was promoted during the break with educational materials provided for these activities.
• Organized games: These were held so that the school children might participate, according to their interests, in games and activities that involve movement during the 30-minute recess twice a week. In addition, the participation of the entire school community was encouraged, with the intention of promoting active and safe recesses. A manual was used with suggestions for games and dynamics according to age-group.
• Banners: Placing banners at the entrance of the school: In order to position the campaign in the school community, a 2-meter high banner was hung which read: "This school promotes healthy recess."
• Recipe calendars: Calendars for the school year were distributed to the parents, which included recipes to prepare snacks (including fruits and vegetables). The recipe-calendar also included messages related to the importance of performing physical activity and of hydration with plain water.
• Activities for teachers and school cooperative: Two-day awareness raising workshops were held in each school about healthy eating and physical activity. The workshops were aimed at highlighting the importance of the availability of fruits and vegetables as well as a pure water supply inside the school and of the benefits of a healthy lifestyle.
• Broadcasting of audio spots on the schools' public address systems three times per week during the break: messages were in regard to consumption of fruits, vegetables, pure water and physical activity during break time.
• Sale of fruits, vegetables and pure water at the school food cooperative: a session (~1 hour) was held with the store personnel to convey information and to make suggestions about healthful eating.
Instruments
A set of measuring instruments were created and applied in each stage in order to collect all information considered in this study. This included:
Body mass index. Weight was determined using a Tanita electronic scale with a precision of 100 grams. Height was measured using Dynatop stadiometers with a 2-m capacity and a precision of 1 mm. Measurements were made at the beginning and at the end of the 2010-2011 school periods. Body mass index (BMI = kg/m2) was calculated for all students in order to determine classifications of OW+O, considering the distribution and cut-off points proposed by the International Obesity Task Force (IOTF).10
Food. A semiquantitative food frequency questionnaire was used to record diets for the children using the same instrument used in Health and Nutrition Survey (Ensanut-2006), whose methodology has been published previously.11
The socioeconomic level was determined based on information related to housing characteristics and possession of goods. A principal component analysis12 was used to obtain the socioeconomic index using the first component, which had seven variables and accounted for 40.2% of the total variance. This index was categorized into tertiles to obtain a three-tiered socioeconomic classification defined as low, medium and high.
Physical activity. In order to record the physical activity performed by school-age children, a semiquantitative questionnaire, developed and validated by Hernández and colleagues and based on the Youth Activity Questionnaire,13 was used to measure physical activity and inactivity.13 School-age children were classified according to the time spent performing vigorous and moderate activities, using the following criteria: school-age children who reported performing at least seven hours per week of moderate and/or vigorous activity were classified as active;14 those reporting less than seven hours and at least four hours were classified as moderately active, and those performing less than four hours a week of vigorous and/or moderate activity were classified as inactive.15
Time spent watching television. Time spent in front of the television or computer screen was classified according to time in hours spent watching television shows and movies, as well as playing video games at home. Adequate time class was considered to be 12 hours/week on average (~80 minutes/day). More than 12 hours and <21 hours per week (an average of 135 minutes a day) was classified as less than adequate, and >21 hours was considered inadequate (average of 3 hours or more per day). The American Academy of Pediatrics (2001) recommends no more than 1 to 2 hours per day.16
Knowledge. Topic identification was carried out through formative research: discussion groups, meetings with experts (psychologists, teachers, nutritionists and physical education teachers) and review of specialized literature. 20 questions were structured with the collected information. Evaluation criteria were writing style, comprehension and content of items. The final questionnaire consisted of 13 items (seven in the food section and six in the physical activity section). Both sections were designed with closed multiple choice questions, and two questions used graphics as answers. A pilot study was carried out with the participation of 30 children to facilitate error detection. These were corrected for the final version.
The results were analyzed and compared considering the average notes obtained by the children in every test -using a scale of 1 to 10- for both food intake and physical activity and according to the group to which they belonged. Finally, a comparison was performed in order to establish the approval percentage among the students for the two topics (≥6 = approved; <6 = failed).
Self-efficacy. To evaluate the self-efficacy of children with respect to physical activity, a 12-item dichotomous scale was used, which was designed and validated for Mexican school-age children by Aedo and Avila (2009).17 The scale consists of three dimensions for self-efficacy: search for positive alternatives, ability to face potential barriers and expectations related to skill or competence.
To assess self-efficacy on the topic of healthy eating, specific questionnaires validated for the population of children were used as a reference, and the items were adapted to be consistent with the physical activity scale. This resulted in a dichotomous choice (yes or no) questionnaire consisting of 13 items with a Cronbach alpha of 0.478. Both scales were previously validated for children of similar ages and characteristics.18,19
The results were obtained from the sum of positive responses (value 1). The minimum value obtained was "0" and the maximum was "12" or "13", according to the number of items in each scale. The percentages of positive responses were then estimated for each evaluation.
Based on the percentage obtained in the previous scores described, the self-efficacy level was categorized for each child according to three groups:
1. Low self-efficacy, classified between 0 and 33.3% when the child had little confidence in him / herself in terms of modifying behavior related to food intake or physical activity.
2. Medium self-efficacy, classified between 33.4 and 66.6% when the child believed he/she could perform various activities (related to his/her eating or physical activity) but was not sure about his/her ability to successfully complete them.
3. High self-efficacy, rated between 66.7 and 100% when the child was convinced he/she would succeed in performing a certain behavior and was willing to modify his/her actions and behaviors.
The above classification was based on the results obtained by the efficacy study regarding this strategy, which does not establish scales for the self-efficacy questionnaire but treats this as a continuous variable in order to avoid loss of sensitivity and predictive information.20 The Eating Self-Efficacy Scale was also included as a way to measure self-efficacy and was adapted for the Spanish language.21
School variables
For school evaluation, observations of the cooperative were conducted, the purpose of these observations was to document the products sold in the school, as well as the access and availability of food, and to record the recipes and their ingredients.
As part of the observation, food preparations -including tacos, sandwiches, and crisp-tortilla preparations- were weighted. The gathered information was recorded in three observation forms:
a) School co-operative stock: This consists of eight sections, each one including a list of food items commonly offered and spaces for recording presence/absence.
b) Food availability: A list including product name, brand and portion size, and spaces for recording presence/absence.
c) Recipe breakdown: A form with blank spaces for recording the ingredients of each recipe as well as thier weight.
For information about the school environment, variables related to the availability of foods in the school were used and classified into four groups. Variables indicating the presence or absence in school were built as follows: the first group covered the availability of dairy and yogurt products; the second group consisted of juices and nectars; the third group included snacks, cookies and crackers, cakes and desserts, and the fourth group, oilseeds and dry pulses (edible seeds).
Schoolyards
In order to evaluate the availability of spaces for physical activity, measures were taken of the schoolyards; the data gathered included not only the width and height data but also the shape (rectangular, square or other), the activity or games performed in it (soccer, basketball, volleyball, multiple uses, floor games etc.), and, finally, whether the schoolyard is covered or not.
Water
In order to to evaluate the availability of water for human consumption, the number and conditions of the drinking fountains existing in the school was recorded in a form, as well as the presence and the potability of water.
Data analysis
A descriptive analysis was conducted using frequencies and means with respective confidence intervals for each variable. In order to verify comparability among groups, X2 tests were performed for independence between the intervention and control groups for the baseline measurements by categorical variables. A student t-test was used for numerical variables when applicable.
Environmental-individual group pattern classifications were built using Ward's hierarchical clustering method with multivariate Euclidian distances.22 Four variables for food availability at school level and average number of children per school using an ecological approach for the socioeconomic index, physical activity, time in front of the television, and scores for knowledge and self-efficacy regarding food intake and physical activity were used. A scheme with patterns grouped into three clusters was chosen based on the shortest distances between groups and an on appropriate environment-individual characterization.
A longitudinal panel data model using Generalized Estimating Equations (GEE) with exchangeable correlation matrix23 was utilized to study the association between the prevalence of overweight and obesity in children and intervention, pattern groups and follow-up stage. Gender and age were used as adjusting variables. A confidence intervals graph was utilized to show factor interactions. All analyses were conducted using Stata 11 package, with the "xtgee" command with an individual ID as panel indicator and stage as time variable. A significance level of 0.05 was used for main effects, and 0.2 was used for interactions.24
Ethical aspects of the study
Written authorization was requested from school principals for school participation in the study and from teachers of the study groups for their inclusion. The purpose and procedure of the study, freedom from risks, and time required to administer the questionnaire along with the process to measure weight and height were explained to the mothers of the participating children. After this explanation, written authorization (informed consent) was requested. This procedure was repeated with the children selected to participate in the study, with a letter of agreement.
The protocol for this study was submitted to and approved by the ethics, biosafety and research committees from the National Institute of Public Health of Mexico.
Results
The baseline characteristics of the children are shown in Table 1, where few statistically significant differences between intervention and control groups were found. T- and X2 tests, respectively, found differences in consumption of nutrients, physical activity and time spent watching television, which are likely to be associated with the lifestyles of the children. Nevertheless, we found no differences in BMI by gender or by prevalence of OW+O.
The study groups showed no significant differences in distribution by gender, age, socioeconomic level, knowledge and self-efficacy related to food intake and physical activity.
Figure 1 shows the pattern group classifications into the three groups obtained from the cluster analysis. These pattern groups were defined as follows:
Group 1: With an intermediate availability of food, high socioeconomic index, high mean scores for physical activity performance and for time spent watching television, and high scores for knowledge and self-efficacy related to food intake and physical activity.
Group 2: With a high availability of foods, a low socioeconomic level and low scores for knowledge, self-efficacy, time spent watching television and physical activity performance.
Group 3: With a low availability of all food groups, low scores for knowledge and self-efficacy regarding food intake and physical activity, medium socioeconomic index, and a score slightly above the average for time performing physical activity and watching television.
Table II shows the population averaged model representing the effect of the pattern groups, stage and the intervention on the probability of overweight and obesity in children. It can be observed that the intervention alone has a protective effect (p=0.007).
The interaction between the intervention and group pattern (overall p=0.18), shows significant differences in the prevalence of OW+O between groups 1 and 3 (p=0.066); on the other hand, a small non-significant difference in group 2 was shown (p=0.43). A significant interaction between the stage and the group patterns was found (overall p=0.04); there were differences between groups 1 and 3 (p=0.014) and between groups 2 and 3 (p=0.055), while there were no differences in prevalence (p=0.44) between groups 1 and 2. There are no significant effects for the intervention-stage or intervention-stage-pattern group interactions.
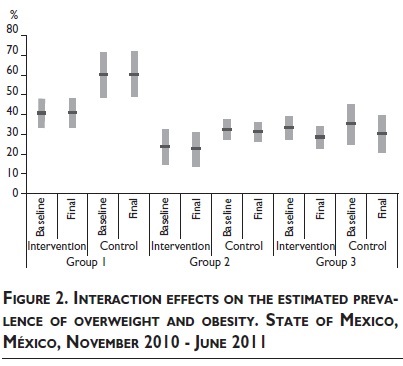
Figure 2 shows the interaction effect of the intervention, stage and pattern groups. It is clear that groups 2 and 3 are associated with a lower prevalence of overweight and obesity (p <0.001 in both cases); in group 1, with a high prevalence of overweight and obesity, the intervention shows group differences. In the pattern group 2, the prevalence was lower, but the intervention effect was not significant, whereas in group 3 there was a small prevalence but a significant reduction on follow up.
Discussion
In the present study, intervention effects were not significant; however, pattern groups showed important differences and implications regarding the prevalence of OW+O. Thus, the implementation of an intervention strategy like "Nutrition on the Go" should take into account the potential effect of different patterns with more obesogenic factors, including high availability of foods, to improve intervention effectiveness.25
Several pervasive environmental factors have been documented to promote energy intake and to limit energy expenditure in children, undermining individual efforts to maintain a healthy bodyweight.26 Different types of environmental influences may also operate across these multiple domains, affecting not only physical characteristics but also those associated with social, cultural and political environments.27
Schools are a natural setting for influencing the food and physical activity environments of children.28 It has been documented that school-age children with higher socioeconomic levels and greater availability of food are more prone to being OW+O;29 the present study produced similar results. This may be due to easy access to energy-rich, low-nutrient foods, as well as access to transportation and the lack of access to healthier alternatives and recreational opportunities.
A study conducted in Brazil found that children who consumed food sold in school stores had a greater likelihood of being overweight or obese (OR=1.56; 95%CI:1.19-2.16). In addition, children from higher socioeconomic backgrounds (OR=1.93, 95%CI:1.32-2.85) also were at increased risk of obesity.30
Another study conducted in the U.S.31 concluded that the differences in BMI by school suggest that some characteristic of the school and/or community environment -perhaps cultural factors or differences in school food, beverage, or physical education policies- facilitate obesity in schools with a high concentration of students with a lower socioeconomic status, beyond individual-level factors.
A small favorable effect of the "Nutrition on the Go" strategy to prevent OW+O9 can be observed. Various articles have documented the effect of strategies to promote healthful eating and physical activity on the prevention and control of OW+O.32-34
An important result is that the differences between pattern groups showed differential possibilities for intervention strategies and also different responses. These are important issues for the design and implementation of effective intervention strategies appropriate to each specific group pattern.
A national survey of schools in Mexico35 documented a high prevalence of OW+O in children of the same age as the children represented in this study (30.3%) with a tortilla-based diet, a low or nonexistent consumption of fruits and vegetables, and a high and frequent consumption of sodas. As to the performance of physical activity, ~50% were inactive.
The availability of food in school stores showed high access to energy-dense foods, foods high in fats and sugars and low in micronutrients and fiber (sweets, commercial snacks, sandwiches, hot dogs, hamburgers and sodas), and fried foods such as sopes, quesadillas, French fries and molletes (bread topped with beans and melted cheese). This situation strengthens an environment that favors the onset of obesity when there are no comprehensive action strategies.
One original aspect of the present study is the cluster analysis, a technique that has been highly employed to construct typographies or classifications useful for the analysis of multivariate data and recently used in an efficient way to solve multiple boundary problems between explanatory variables when building statistical models.
The results of the present study are useful to identify elements of school and individual characteristics that significantly influence the development of obesity and that can be modified for prevention and control in intervention strategies, taking into account that children spend one-half of their days in school.
For the 13 reagent questions included in this self-efficacy scale, Cronbach alpha was 0.478, which indicates that an association may be intermediate, i.e., the estimated efficacy rate has an internal mean consistency. Future studies should validate the self-efficacy scale for food in children.
Study limitations
An important study limitation is the use of indirect instruments to measure children's diet and physical activity; however, the questionnaires used were adapted and pre-tested with representative populations in Mexico,11,13 which contributes to the validity of the presented information. Using the questionnaire of Hernández and colleagues, we evaluated routine physical activity; while we recognize that this is a reporting method that cannot be verified, it is an approach to what happens outside of the school.
Conclusions
In the present study, the effects of the intervention were not significant; however, pattern groups showed important implications for the prevalence of OW+O, and therefore the implementation of an intervention strategy should take into account the potential effect of different patterns to improve effectiveness.
Efforts to tackle obesity should focus on prevention rather than treatment. The challenge that lies ahead is to identify obesogenic group patterns and to influence them so that healthier choices are more available, accessible, and widely promoted to a large proportion of the school community.28 The results obtained in this study will be used as a basis for future studies to explore the impact of pattern groups on intervention strategies in order to improve their efficiency.
Therefore existing school policies should be strengthened to ensure the availability of healthy food as well as limit the energy-dense food supply. In addition, the frequency, intensity and duration of physical activity at school should be increased. Thus, a systematic and coordinated response by the society and an increased political will are required to prioritize the health and well-being of children.
Implications for school health/school health professionals
This study provides evidence of the need for further investigation of the environmental-individual interactions in school. It is necessary to identify the factors that contribute to obesogenic patterns, as well as to implement new strategies for obesity prevention in school-age children. Communities may be able to improve child nutrition through school-based nutritional programs and policies that address the sale of healthy foods.
References
1. Kimbro RT, Brooks-Gunn J, McLanahan S. Racial and ethnic differentials in overweight and obesity among 3-year-old children. Am J Public Health 2007;97(2):298-305. [ Links ]
2. Rivera-Dommarco J, Cuevas-Nasu L, Shamah-Levy T, Villalpando-Hernández S, Ávila-Arcos MA, Jiménez-Aguilar A. Estado nutricio. En: Olaiz-Fernández G, Rivera-Dommarco J, Shamah-Levy T, Rojas R, Villalpando-Hernández S, Hernández-Avila M, et al. Encuesta Nacional de Salud y Nutrición 2006. Cuernavaca, México: Instituto Nacional de Salud Pública, 2006. [ Links ]
3. Institute of Medicine. Joint U.S - Mexico workshop on preventing obesity in children and youth of Mexican origin. Washington, DC, USA: Institute of Medicine of the National Academies, the National Academies Press, 2007. [ Links ]
4. Swinburn B, Eggar G, Raza F. Dissecting obesogenic environments; the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev Med 1999;29(6):563-570. [ Links ]
5. Instituto Nacional de Salud Pública. Documento técnico de recomendaciones para guías de alimentación en escuelas primarias públicas. Caracterización del ambiente escolar en escuelas primarias de estados de la República Mexicana y Recomendaciones para un "Refrigerio escolar saludable". Cuernavaca, Mexico, 2008 [accessed November 6, 2012]. Available at: http://www.insp.mx/images/stories/Centros/cinys/Docs/DOC_TECNICO_GUIAS_INSP_SSA_2010.pdf [ Links ]
6. Bonvecchio A, Safdie M, Theodore F, Aburto N, Gust T, Villanueva M, et al. Diseño y evaluación de una estrategia para la prevención de la obesidad en el niño mexicano. Salud Publica Mex 2007;49(supl 1):229. [ Links ]
7. Instituto Nacional de Salud Pública. Nutrición en movimiento [web-site]. México: INSP, 2011 [accessed December 10, 2012]. Available at: http://www.nutricionenmovimiento.org.mx/dif/. [ Links ]
8. Murray DM. Design and Analysis of Group-Randomized Trials. New York: Oxford University Press, 1998. [ Links ]
9. Shamah-Levy, T, Morales-Ruán C, Amaya-Castellanos C, Salazar-Coronel A, Jiménez-Aguilar A, Méndez Gómez-Humarán I. Effectiveness of a diet and physical activity promotion strategy on the prevention of obesity in Mexican school children. BMC Public Health 2012;12(1):1-13 [accessed November 5, 2012]. Available at: http://www.biomedcentral.com/1471-2458/12/152. [ Links ]
10. Cole T, Bellizzi M, Flegal K, Dietz W. Establishing a Standard definition for child overweight and obesity worldwide: international survey. British Medical J 2000;320(7244):1240-1243. [ Links ]
11. Rodríguez S, Mundo V, Jiménez A, Shamah T. Methodology for the analysis of dietary data from the Mexican National Health and Nutrition Survey 2006. Salud Publica Mex 2009;51(4):S523-S529. [ Links ]
12. Bronfman M, Guiscafré H, Castro V, Castro R, Gutiérrez G. La medición de la desigualdad: una estrategia metodológica, análisis de las características socioeconómicas de la muestra. Arch Invest Med 1988;19:351-360. [ Links ]
13. Hernández B, Gortmarker S, Larid N, Colditz G, Parra-Cabrera S, Peterson K. Validez y reproductibilidad de un cuestionario de actividad e inactividad física para escolares de la Ciudad de México. Salud Publica Mex 2000;42(4):315-323. [ Links ]
14. Council on Sports Medicine and Fitness, Council on School Health. Active Healthy Living: Prevention of Childhood Obesity Through Increased Physical Activity. Pediatrics 2006;117(5):1834-1842. [ Links ]
15. Morales-Ruán MC, Hernández-Prado B, Gómez-Acosta LM, Shamah-Levy T, Cuevas-Nasu L. Obesity, overweight, screen time and physical activity in Mexican adolescents. Salud Publica Mex 2009;51(4):S613-S620. [ Links ]
16. American Academy of Pediatrics. Committee on Public Education. Media Violence. Pediatrics 2001;108:1222-1226. [ Links ]
17. Aedo A, Ávila H. Nuevo cuestionario para evaluar la auto eficacia hacia la actividad física en niños. Rev Panam Salud Publica 2009;26(4):324-329. [ Links ]
18. Norman GJ, Carlson JA, Sallis JF, Wagner N, Calfas KJ, Patrick K. Reliability and validity of brief psychosocial measures related to dietary behaviors. Int J Behav Nutr Phys Act 2010;7(1):56. [ Links ]
19. PACE PROGRAM. [website]. San Diego UC: Physician Assessment and Clinical Education program, Inc; 2008 [accessed July 25, 2011]. Available at: http://www.paceprogram.ucsd.edu/. [ Links ]
20. Bandura A. Self-efficacy: The exercise of control. New York: WH Freeman, 1997. [ Links ]
21. Ruiz VM, Berrocal C, López AE, Rivas T. Autoeficacia en el control de la conducta de ingesta. Adaptación al castellano de la Eating Self-Efficacy Scale. Psicothema 2003;15(1):36-40. [ Links ]
22. Johnson-Dallas E. Applied Multivariate Methods for Data Analysts. Belmont: Duxbury Press, 1998. [ Links ]
23. Ziegler A. Generalized Estimating Equations. New York: Springer Science+Business Media, LLC, 2011. [ Links ]
24. Selvin S. Statistical Analysis of Epidemiological Data. New York: Oxford, 2004. [ Links ]
25. Melendez G. Factores asociados con el sobrepeso y obesidad en el ambiente escolar. México: Médica Panamericana, 2008. [ Links ]
26. Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet 2002;360:473-482. [ Links ]
27. Government Office for Science. Foresight Tackling Obesities: Future Choices Project. [website]. United Kingdom: 2007 [accessed December 13, 2012]. Available at: http://www.bis.gov.uk/assets/foresight/docs/obesity/14.pdf. [ Links ]
28. Dehghan M, Akhtar-Danesh N, Merchant AT. Childhood obesity, prevalence and prevention. Nutr J 2005;4:24. [ Links ]
29. Lobstein T, Baur L, Uauy R, IASO International Obesity TaskForce. Obesity in children and young people: a crisis in public health. Obes Rev 2004;5(suppl 1):4-104. [ Links ]
30. Guedes DP, Rocha GD, Silva AJ, Carvalhal IM, Coelho, EM. Effects of social and environmental determinants on overweight and obesity among Brazilian schoolchildren from a developing region. Rev Pan Salud Pública 2011;30(4):295-302. [ Links ]
31. O'Malley PM, Johnston LD, Delva J, Bachman JG, Schulenberg JE. Variation in obesity among American secondary school students by school and school characteristics. Am J Preventive Medicine 2007;33(Suppl 4):S187-S194. [ Links ]
32. Summerbell CD, Waters E, Edmunds LD, Kelly S, Brown T, Campbell KJ. Intervenciones para prevenir la obesidad infantil (revisión Cochrane traducida). In: La Biblioteca Cochrane Plus, 2008 Number 4. Oxford: Update Software Ltd. (The Cochrane Library, 2008 Issue 3. Chichester, UK: John Wiley & Sons, Ltd.) [accessed: October 17, 2012]. Available at: http://www.update-software.com/.
33. Brown T, Summerbell C. Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: an update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obes Rev 2009;10(1):110-141. [ Links ]
34. Katz L. School-Based Interventions for Health Promotion and Weight Control: Not Just Waiting on the World to Change. Annu Rev Public Health 2009;30:253-272. [ Links ]
35. Shamah-Levy T, ed. Encuesta Nacional de Salud en Escolares 2008. Cuernavaca (Mexico): Instituto Nacional de Salud Pública, 2010. [ Links ]
Received on: April 24, 2013
Accepted on: April 23, 2014
 Corresponding author:
Corresponding author:
Dra. Teresa Shamah Levy.
Centro de Investigación en Nutrición y Salud,
Instituto Nacional de Salud Pública.
Av. Universidad 655, col. Santa María Ahuacatitlán.
62100 Cuernavaca, Morelos, México.
E-mail: tshamah@insp.mx
Declaration of conflict of interests. The authors declare that they have no conflict of interests.













