Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Salud Pública de México
Print version ISSN 0036-3634
Salud pública Méx vol.56 n.2 Cuernavaca Mar./Apr. 2014
Artículo original
Anthropometric parameters' cut-off points and predictive value for metabolic syndrome in women from Cartagena, Colombia
Puntos de corte y valor predictivo de medidas antropométricas para el síndrome metabólico en Cartagena, Colombia
Gustavo José Mora-García, MD,(1) Doris Gómez-Camargo, MSc, PhD,(1) Enrique Mazenett, MD, MSc,(2) Ángelo Alario, MD,(1) Álvaro Fortich, MD,(1) Claudio Gómez-Alegría, PhD.(3)
(1) Facultad de Medicina, Universidad de Cartagena. Cartagena de Indias, Colombia.
(2) Cooperativa de Salud y Desarrollo Integral de la Zona Sur Oriental de Cartagena (Coosalud), Entidad Promotora de Salud (EPS), Departamento Administrativo Distrital de Salud (DADIS). Cartagena de Indias, Colombia.
(3) Facultad de Ciencias, Universidad Nacional de Colombia. Bogotá, Colombia.
Abstract
Objective. To estimate anthropometric parameters' (APs) cut-off points and association for metabolic syndrome (MetS).
Materials and methods. A cross-sectional study was carried out with a total of 434 adult women from Cartagena de Indias, Colombia, in 2012. APs measured were waist circumference (WC), body mass index (BMI), body adiposity index (BAI), waist-hip ratio (WHR) and waist-height ratio (WHtR). Cut-off points were estimated by a receiver operating characteristic curve (ROC). Logistic regression was applied to estimate possible associations.
Results. Cut-off points for WC, BMI, BAI, WHR and WHtR were 85 cm, 28 kg/m2, 39%, 0.80 and 56, respectively. Only WHtR was associated to MetS (OR=1.11, CI95% [1.07-1.15]).
Conclusion. WC cut-off point was higher than those proposed for Latin-American women by the Joint Interim Statement (JIS). WHtR had a low predictive value for MetS.
Key words: obesity; abdominal obesity; body mass index; metabolic syndrome X; Caribbean region; Colombia.
Resumen
Objetivo. Estimar los puntos de corte y asociación de las medidas antropométricas para obesidad con el síndrome metabólico (SMet).
Material y métodos. Se realizó un estudio de corte transversal con 434 mujeres adultas, en Cartagena de Indias, Colombia, durante 20I2. Se midieron la circunferencia abdominal (CA), el índice de masa corporal (IMC), el índice de adiposidad corporal (IAC) y las razones cintura-cadera (RCC) y cintura-talla (RCT). Los puntos de corte fueron determinados mediante la curva ROC. La fuerza de asociación se estimó por regresión logística.
Resultados. Los puntos de corte para CA, IMC, IAC, RCC y RCT fueron, respectivamente, 85 cm, 28 kg/m2, 39%, 0.80 y 56. De los parámetros evaluados sólo RCT se asoció con SMet (OR= 1.11, IC95% [1.07-1.15]).
Conclusión. El punto de corte para circunferencia abdominal fue superior al reportado en América Latina, según el criterio de declaración provisional conjunta (JIS). La asociación de RCT con SMet fue baja.
Palabras clave: obesidad; obesidad abdominal; índice de masa corporal; síndrome X metabólico; región del Caribe; Colombia.
Metabolic syndrome (MetS) was initially described in 1988 as a hyperinsulinemic status associated to glucose intolerance, elevated plasma levels of free fatty acids and high blood pressure (HBP).1 Since then, continuous efforts have been carried out in order to develop a useful definition that allows a feasible assessment of the syndrome in a clinical context.2-4 A common key criteria in all definitions has been obesity, mainly defined as central and abdominal obesity.5
Assessment of obesity and its relation to insulin resistance has been controversial due to ethnic and environmental influences in metabolic responses to risk factors.6 In this regard, different waist circumference (WC) cut-off points for abdominal obesity were proposed, and only the International Diabetes Federation (IDF) considered ethnic differences in its MetS definition.4
A recent international consensus has proposed a unified MetS definition referred to as the Joint Interim Statement (JIS), which emphasizes the ethnic characteristics of the population, proposing to determine the cutoff points of waist circumference (WC) for each region and population.7
Asian and Latin American groups have suggested their particular WC cut-off points for abdominal obesity assessment in MetS.8,9 Although the Latin American study included Andean population from Colombia, it is still lacking of a cut-off value applied to the Colombian Caribbean region, a population with different ethnic and socio-demographic characteristics and a high prevalence of MetS.10,11 Also, due to the fact that measures for abdominal obesity vary between women and men, as it has been largely observed,2-5 it is necessary to estimate sex-specific cut-off points for WC in Caribbean coast population.
Even though WC has been widely applied as a practical definition for abdominal obesity, other anthropometric parameters (APs) such as body mass index (BMI), waist-hip ratio (WHR) and waist-height ratio (WHtR) have been employed to estimate body fat distribution and to predict disorders associated with MetS;12,13 moreover, a new body adiposity index (BAI) was recently developed in an attempt to rely on a better clinical tool for body percent adiposity estimation,14 but its significance for the diagnosis of obesity-related disorders remains unclear.15 In this regard, APs utility as indicators for insulin resistance and MetS remain a controversial issue; thus, to determinate their relevance on MetS approach it would be helpful to understand interactions between cardiovascular risks and their manifestations.16,17
With that in mind, the aim of this study was to estimate APs, cut-off points and predictive value for MetS in a population from Cartagena, on the Colombian Caribbean coast.
Materials and methods
A cross-sectional study was carried out on women from urban areas of Cartagena de Indias, Colombia, in 2012. Individuals aged 20-80 years were randomly selected through a cluster sampling, and invited to participate in our study by completing a medical examination by trained physicians, as it has been described in a previous report.10 According to the last national census, Cartagena accounts for 895 400 inhabitants, where women represent 50% of the population.18 With a 25% MetS prevalence,11 and a study error determined at 4.1, confidence interval at 95%, a minimum sample size was calculated to be 430 individuals, where sample size is the product of p*q*Z2 divided by d (p=0.25;(11) q=(1-p); Z=1.96; d=study error).19
Anamnesis and physical examination were employed to register sociodemographic and biophysical variables. APs catalogued as indicators for body fat distribution were WC, BMI, WHR, WHtR and BAI. Procedures for examination were performed according to IDF and JIS guidelines.4,7 Blood samples were drawn after a fasting period of 8-12 hours, and processed in our laboratory at Universidad de Cartagena within the first 2 hours. Serum biochemical parameters (glycemia, triglyceridemia and HDLc) were determined by colorimetric assays with appropriated reagent kits (Biosystems, Barcelona, Spain).
JIS criteria were followed to define MetS components.7 For analytical procedures, MetS was defined as the presence of two or more components, excluding central obesity criteria. Central tendency measurements were employed to describe data. A receiver operating characteristic curve (ROC) was applied to determine the cut-off point of APs for MetS and each of its associated disorders; also, area under the curve (AUC) comparisons were performed following the method described by De-Long and colleagues.20 Procedures were carried out with R 2.13.0 (Vienna, Austria),21 employing pROC 1.4.3 package for AUC calculation and comparisons, and Epi 1.1.20 package for plotting.22,23 A logistic regression model, fitted by age, using multivariable fractional polynomials (MFP) and reporting odds ratios (OR) was performed to estimate predictive values of APs on MetS and each of its associated disorders.24 MFP 1.4.9 package for R was employed for regression coefficients calculation.25 Calibration was assessed employing the Hosmer-Lemeshow test (HL), and a p>0.05 was interpreted as a statistically significant calibration of the model.26
This study was approved by the Universidad de Cartagena Bioethics Committee, and all participants gave their written informed consent.
Results
A total of 500 women were invited to participate in our study; 51 of them were excluded because they did not fulfill the minimal fasting time for biochemical serum assays (12 h); 15 additional patients reported missing values in their sociodemographic or biophysical data and they were also excluded. Finally, a total of 434 women participated in the present study. Age average was 47.2 ± 14.1 y, while means ± standard deviations for APs were: WC 88.2 ± 13.0 cm, BMI 26.9 ± 5.4 kg/m2, BAI 34.3 ± 7.3%, WHR 0.85 ± 0.08, WHtR 55.9 ± 8.8. Prevalence of MetS and its related disorders were: HBP 32.7% (CI95% [29.1 - 36.2]), high serum triglycerides levels 38.2% (CJ95% [34.5 - 41.9]), low serum HDLc 44.2% (CI95% [40.4 - 47.9]), High serum glucose levels 18.6% (CI95% [15.6 - 21.5]), and MetS 33.4% (CI95% [29.8 - 36.9]).
ROC curves with MetS as the outcome and APs as variables are represented in figure 1. WC cut-off points for HBP, high serum triglycerides, low HDLc, high serum glucose and MetS were 83, 83, 92, 85 and 85 cm, respectively. BMI cut-off points for HBP, high serum triglycerides, low HDLc, high serum glucose and MetS were 28, 24, 26, 28 and 28 kg/m2, respectively. BAI cut–off points for HBP, high serum triglycerides, low HDLc, high serum glucose and MetS were 34, 32, 39, 40 and 39%, respectively. WHR cut-off points for HBP, high serum triglycerides, low HDLc, high serum glucose and MetS were 0.83, 0.80, 0.76, 0.85 and 0.80, respectively. WHtR cut-off points for HBP, high serum triglycerides, low HDLc, high serum glucose and MetS were 52, 52, 46, 56 and 56, respectively (table I and figure 1). AUCs and their respective confidence intervals are represented in table I, while AUCs comparisons are illustrated in figure 2.
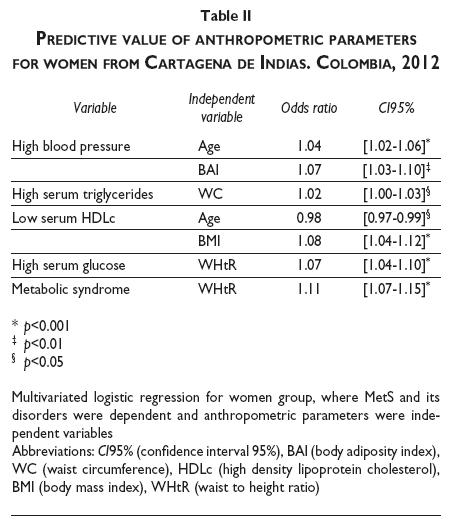
Concerning the APs as predictors of MetS and its disorders, we observed that ORs reported through logistic regression oscillated between 0.98 and 1.11, where MetS and its components were dependent variables while age and APs were independent variables. Instead of a unique predictor for the four MetS components, a heterogeneous behavior of APs was found in the regression model. In this regard, age was found as a predictor only for HBP (OR=1.04) and low serum HDLc; BAI was a predictor exclusively for HBP (OR=1.07); WC was a predictor solely for high serum triglycerides (OR=1.02); while BMI was a predictor for low serum HDLc (OR=1.08). In this sense, WHtR was the only AP correlated to two dependent variables, being predictor for high serum glucose (OR=1.07) and for MetS as a cluster (OR=1.11, table II).
Discussion
WC has been described as the best parameter to assess abdominal obesity in clinical practice. IDF proposed ethnic-specific WC thresholds as obligatory criteria in its MetS definition, and suggested a cut-off point ≥80 cm for South American women based on Asian studies until more specific data were available; in the same way, the JIS definition adopted IDF thresholds and recognized the need for ethnic-specific WC cut-offs.4,7
The WC cut-off point estimated here for MetS in women (85 cm) is higher than the point proposed previously in JIS guidelines for Latin American population (80 cm),7 however it is lower than the WC threshold for abdominal obesity (90-92 cm) recently found by Ashner and colleagues in South American women.9 Considering that Colombia is a country with ethnic variations and a diverse set of population phenotypes between regions, in particular between the Caribbean region and people from Andean cities (Bogotá, Bucaramanga, Medellín, among others),18 such differences in WC cut-off points could be attributed to ethnic influences on body fat distribution, as it has been also suggested by other authors.6
Additionally, WC cut-off points found here differ from those observed in a Brazilian cohort, where 80 cm (women) and 87 cm (men) were reported as the most sensible and specific points for HBP prediction;27 our results also diverge from a Mexican National Health survey where WC cut-off points for diabetes and HBP were 94-99 cm and 93-96 cm in women and men, respectively,28 showing a high diversity of cut-off points within Latin American population.
According to our results, WC AUC for MetS showed an acceptable discriminatory capacity (table I), even better than WHR ROC plot performance; moreover, none of the other APs here studied have shown a significantly larger AUC than WC when MetS was the classification variable (figure 2). These findings agree with JIS and WHO suggestion to employ WC as the criteria for abdominal obesity assessment in MetS approach.7,29
Given that MetS is a cluster of several alterations, we were concerned about the APs' performance in the diagnosis of every alteration included in the syndrome. In this regard, utility of APs to diagnose these alterations separately could provide a clinical tool in order to anticipate their clustering. However, APs' AUC showed small values when HBP, high serum triglycerides, low serum HDLc and high serum glucose were classificatory variables; although these observations discard their use for a single-alteration diagnosis in our population, ROC curve results allow us to conclude that APs would be useful for MetS assessment (table I, figure 2).
In 2011, Bergman and colleagues published the BAI as a new indicator of body percent adiposity. This index had a high concordance with x-ray based methods to estimate the proportion of body adiposity in men and women with Hispanic and Afro-American features.14 BAI has considerable advantages for its application in clinical practice, and possibly it will be a useful tool in regions where imaging devices are not easily available. However, in the present study the ROC curve analysis evidenced that BAI's AUC was not significantly superior to any other AP for MetS diagnosis (figure 2); this probably reflects the fact that this index is not specifically designed for abdominal obesity assessment. From this point of view, BAI would not be more appropriate than WC as the parameter for abdominal obesity definition in MetS. To our knowledge, this is the first evaluation of this index in Colombian population, and it would be hasty to make a definitive conclusion based on our results. Further studies are needed to evaluate its usefulness on obesity related disorders in order to clarify BAI's clinical meaning.
Concerning APs' predictive value for MetS, independent variables showed a heterogeneous behavior, and a unique predictor was not found in every alteration included in MetS cluster (table II). This phenomenon has been observed previously in Asians and in North Americans,16,17 where APs were suggested as predictors for peripheral vascular disease and insulin resistance in large case-control studies, but their usefulness was not constant to every MetS criteria. Similar findings were also reported in Peruvian population where no single AP was identified as the best MetS predictor.30
Although WHtR had a statistically significant result for MetS prediction, confidence interval values are close to the unit, indicating that only 7-15% of MetS cases would be predicted by WHtR.
Although findings in this study might suggest a higher WC cut-off point for MetS in women from Cartagena de Indias, application of new criteria should be confirmed by an external validation on an independent and comparable sample. Our results are only valid for adult women from Cartagena de Indias due to the nature of our sample. Currently, a larger study is being made by sampling people from three major cities of Colombia's Caribbean coast. According to our findings, a higher cut-off point for WC applicable to women in the entire region is expected to be observed. As a matter of fact, cut-off points based on ROC curve might diverge when different statistical approaches are applied in the same population; to avoid bias related to this, some authors suggest to employ Youden index to determine optimal cut-off points,31 as it was applied in this study. Although MetS has been the focus of a large discussion, in part due to the fact that the syndrome is based on categorical criterion created from continuous variables (i.e. glicemia, blood pressure), Royston and colleagues (2006) have pointed out that MFP applied to regression models would reduce bias attributable to dichotomization of continuous variables.24,32
In conclusion, APs' cut-off points in the Caribbean population from Cartagena are different to those proposed by IDF guidelines and JIS criteria, and also different from other Latin American groups.(7,9,28) Given that a single MetS predictor was not found, further studies focused on prevention of MetS and its alterations should be developed.
Acknowledgments
This work was partially supported by Vicerrectoría de Investigación Universidad de Cartagena (GCD) and Dirección Nacional de Investigación, Universidad Nacional de Colombia (DIB N° 8003115 to GAC). Mora-García GJ is supported by a Doctoral Fellowship from the Departamento Administrativo de Ciencia, Tecnología e Innovación de Colombia (Colciencias).
References
1. Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes I988;37(12):1595-607. [ Links ]
2. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106(25):3143-3421. [ Links ]
3. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome. An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Executive summary. Cardiology review 2005;13(6):322-327. [ Links ]
4. Alberti KG, Zimmet P, Shaw J. The metabolic syndrome--a new worldwide definition. Lancet 2005;366(9491):1059-1062. [ Links ]
5. Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part I: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 1998;15(7):539-553. [ Links ]
6. Bautista LE, Casas JP, Herrera VM, Miranda JJ, Perel P, Pichardo R, et al. The Latin American Consortium of Studies in Obesity (LASO). Obes Rev 2009;10(3):364-370. [ Links ]
7. Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009;120(I6):1640-1645. [ Links ]
8. Azizi F, Khalili D, Aghajani H, Esteghamati A, Hosseinpanah F, Delavari A, et al. Appropriate waist circumference cut-off points among Iranian adults: the first report of the Iranian National Committee of Obesity. Arch Iranian Med 20I0;13(3):243-244. [ Links ]
9. Aschner P, Buendia R, Brajkovich I, Gonzalez A, Figueredo R, Juarez XE, et al. Determination of the cutoff point for waist circumference that establishes the presence of abdominal obesity in Latin American men and women. Diabetes Res Clin Pract 2011;93(2):243-247. [ Links ]
10. Mora Garcia G, Salguedo Madrid G, Ruiz Diaz M, Ramos Clason E, Alario Bello A, Fortich A, et al. [Agreement between Five Definitions of Metabolic Syndrome: Cartagena, Colombia]. Rev Esp Salud Publica 2012;86(3):301-311. [ Links ]
11. Alayon AN, Ariza S, Baena K, Lambis L, Martinez L, Benitez L. [Active search and assessment of cardiovascular risk factors in young adults, Cartagena de Indias, 2007]. Biomedica 2010;30(2):238-244. [ Links ]
12. Shao J, Yu L, Shen X, Li D, Wang K. Waist-to-height ratio, an optimal predictor for obesity and metabolic syndrome in Chinese adults. J Nutr Health Aging 2010;14(9):782-785. [ Links ]
13. Wang F, Wu S, Song Y, Tang X, Marshall R, Liang M, et al. Waist circumference, body mass index and waist to hip ratio for prediction of the metabolic syndrome in Chinese. Nutr Metab Cardiovasc Dis 2009;19(8):542-547. [ Links ]
14. Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG, et al. A better index of body adiposity. Obesity (Silver Spring) 2011;19(5):1083-1089. [ Links ]
15. Snijder MB, Nicolaou M, van Valkengoed IG, Brewster LM, Stronks K. Newly proposed body adiposity index (bai) by Bergman et al. is not strongly related to cardiovascular health risk. Obesity (Silver Spring). 2012;20(6):1138-1139. [ Links ]
16. Chen CC, Wang WS, Chang HY, Liu JS, Chen YJ. Heterogeneity of body mass index, waist circumference, and waist-to-hip ratio in predicting obesity-related metabolic disorders for Taiwanese aged 35-64 y. Clin Nutr 2009;28(5):543-548. [ Links ]
17. Manu P, Tsang J, Napolitano BA, Lesser ML, Correll CU. Predictors of insulin resistance in the obese with metabolic syndrome. Eur J Intern Med 2010;21(5):409-413. [ Links ]
18. Departamento Administrativo Nacional de Estadística. Censo General de 2005. Libro Censo General. 1st ed. Bogotá: DANE, 2006. [ Links ]
19. Altman DG. Practical Statistics for Medical Research. London: Chapman and Hall, 1991:624. [ Links ]
20. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988;44(3):837-845. [ Links ]
21. R Development Core Team. R: A language and environment for statistical computing. Viena, Austria: R Foundation for Statistical Computing, 2013. [ Links ]
22. Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez JC, et al. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics 2011;12:77. [ Links ]
23. Plummer M, Carstensen B. An R Class for Epidemiological Studies with Long-Term Follow-Up. J Stat Softw 2011;38(5):1-12. [ Links ]
24. Royston P, Altman DG. Regression Using Fractional Polynomials of Continuous Covariates: Parsimonious Parametric Modelling. JR Stat Soc Ser C Appl Stat 1994;43(3):429-467. [ Links ]
25. Benner A. mfp-multivariable fractional polynomials. R News 2005;5:20-23. [ Links ]
26. Hosmer DW, Hosmer T, Le Cessie S, Lemeshow S. A comparison of goodness-of-fit tests for the logistic regression model. Statistics in medicine I997;16(9):965-980. [ Links ]
27. Gus M, Cichelero FT, Moreira CM, Escobar GF, Moreira LB, Wiehe M, et al. Waist circumference cut-off values to predict the incidence of hypertension: an estimation from a Brazilian population-based cohort. Nutr Metab Cardiovasc Dis 2009;19(1):15-19. [ Links ]
28. Sanchez-Castillo CP, Velazquez-Monroy O, Berber A, Lara-Esqueda A, Tapia-Conyer R, James WP. Anthropometric cutoff points for predicting chronic diseases in the Mexican National Health Survey 2000. Obes Res 2003;11(3):442-451. [ Links ]
29. Simmons RK, Alberti KG, Gale EA, Colagiuri S, Tuomilehto J, Qiao Q, et al. The metabolic syndrome: useful concept or clinical tool? Report of a WHO Expert Consultation. Diabetologia 2010;53(4):600-605. [ Links ]
30. Knowles KM, Paiva LL, Sanchez SE, Revilla L, Lopez T, Yasuda MB, et al. Waist Circumference, Body Mass Index, and Other Measures of Adiposity in Predicting Cardiovascular Disease Risk Factors among Peruvian Adults. Int J Hypertens 2011;2011:931402. [ Links ]
31. Perkins NJ, Schisterman EF. The inconsistency of "optimal" cutpoints obtained using two criteria based on the receiver operating characteristic curve. Am J Epidemiol 2006;163(7):670-675. [ Links ]
32. Royston P, Altman DG, Sauerbrei W. Dichotomizing continuous predictors in multiple regression: a bad idea. Statistics in medicine 2006;25(1):127-141. [ Links ]
Received on: April 15, 2013
Accepted on: January 22, 2014
 Corresponding author:
Corresponding author:
Dr. Claudio Gómez-Alegría.
Universidad Nacional de Colombia.
Cra. 30 # 45-03, Ciudad Universitaria, edificio 450. Bogotá, Colombia
E-mail: cjgomeza@unal.edu.co
Declaration of conflict of interests. The authors declare that they have no conflict of interests.













