Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Salud Pública de México
Print version ISSN 0036-3634
Salud pública Méx vol.55 suppl.3 Cuernavaca 2013
Artículo original
Targeting children's dietary behaviors in a family intervention: 'Entre familia: reflejos de salud'
Enfoque en hábitos alimenticios de los hijos en una intervención familiar: 'Entre familia: reflejos de salud'
Lucy A Horton, MPH, MS,(1) Humberto Parada, MPH,(1) Donald J Slymen, PhD,(2) Elva Arredondo, PhD,(1,2) Leticia Ibarra, MPH,(3) Guadalupe X Ayala PhD, MPH, MA.(1,2)
(1) Institute for Behavioral & Community Health, San Diego State University Research Foundation. San Diego, CA, USA.
(2) San Diego State University. San Diego, CA, USA.
(3) Clínicas de Salud del Pueblo, Inc. Brawley, CA, USA.
Abstract
Objective. This intervention sought to promote healthy eating with the ultimate goal of reducing childhood obesity risk.
Materials and methods. Three hundred and sixty-one Latino families living on the US-Mexico border with at least one child between 7-13 years of age were eligible to participate. Families randomly assigned to the four-month intervention received 14 contacts with a promotora (community health worker), consisting of 11 home visits and three telephone calls; the control condition was a delayed treatment intervention. Children reported on their dietary intake at baseline, immediately post-intervention and at the six month follow-up visit.
Results. The intervention reduced weekly consumption of fast food (p<0.05). A dose-response relationship was observed such that for every seven hours of promotora contact, monthly variety of fruits (p<0.01) and vegetables (p<0.01) increased by one. No other intervention effects were observed.
Conclusions. Family-based interventions can improve children's eating habits, with the amount of contact with the promotora being key to success.
Key words: diet; Mexican Americans; child; intervention; community health workers.
Resumen
Objetivo. Promover una alimentación saludable con el objetivo final de reducir el riesgo de obesidad infantil.
Material y métodos. Trescientas sesenta y una familias latinas que viven en la frontera de EU y México, y que cuentan con por lo menos un hijo entre 7 y 13 años, fueron elegibles para participar. Las familias asignadas al azar a la intervención de cuatro meses tuvieron contacto 14 veces (11 visitas familiares y tres llamadas telefónicas) con una promotora; el grupo de control recibió el tratamiento de intervención al final del programa. Los niños reportaron su ingesta alimenticia al inicio, inmediatamente después de la intervención y en la visita de seguimiento a los seis meses.
Resultados. La intervención redujo el consumo semanal de comida rápida (p<0.05). Se observó una relación dosis-respuesta tal que por cada siete horas de contacto con la promotora, la variedad mensual de frutas (p<0.01) y verduras (p<0.01) tuvo un incremento de uno. No se observaron otros efectos de intervención.
Conclusiones. Las intervenciones basadas en la familia pueden mejorar los hábitos alimenticios de los niños, siendo la cantidad de contacto con la promotora clave para el éxito.
Palabras clave: dieta; americanos mexicanos; niño; intervención; agentes comunitarios de salud.
The Hispanic population in the US has a higher risk of certain preventable diseases such as diabetes1 and some forms of cancer2 compared to non-Hispanic Black, non-Hispanic White, and other population groups. Recent data suggest that Mexican-American children display higher rates of overweight and obesity compared to other Hispanic and non-Hispanic White groups,3 which may further predispose them to these diseases later in life. Healthy eating plays an important role in preventing and managing these health challenges, particularly the intake of fruits and vegetables and foods low in fat, salt and sugar. Although rates of fruit and vegetable intake in this population are higher than the US population as a whole,4 intake regularly does not meet national US guidelines.5 In addition, a systematic review on the association between the process of acculturation and diet suggests that fruit and vegetable consumption decreases the longer Hispanic families live in the US.6 Given that most of this research has been conducted with the Mexican origin population living in the US, this provides further evidence for the need to intervene before health consequences are realized.
The promotion of healthy eating within Mexican origin families, through the implementation of culturally sensitive interventions, is therefore a priority to reduce health disparities. Culturally sensitive interventions are those that consider the attitudes, behaviors, and preferences of the target population in their design (e.g., the emphasis on family responsibility in the Hispanic community).7 Culturally sensitive interventions are more effective at achieving behavior and health status changes compared with those that are not culturally sensitive, in part, because of their ability to engage the population in a meaningful way.8
Promotora-based health promotion interventions
Promotora-based interventions within the Mexican immigrant/Mexican-American community have been applied to a wide variety of health issues.9 Along the Arizona, US and Sonora, Mexico border region for example, Hunter et al. (2004) saw increased uptake of preventative health screenings among women who received one promotora visit, compared to those who received no visit.10 Other positive health outcomes observed using the promotora model include increased HIV knowledge and awareness among Latinos in Chicago, US,11 and improved physical activity in Mexican-Americans in Detroit, US.12
Family-based promotora healthy eating interventions
Family-based interventions acknowledge the importance of family in the Latino culture such as family support, obligation and cohesion.13,14 Targeting the family has been shown to positively influence health knowledge, attitudes and behaviors in Latinos and several interventions, although not always having healthy eating as a primary outcome, have included measures of dietary intake and/or behaviors.15-21 For example, one study targeted the extended family (including friends) of Latino diabetes patients using a promotora-based intervention delivered in the patient's home. The intervention, which addressed food choices, physical activity and communication through the use of pictures, games, food-based and physical activities, was successful at increasing diabetes knowledge and family efficacy to change food and activity behaviors. This study, however, lacked a control condition.20 Cronk et al. (2011) conducted a family-based multicomponent intervention delivered in a community health center and observed decreases in child BMI, increases in parent fitness, and increases in quality of life scores for both children and parents compared to the control condition.16 Similarly, participants of a nutrition intervention for Latina women18 were randomly assigned to one of the following conditions: promotora visits and mailed tailored newsletters; mailed tailored newsletters only; or mailed culturally-targeted newsletters. Fewer barriers to eating diets high in fruits and vegetables and promoting healthy dietary practices in the family were noted in the former intervention group compared to the latter two groups. Additionally, post-intervention results showed positive health behaviors such as lower intakes of total fat and energy intake in the former group. These results, however, were not sustained one-year post-intervention.18
Fewer home-based promotora studies have been conducted which focus on the health of children. As part of a 2x2 factorial group randomized controlled trial, participating families received a promotora-based intervention in their homes to promote healthy eating and physical activity among children and healthy parenting skills in the parents. Mothers receiving the intervention reported changes in parenting such as more frequent monitoring of their child's diet and physical activity, and reduced consumption of away-from-home foods.15 Additionally, increases in child fruit and vegetable intake and behavioral strategies to reduce fat were observed in the intervention condition two years post-baseline.21
Despite the growing body of research on effective Latino family-based interventions, few studies have looked at the effects of these interventions on Latino children. Given the higher rates of overweight and obesity in Mexican-American children compared to other Hispanic and white non-Hispanic groups,3 the present study sought to build evidence in this area to broaden knowledge on effective strategies to promote healthy eating in the Mexican immigrant/Mexican-American population.
Present study
The Entre Familia study was a randomized controlled trial comparing the efficacy of a family-based intervention aimed at promoting healthy eating (specifically fruit and vegetable intake) to a delayed treatment control condition. The home-based intervention was delivered by promotoras to Mexican immigrant/Mexican-American families living on the US-Mexico border.
The intervention included the use of a culturally-specific telenovela (based on documented effectiveness in past Latino-focused interventions)22 and accompanying family manual, and was designed to include as many family members as possible. The telenovela cast represented the border population in terms of ethnic and racial background (Mexican origin families). The intervention materials were written following formative research with the target population so as to reflect the beliefs, behaviors, values, and other characteristics common to those involved (such as the important role of family in Mexican culture). The model used in the present study involved promotoras who were members of the same communities as the participants and thus were intimately aware of the barriers to healthy eating in these communities and how to surmount these barriers.
The present study describes the development, implementation, and immediate post-intervention effects of this intervention on child-reported dietary intake, specifically fruits and vegetables, fast food, and sugar-sweetened beverage consumption.
Materials and methods
Setting
This study was conducted in Imperial County, CA, along the US-Mexico border. Imperial County is characterized by nationally high poverty rates,23 and among the highest childhood obesity rates in California.24 Intervention activities were delivered through Clínicas de Salud del Pueblo, Inc. (CDSDP), a federally-qualified community health center serving residents of Imperial and Riverside counties.
Study design
Latino families were randomly assigned to a family-based promotora-delivered nutrition intervention or a delayed treatment control condition.
Recruitment of study participants
Between May 2009 and February 2011, a convenience sample of 361 mothers and their children were recruited using a variety of methods including newspaper advertisements, solicitation at health fairs, and letters mailed to parents of pediatric patients of CDSDP. Fathers were recruited in 25% of the families to complete the assessment protocol. Families were eligible to participate if the mother was at least 18 years of age and married or living with a partner, if she was fluent in Spanish and considered herself Latina, if she had a child residing in the home who was between 7 and 13 years of age, and if the family resided in Imperial County and had no plans to move in the next 10 months. Families were excluded if any member of the family was on a medically-prescribed diet.
All study activities were approved by the Institutional Review Board at San Diego State University and informed consent (mother) and assent (child) were obtained prior to participation in study activities. In addition, research assistants and promotoras were required to complete ethics training at CDSDP to ensure the Health Insurance Portability and Accountability Act (HIPAA) requirements.
Intervention development and delivery
The Entre Familia intervention was developed following extensive formative research with the target population and a systematic review of the literature on family-based interventions to promote healthy eating.25 Focus groups and in-depth interviews with the target population were instrumental in designing a Spanish-language nine-part DVD television series (similar to a telenovela) that depicted the lives of a family trying to make healthy dietary changes. The production company (Spectrum Advertising) worked with the research team to identify Mexican actors to ensure that they were similar to the target community. A Spanish-language family manual was designed to accompany the DVD series and included goal setting sheets, skill building activities, and a variety of other parent- and child-focused activities (table I).
In addition to the DVD and family manual, the research team trained six promotoras to deliver the intervention using a 13-part promotora training manual. Parts 1-3 of the training provided an overview of the study, how to promote healthy eating, and effective strategies for working with families and conducting home visits. The remaining training sessions were designed to parallel the home visits to provide the promotoras with the opportunity to experience the intervention as participants, as well as practice their skills promoting family-based behavior change. Promotoras were recruited from among female volunteers of CDSDP, interviewed and then selected based on their experience and interest in promoting family behavior change. They were employed by CDSDP on a part-time basis.
After completing the baseline assessment, families were randomly assigned to an intervention or control (delayed treatment) condition. Intervention families were contacted by an assigned promotora first by letter and then by telephone to schedule the introductory home visit. The home visits were designed to include as many family members as possible to foster family support for healthy eating and to maximize sustainability of family behavior change. Intervention families were visited once a week for two months, followed by biweekly home visits during the third month with telephone calls on non-visit weeks, and a final home visit and telephone call during the fourth month. Tapering of intervention delivery was designed to facilitate independence from the promotora. The intended dose was 16 ½ hours or 990 minutes and was tracked on weekly progress reports submitted by the promotoras. Control families received the DVD series and family manual after completing the final assessment protocol.
Evaluation procedure
Bilingual and bicultural research assistants were trained to collect data from mothers, fathers and children (the former two are not described in detail here). Interested families received a telephone call from the research assistant to schedule a baseline home visit. The baseline assessment included independent interviews with the parents and the selected child, followed by measurement of their height and weight to calculate body mass index percentile. Similar procedures were used at post-intervention and at the 6-month follow-up (the latter is not described here).
Materials
The child interview guide was designed to be short and was available in Spanish or English, with children given the preference to have the interview conducted in either language.
Daily fruit and vegetable intake was assessed with two questions from the National Cancer Institute Food Attitudes and Behavior survey.26 Children were asked how many cups of fruits and how many cups of vegetables they consume on a daily basis, with several examples provided on how much is a cup. Fruit and vegetable variety was assessed by asking children whether they had consumed any of 30 fruits and 44 vegetables in the past month. To facilitate recall on produce items that may not be known by name, pictures of all 74 produce items were presented to the child during the recall process. A summary score was computed representing the total variety of fruits and vegetables consumed during the past month. Daily servings of sugar-sweetened beverages was assessed by one question on number of cans or glasses of sugar-sweetened beverages consumed daily. Weekly fast food consumption was assessed by asking how many days they ate fast food in a typical week.27
Demographic information was obtained including the child's age, gender, country of origin and level of acculturation using the Bidimensional Acculturation scale.28 Additional demographic information was obtained during the mothers' interview including assessment of mother's marital status and country of origin, household size, monthly household income, whether the family is on any type of food assistance, and whether they own their home.
Data analyses
Data management and initial comparisons of baseline measures between groups were conducted using SPSS Version 18. T-tests for continuous variables and chi-square tests for categorical variables were used to identify any differences between conditions.
With a few exceptions, analysis of covariance (ANCOVA) using PROC GLM on SAS Version 9.2 was used to compare the intervention and control conditions on the child outcomes at post-intervention adjusting for the corresponding baseline measure as well as mother's race, education, and marital status. For daily servings of sugar-sweetened beverages and days per week consuming fast food, negative binomial models for count data were better fits for the distributions. Therefore, negative binomial regression, as a specified model within generalized linear models was used with PROC GENMOD in SAS. All significance tests used an alpha level of 0.05. A dose response relationship was tested using number of minutes of contact between the promotora and the child participant. In order to provide a more meaningful time interval for interpretation, results are presented based on a 420 minute (or 7 hours) increase in contact time which is very close to the underlying standard deviation.
Results
Participant characteristics and retention rates
Table II shows descriptive statistics for children and households participating in the study, by intervention condition. In regard to both child and household demographic variables, the control condition had significantly more single mothers than the intervention condition (χ2 = 3.71, p<0.05). In addition, mother's race and education were significantly associated with child's fruit and vegetable intake (both p<0.05).

Figure 1 shows the Consolidated Standards of Reporting Trials (CONSORT) flow diagram for recruitment and retention of children. Of the 701 families who were assessed for eligibility, 36% (249) were ineligible. From among 452 eligible families, 20% (91) declined to participate. Three hundred and sixty-one families were randomized to receive the intervention (50%, 180) or the delayed treatment (50%, 181). At the 4-month post-intervention assessment, 21 (12%) of the intervention families were lost to follow-up compared with 17 (9%) in the delayed treatment group. This resulted in retention rates of 88% in the intervention condition and 91% in the control condition.
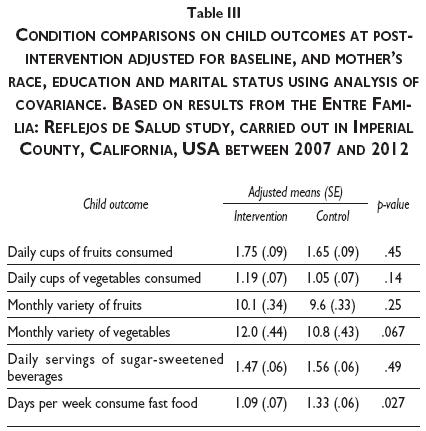
Family size was examined as a potential moderator by adding an interaction term with condition in each model for the six child outcomes of table III. None were found to be statistically significant. Additionally, an evaluation of baseline differences was carried out between those who completed the study and those who dropped out on the child characteristics listed in table II and on baseline levels of the outcomes in table III. Wilcoxon rank-sum tests were carried out for continuous variables and either chi-square or Fisher's exact test for categorical variables. None of the variables were found to be statistically significant at the 0.05 level.
Intervention effects
As shown in table III, intervention effects were observed on weekly fast food consumption (p<0.05) and trends were observed in increases in monthly variety of vegetables (p<0.07). Regarding the former, children in the intervention condition reported consuming fast food on fewer days in a typical week at follow-up. Regarding the latter, intervention children compared with control children reported consuming one additional variety of vegetables in the past month at follow-up. Finally, although not statistically significant, the intervention children reported consuming 0.14 more daily cups of vegetables compared with control children. If sustained over seven days, this increase would translate to approximately one additional cup of vegetables per week. No other intervention effects were observed.
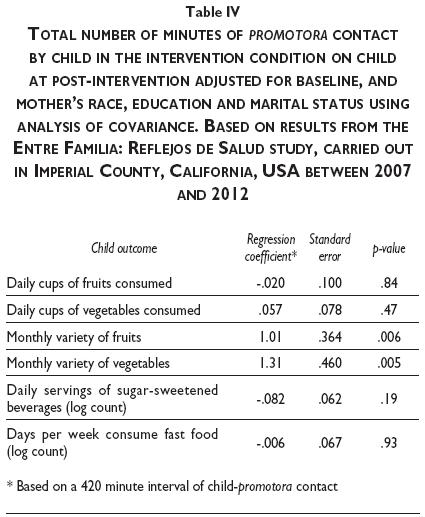
Dose response relationship
A significant dose-response relationship was observed for monthly variety of fruits and monthly variety of vegetables (table IV). For every 420 minutes (approximately 7 hours) of contact the children had with the promotora, the children reported consuming one additional variety of fruit (p<0.01) and one additional variety of vegetables (p<0.01) in the past month. No other dose response relationships were observed.
Discussion
Promotora-based interventions have proven successful in effecting health behavior change in the Latino community.15-21 The present study sought to address a gap in the literature by examining changes in Latino child health behavior outcomes resulting from a promotora-delivered home-based intervention. Significant intervention effects were observed for consumption of fast food– at post-intervention, children in the intervention condition consumed fast food on significantly fewer days of the week compared to the control condition. Although not statistically significant, children in the intervention condition ate a greater monthly variety of vegetables than children in the control condition. Finally, there was an association between increased promotora contact and child consumption of a greater variety of both fruits and vegetables per month.
Limited research is available on promotora-based interventions targeting healthy eating in Latino children. However home-based family interventions have been used for many years29,30 to successfully target changes in nutritional intake.15,31,32 For example a similar intervention study comprising of 10 home visits delivered by family advisors to parents and children facilitated movement toward achieving a family weekly nutrition goal, with more advisor time associated with higher family engagement and achievement of these goals.32 The study presented here highlights the need for further understanding into the efficacy of interventions to improve healthy eating in Latino children as a strategy to promote health, and reduce overweight and obesity risk.
Study limitations
Certain limitations exist within this study. Convenience sampling may have resulted in the recruitment of families motivated to change their behaviors.33 Dietary intake was assessed using several brief scales to minimize respondent burden and ensure an interview guide that could be administered to children as young as seven years old. However, future studies should consider more rigorous methods for assessing diet such as 24-hour dietary recalls, or a combination of different dietary assessment methods to minimize measurement error as a possible explanation for the minimal intervention effects observed.34 It is also acknowledged that interview responses could have been affected by social desirability bias such as underreporting of overall dietary intake, a documented limitation of administering self-report surveys to children.35 Control families could have been exposed to the intervention given that intervention families retained their family manuals to use in-between promotora visits. We weighed their use more favorably than risk of exposure to control families and recognize this as a possible limitation. However, we did not leave the DVDs with the families as we felt the risk of sharing was too high given their entertaining value. Finally, more significant changes in these dietary patterns may have been observed with a more intense intervention.
Future research
Understanding the longer-term intervention effects is important given the need to identify methods to sustain health behavior change to reduce health disparities. In addition, this group of researchers is now involved in the CDC-funded Childhood Obesity Research Demonstration (CORD) study that is testing system, environmental and policy intervention strategies to promote childhood obesity prevention and control. A more intense version of the Entre Familia study is being adapted for integration into a community health center to compliment other activities that are happening in schools, child care centers, restaurants, and community recreation outlets to promote healthy eating physical activity, water intake, and sleep. This would contribute to reducing health disparities between American population subgroups, an objective of Healthy People 2010.36
Acknowledgements
This research was supported by a grant to Dr. Ayala from the American Cancer Society (RSGPB 113653). The authors wish to thank the promotoras who provided critical feedback in the development of the intervention and the families for their participation in the study.
References
1. Narayan K, Boyle J, Thompson T, Sorensen S, Williamson D. Lifetime risk for diabetes mellitus in the United States. JAMA 2003;290:1884-1890. [ Links ]
2. American Cancer Society. Cancer facts and figures for Hispanics/Latinos 2009-2011. 2012 [Accessed 2012 August 01]. Available in: http://www.cancer.org/acs/groups/content/@nho/documents/document/ffhispanicslatinos20092011.pdf [ Links ]
3. Forum on child and family statistics. Percentage of children ages 6-17 who are obese by race and Hispanic origin, age and gender, selected years 1976-2010. 2012 [Accessed 2012 July 29]. Available in:http://www.childstats.gov/americaschildren/tables.asp. [ Links ]
4. Duffey KJ, Gordon-Larsen P, Ayala GX, Popkin BM. Birthplace is associated with more adverse dietary profiles for US-born than for foreign-born Latino adults. J Nutr 2008;138:2428-2435. [ Links ]
5. Centers for Disease Control and Prevention. Prevalence of fruit and vegetable consumption and physical activity by race/ethnicity - United States, 2005. 2007 [Accessed 2011 June 17]. Available in: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5613a2.htm. [ Links ]
6. Ayala GX, Baquero B, Klinger S. A systematic review of the relationship between acculturation and diet among Latinos in the United States: implications for future research. J Am Diet Assoc 2008;108(8):1330-1344. [ Links ]
7. Elder JP, Ayala GX, Parra-Medina D, Talavera GA. Health communication in the Latino community: issues and approaches. Annu Rev Publ Health 2009; 30:227-251. [ Links ]
8. Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethnic Dis 1999;9(1):10-21. [ Links ]
9. Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos: a qualitative systematic review. Am J Prev Med 2007;33(5):418-427. [ Links ]
10. Hunter JB, de Zapien JG, Papenfuss M, Fernandez ML, Meister J, Giuliano AR. The impact of a promotora on increasing routine chronic disease prevention among women aged 40 and older at the U.S.-Mexico border. Health Educ Behav 2004;31 suppl 4:18S-28S. [ Links ]
11. Martin M, Camargo M, Ramos L, Lauderdale D, Krueger K, Lantos J. The evaluation of a Latino community health worker HIV prevention program. Hispanic J Behav Sci 2005;27(3):371-384. [ Links ]
12. Nies M, Artinian NT, Schim SM, Vander-Wal JS, Sherrick-Escamilla S. Effects of lay health educator interventions on activity, diet, and health risks in an urban Mexican American community. J Prim Prev 2004;25(4):441-455. [ Links ]
13. Sabogal F, Marín G, Otero-Sabogal R, Marín B, Perez-Stable EJ. Hispanic familsm and acculturation: what changes and what doesn't? Hispanic J Behav Sci 1987;9(4):397-412. [ Links ]
14. Elder JP, Ayala GX, Parra-Medina D, Talavera G. Health communication in the Latino community: issues and approaches. Annu Rev Public Health 2009;30:227-251. [ Links ]
15. Ayala GX, Elder JP, Campbell NR, Arredondo E, Baquero B, Crespo NC, et al. Longitudinal intervention effects on parenting of the Aventuras para Niños study. Am J Prev Med 2010;38(2):154-162. [ Links ]
16. Cronk C, Hoffmann R, Mueller M, Zerpa-Uriona V, Dasgupta M, Enriquez F. Effects of a culturally tailored intervention on changes in body mass index and health-related quality of life of Latino children and their parents. Am J Health Promot 2011;25(4):e1-e11. [ Links ]
17. Dreimane D, Safani D, MacKenzie M, Halvorson M, Braun S, Conrad B, et al. Feasibility of a hospital-based, family-centered intervention to reduce weight gain in overweight children and adolescents. Diabetes Res Clin Pract 2007;75(2):159-168. [ Links ]
18. Elder JP, Ayala GX, Slymen DJ, Arredondo EM, Campbell NR. Evaluating psychosocial and behavioral mechanisms of change in a tailored communication intervention. Health Educ Behav 2009;36(2):366-380. [ Links ]
19. Nader PR, Sallis JF, Patterson TL, Abramson IS, Rupp JW, Senn KL, et al. A family approach to cardiovascular risk reduction: results from the San Diego Family health project. Health Educ Quart 1989;16(2):229-244. [ Links ]
20. Teufel-Shone NI, Drummond R, Rawiel U. Developing and adapting a family-based diabetes program at the U.S.-Mexico border. Prev Chronic Dis 2005;2(1):A20. [ Links ]
21. Crespo N, Elder JP, Ayala GX, Slymen DJ, Campbell NR, Sallis JF, et al. Results of a multi-level intervention to prevent and control childhood obesity among Latino children: The Aventuras para Niños study. Ann Behav Med 2012;43(1):84-100. [ Links ]
22. Wilkin H, Valente T, Murphy S, Cody M, Huang G. Does entertainment education work with Latinos in the United States? Identification and the effects of a telenovela breast cancer storyline. Health Commun 2007;21(3):223-233. [ Links ]
23. U.S. Census Bureau, 2006-2010 American Community Survey. Poverty status in the past 12 months. 2012 [Accessed 2012 August 01]. Available in: http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_10_1YR_S1701&prodType=table [ Links ]
24. UCLA Center for Health Policy Research and California Center for Public Health Advocacy. A patchwork of progress: changes in overweight and obesity among California 5th, 7th, and 9th graders, 2005-2010. 2011 [Accessed 2012 August 01]. Available in: http://www.healthpolicy.ucla.edu/pubs/files/PatchworkStudy.pdf [ Links ]
25. Ayala G, Ibarra L, Arredondo E, Horton L, Hernandez E, Parada H, et al. Promoting healthy eating by strengthening family relations: design and implementation of the Entre Familia: Reflejos de Salud intervention. In: Elk R, Landrine H, eds. Cancer Disparities: Causes and Evidence-Based Solutions. Springer US 2011:237- [ Links ]252.
26. Blanck H, Thompson O, Nebeling L, Yaroch A. Improving fruit and vegetable consumption: use of farm-to-consumer venues among US adults. Prev Chronic Dis 2011;8(2):A49. [ Links ]
27. Ayala G, Rogers M, Arredondo E, Campbell N, Baquero B, Duerksen S, et al. Away-from-home food intake and risk for obesity: examining the influence of context. Obes Res 2008;16(2):1002-1008. [ Links ]
28. Marin G, Gamba RJ. A new measurement of acculturation for Hispanics: the bidimensional acculturation scale for Hispanics (BAS). Hisp J Behav Sci 1996;18(3):297-316. [ Links ]
29. Epstein L, Paluch R, Roemmich J, Beecher M. Family-based obesity treatment, then and now: twenty-five years of pediatric obesity treatment. Health Psychol 2007;26(4):381-391. [ Links ]
30. Kitzmann KM, Beech BM. Family-based interventions for pediatric obesity: methodological and conceptual challenges from family psychology. J Fam Psychol 2006;20(2):175-189. [ Links ]
31. Harrington KF, Franklin F, Davies SL, Shewchuk RM, Binns MB. Implementation of a family intervention to increase fruit and vegetable intake: the Hi5+ experience. Health Promot Pract 2005;6(2):180-189. [ Links ]
32. Heimendinger J, Uyeki T, Andhara A, Marshall J, Scarbro S, Belansky E, et al. Coaching process outcomes of a family visit nutrition and physical activity intervention. Health Educ Behav 2007;34(1):71-89. [ Links ]
33. Sousa VD, Zauszniewski JA, Musil CM. How to determine whether a convenience sample represents the population. Appl Nurs Res 2004;17(2):130-133. [ Links ]
34. Livingstone MBE, Robson PJ. Measurement of dietary intake in children. Proc Nutr Soc 2000:59(2);279-293. [ Links ]
35. Sherwood NE. Diet assessment in children and adolescents. In: Jelalian E, Steele RG, eds. Handbook of childhood and adolescent obesity. New York: Springer US, 2009:73-89. [ Links ]
36. U.S. Dep. Health Hum. Serv. Healthy people 2010: understanding and improving health. [Internet]. 2000 [Accessed 2011 May 10]. Available from: http://www.healthypeople.gov/Document/tableofcontents.htm. [ Links ]
Received on: March 14, 2012
Accepted on: September 19, 2012
 Corresponding author:
Corresponding author:
Guadalupe X. Ayala.
San Diego State University. 5500 Campanile Drive, San Diego, CA 92182, USA.
E-mail: ayala@mail.sdsu.edu
Declaration of conflict of interests: The authors declare not to have conflict of interests.













