Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Salud Pública de México
Print version ISSN 0036-3634
Salud pública Méx vol.55 suppl.1 Cuernavaca Jul. 2013
REVIEW ARTICLE
Systematic review of HIV prevalence studies among key populations in Latin America and the Caribbean
Revisión sistemática de estudios de prevalencia del VIH en poblaciones clave de mayor riesgo en América Latina y el Caribe
William Meihack Miller, MPHI; Lindsay Buckingham, BAII; Mario Salvador Sánchez-Domínguez, MvD, MScIII; Sonia Morales-Miranda, MVD, MScI; Gabriela Paz-Bailey, MD, MSc, PhD.I, II, IV
IUniversidad del Valle de Guatemala. Guatemala
IISchool of Medicine, University of North Carolina at Chapel Hill. North Carolina, USA
IIIInstituto Nacional de Salud Pública. Cuernavaca, Morelos, México
IVTephinet, Inc. Guatemala
ABSTRACT
OBJECTIVE: This systematic review aims to synthesize articles, abstracts and reports of HIV prevalence studies conducted among men who have sex with men (MSM) and female sex workers (FSW) in Latin America and the Caribbean (LAC).
MATERIALS AND METHODS: Authors searched online databases and collected gray literature on HIV prevalence among MSM and FSW from LAC. Year, location, sampling methodology, study design, sample size, HIV prevalence and confidence intervals were abstracted.
RESULTS: A total of 73 studies, dating from 1986 to 2010 were included.The median prevalences for MSM and FSW were 10.6% (interquartile range: 7.4- 17.4) and 2.6% (IQR: 0.6 -4.2), respectively. Variability was high, especially for MSM. The majority of studies recruited participants using convenience methods.
CONCLUSION: HIV prevalence among MSM was higher than that among FSW. Sampling techniques should be standardized for future studies, prioritizing probability methods.
Key words: HIV; vulnerable populations; Latin America; Caribbean region
RESUMEN
OBJETIVO: Esta revisión sistemática tiene el objetivo de sintetizar artículos, resúmenes y reportes de estudios de prevalencia de VIH en hombres que tienen sexo con hombres (HSH) y mujeres trabajadoras sexuales (MTS) en América Latina y el Caribe (ALC).
MATERIAL Y MÉTODOS: Se realizaron búsquedas en bases de datos electrónicas y se recopiló literatura gris sobre la prevalencia de VIH en HSH y MTS de América Latina y el Caribe. Los datos recolectados fueron año, lugar, metodología de muestreo, diseño del estudio, tamaño muestral, prevalencia de VIH e intervalos de confianza.
RESULTADOS: Se incluyó un total de 73 estudios, realizados de 1986 a 2010. La mediana de la prevalencia para HSH y MTS fue 10.6% (rango intercuartil: 7.4- 17.4) y 2.6% (RIC: 0.6-4.2), respectivamente. La variabilidad de las prevalencias estimadas fue alta, especialmente para HSH. La mayoría de estudios usaron muestras por conveniencia.
CONCLUSIONES: La prevalencia de VIH entre HSH es superior a MTS. Los métodos muestrales deben ser estandarizados para estudios futuros, priorizando métodos probabilísticos.
Palabras clave: VIH; poblaciones vulnerables; América Latina; región del Caribe
HIV/AIDS continues to be a pressing public health problem around the world. The Joint United Nations Programme on HIV/AIDS (UNAIDS) recently reported that in 2010 33.3 million people were infected, while in 2009 1.8 million deaths occurred as a result of HIV worldwide. Since new infections peaked in 1999, UNAIDS estimates a 19% decrease in new infections globally, with increases witnessed principally in several countries in Eastern Europe and Central Asia. Based on data from 120 countries, 2.6 million new infections were estimated to have occurred in 2009.1,2
The epidemic in Latin America is characterized as stable and concentrated with an estimated population prevalence of 0.5% (95% CI: 0.4-0.6), while in the Caribbean prevalence varies widely from country to country with an overall estimate of 1.0% (95% CI: 0.9-1.1).2 Brazil is thought to be the most affected country, home to one third of all infected people in the region. Key populations at higher risk of HIV exposure and most affected by the epidemic include: men who have sex with men (MSM), reported prevalence between 7.9%-25.6%,3 female sex workers (FSW), 3.2%-4.3%4 and intravenous drug users (IDU), 0-78.0%.5
Data on the incidence and prevalence of HIV and other STI among MSM are very poor in most of the developing world.6 Even in countries where more information is available, the contribution of homosexual behavior to the HIV/AIDS epidemic is not fully appreciated, in part due to either a lack of data or lack of analysis of the available data.7 A number of more detailed epidemiological studies have shown that same sex behavior is more common and the HIV prevalence among MSM is higher than previously thought.8-10 In urban centers of Latin America, HIV prevalence has remained high among MSM, even as the epidemic has expanded to other populations.11
FSW have lower reported HIV prevalence than MSM but are still one of the key populations for HIV and STI transmission in Latin America and the Caribbean due to the large proportion of men who visit sex workers (2.5%-6.5%).12 Clients of FSW have sex with members of both high risk (FSW) and low risk (wives, regular partners) female populations.13 HIV/STI transmission networks are thus formed between populations at higher and those at lower risk, allowing for transmission of HIV and other STI between FSW and their partners, as well as transmission of STI among FSW. Given their central role in the epidemiology of HIV and other STI in Latin America, FSW must also be a major focus of HIV/STI surveillance and control efforts.
In response to differentiated epidemiological characteristics of the pandemic, UNAIDS recommends differentiated national strategic plans attuned to the situation in each country.14 A principal difficulty in creating such proposals, however, is the availability of accurate information on different sub-populations or widely varying estimates for the same country.15 Considering the mix of available information, we conducted a systematic review of the HIV prevalence among different key populations in Latin America and the Caribbean to gain a greater understanding of the epidemiologic profile in the region and help inform strategies in response to the HIV epidemic.
Materials and methods
This systematic review aims to synthesize articles, abstracts and reports of HIV prevalence studies conducted among key populations in Latin America and the Caribbean. From May to October, 2010, two independent investigators conducted searches of the PubMed and National Library of Medicine's meeting abstract databases for published articles and abstracts using the following key words: highrisk groups; female sex workers; men who have sex with men; homosexual men; HIV; prevalence; Latin America; and individual country names. Reference listings from previous reviews and papers were also used to identify original articles, conference proceedings and reports. "Gray literature," most often in the form of study reports, was included based on the knowledge of coauthors. We considered peerreviewed articles, abstracts and documents published up to September 2010.
Eligibility criteria
Publications were assessed based on target population, location, year, sampling methodology, sample size and language. Inclusion criteria for studies were determined a priori to be: studies including HIV prevalence data among MSM or FSW; publication in a peer-reviewed journal, country report or an abstract at a conference with peer-reviewed blinded abstract selection process; studies from the Latin American and Caribbean regions. Inclusion criteria for studies among FSW included ex-changing sex for money or goods in different periods (i.e.: last month, last six months and last year). Inclusion criteria for MSM included anal or oral sex with another man, recall periods varying (i.e.: last month, last six months and last year). Studies in English, Spanish and Portuguese published between 1986 and 2010 were included in the review.
Exclusion criteria were studies with 100 or fewer participants and studies that combined participants from the target populations with other populations such as clients of FSW. When multiple reports existed for a single study, one paper was chosen based on completeness of the information. Only original research articles and reports were taken into account for this study, ex-cluding those reported in a review for which we could not locate the abstract, original paper or report. Authors kept records of all excluded publications.
Classification and analysis of the published work
We created a master table in Microsoft Excel (Redmond, WA, USA), extracted key information from included surveys, and entered data into the table. We extracted 1) the first author; 2) the year of the study; 3) survey location; 4) sampling methodology; 5) study design; 6) inclusion criteria; 7) sample size; 8) HIV prevalence; and 9) respective confidence intervals. When unavailable in the selected publications, confidence intervals were calculated assuming a simple random sample: this included 48 studies among MSM and 38 studies among FSW.
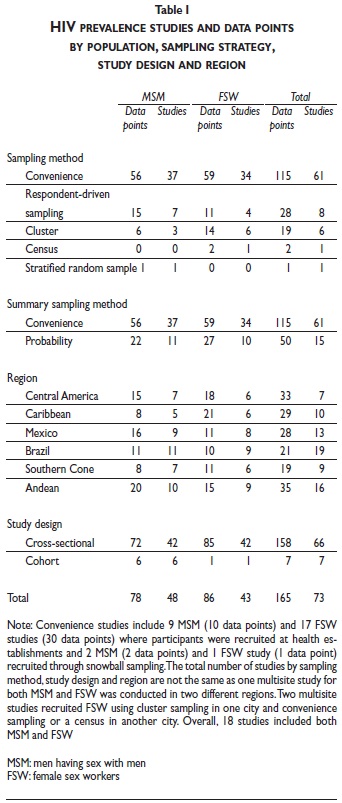
City estimates were reported as separate data points if the study presented the prevalence disaggregated by city. We originally arranged sampling methodologies into seven categories: unspecified convenience; snow-ball convenience; institutional convenience; cluster sampling including time-location sampling (TLS); stratified random sampling; census; and respondent-driven sampling (RDS). Institutional samples included those recruited at HIV testing, sexual/reproductive health, STI treatment and community centers. Institutional samples were presented as convenience samples in tables I, II and III. More recent data from 2000 to 2010 were summarized in a graph (figure 2).
Results
A total of 2 566 conference abstracts and 3 983 articles abstracts were originally identified. Of those, 2 539 conference proceedings and 3 876 articles were excluded because they were not from Latin America or the Caribbean, were out of scope or because they lacked an HIV prevalence estimate. One hundred and thirty-four records were deemed relevant by any reviewer and marked for full-text retrieval. Of those, 84 more were excluded due to duplicated data or sample size less than 100 (figure 1). Twenty- three studies considered gray literature were added to relevant peer-reviewed studies and conference papers for a total of 73 studies.
Men who have sex with men
Forty-eight studies screened 60 421 MSM (sample size range 102-7 041; median 306) and provided 78 population-and city- specific data points. Studies were published between 1988 and 2010. Data points were available from 19 countries. Most sites were large metropolitan centers. Studies were mostly cross-sectional, with the exception of six prospective cohort studies in four cities in South America and one Caribbean island. Recruitment venues included HIV testing clinics, medical and community-based organizations serving MSM, street locations, and social and workplace venues. The majority (77.1%) of studies was conducted using convenience sampling, and often a combination of techniques (advertising, active recruitment, HIV/STI testing centers, snowball, etc.) was used to reach the desired sample size. There were seven (14.6%) that used RDS, most of these in Central America, three (6.3%) cluster designs and one (2.1%) stratified random sample (table I). RDS studies were first reported in 2008. In countries where both RDS studies and convenience samples were conducted, there was a tendency for RDS studies to report lower HIV prevalence, though differences were not statistically significant based on confidence intervals.
Seventy-eight HIV prevalence points for MSM yielded a range of 0.5% in Paraguay (conducted in 2006)16 to 31.1% in Guadalajara, Mexico (1985-87),17 with a median of 10.6% (IQR: 7.4-17.4) (table II). Prevalence rates from 2000 to 2010 are presented in figure 2. Data points from the Caribbean, Central America, and Mexico showed less variability than the Andean region.
A few studies reported HIV incidence. In Brazil, three cohort studies were implemented in the cities of Rio de Janeiro, Sao Paulo and Belo Horizonte which found incidence rates of 3.1, 1.5 and 2.0 per 100 person years, respectively.18,19 In Peru, 1 140 men followed up between 1998 and 2000 yielded a seroincidence rate of 3.5 per 100 person years.20 The BED assay has also been used to estimate incidence in cross-sectional studies reporting a range of 2.1-14.4% (95%CI: 5.4-29.7) in Central America4 and 11.2% in Peru.21
Female sex workers
Forty-three prevalence studies surveyed 76 416 female sex workers (sample size range 101-24 500; median 265) and included 86 data points. Studies were published between 1986 and 2010 from 18 countries. Sites included capitals, ports and other tourist and commercial centers. The highest sample size, 24 500 was reached in Mexico (0.3% HIV prevalence), where women were recruited from HIV testing sites at health units across the country.22 Cross-sectional studies predominated with the exception of one prospective cohort study. Recruitment venues included HIV testing clinics, medical and community-based organizations serving FSW, street locations, and social and workplace venues. Most studies (77.3%) used convenience sampling with the exception of six (13.3%) cluster designs, four (8.9%) RDS and one (2.2%) census (not exclusive; some studies used different sampling methods in different cities).
RDS studies were first reported for FSW in 2009. Studies from Central America were more often conducted using RDS than those from other regions. FSW were sampled using probability methods more frequently than MSM, though the difference was small.
HIV prevalence ranged from 0% in parts of Honduras, Nicaragua, Panama, Uruguay, Chile, Bolivia, Peru and Venezuela (conducted between 1986 and 2006)*,23-30,121 to 12.4% in Haiti (1987-1988)31 with a median of 2.6% (IQR: 0.6-4.2) (table III). HIV prevalence among FSW by region and country from 2000-2010 are presented in figure 2. The data points showed lower prevalence and less variability than for MSM.
Discussion
Traditionally, the highest HIV prevalence among MSM have been reported in Mexico and the Andean countries. However, in the last 10 years the prevalence in Mexico appears to have decreased or studies have recruited a more heterogeneous sample and recent levels are similar to those reported in Central America. For FSW, the disease burden was greatest overall in Brazil, though recent rates were also lower than those from a decade ago. Taking into account the studies in this review, HIV prevalence among MSM was five times higher than among sex workers. HIV seroprevalence studies of other potentially key populations from Latin America and the Caribbean were lacking, and based on previous reviews men who have sex with men and female sex workers have proven to be the populations most affected by the HIV epidemic in countries across the region.3,32-36
One of most apparent characteristics regarding the prevalence among MSM, especially evident in the Andean region, was the high degree of variability among studies from different countries but also from the same country. This could be due to the different sampling methods used to recruit MSM. Few studies with probabilistic sampling methodologies had been carried out in the region. Furthermore, it is possible that researchers chose probability methods to sample female sex workers more often than for MSM on the assumption that the entire FSW population works from establishments that can be mapped and cluster sampled. In the U.S. venue based sampling has been used to conduct ongoing HIV behavioral surveillance among MSM,37 but in Latin America researchers have not opted for venue-based methods. In fact, the majority of articles were based on convenience methods, often combining snowball recruitment, out-reach referrals or advertisement methods. There are several possible explanations for this observation. MSM in Latin American countries might have been more difficult to recruit in venues compared to the U.S. due to lower social tolerance of sexual diversity and higher levels of stigma and discrimination. This could have resulted in insufficient number of MSM venues and safety concerns for field staff operating in dangerous areas. The high degree of convenience sampling and inclusion of larger proportions of MSM sub-populations at even higher risk such as male sex workers could have caused the large degree of variability on HIV prevalence among the MSM studies. Another explanation for the variability among studies is that RDS has been thought to produce lower seroprevalence estimates than other methods assuming that it reaches hidden segments of the target population, individuals who may have been sheltered from a lifestyle propitious to high rates of transmission.
More difficult to study are individuals who have sexual relations with key populations and with individuals at lower risk. In Latin America and the Caribbean, HIV has often been transmitted in this manner and data on infection rates in these populations were lacking. Mobile workers have exhibited high risk behavior via interactions with FSW: for example in 2003, in Santos, Brazil, 21.0% of 300 truck drivers reported paid sex in the last six months.38 Migrants, yet another key population, have been at higher risk of HIV exposure, a product of the conditions and structure of the migration process.39 Marginalized populations such as sex workers, injecting drug users and men who have sex with men traditionally have experienced internal and international migration and may become victims of exploitation, violence and exclusion.40,41 A high level of mobility, legal status, language and cultural differences; lack of information, education and work; poor access to prevention, harm reduction and health care services; and gender related factors have led to migrants' underprivileged status. Stigma has further exacerbated their vulnerability. These key populations should also be the focus of surveillance to better monitor the HIV epidemic. The objective of surveillance and most prevalence studies is to document the gravity of disease burden in the target population and to make recommendations regarding allocation of resources to control the spread of disease. A primary challenge for surveillance of these key populations is obtaining 'representative' samples.42,43 General population surveys with multi -stage cluster sampling are excessively expensive and cannot be used to reach hidden segments of the population.44
Several approaches have been proposed to balance the need for recruitment efficiency and inclusiveness in representation. Snowball sampling increases efficiency, identification, and inclusion of hidden populations by having members of the target population recruit other members.45 However, snowball sampling suffers from sampling bias and leads to a group that is not representative of the population. Facility-based sampling is also not generalizable as those who obtain services are different from those who do not. Targeted sampling involves an ethnographic mapping of the target population to later sample subgroups as strata. The magnitude of the bias in targeted sampling depends on the thoroughness of the ethnographic assessment. Time-location sampling involves an ethnographic mapping of sites where the target population meets or works and random selection of participants at randomly selected sites, days and times. Time-location sampling is a probability sampling method but as with targeted sampling, its representativeness depends on the exhaustiveness of the mapping and assistance of all population subgroups at selected sites. Nevertheless, TLS has worked well with more visible populations including female sex workers and their clients,46,47 and MSM in gay-identified areas of urban centers.48,49
Respondent-driven sampling has been used for surveillance of populations most at risk for HIV/AIDS in the United States and in more than 83 countries worldwide since 1994.50,51 In theory, weighted estimates generated from RDS generalize to the population as a whole. However, recent assessments of the RDS sampling methodology have documented limitations in the RDS assumptions.52,53 Despite these limitations, RDS is currently one of the only methods available to reach highly hidden populations that provides methodological rigor.
This review has several limitations. The use of different sampling methodologies diminished the validity of pooled prevalence estimates and only medians were presented as summary estimates in this paper. Calculated asymptotic confidence intervals were tighter than the true intervals, limiting the interpretability of the data. More recent studies may not have been included due to the lag time between data collection and publication of results. The inclusion of gray literature may also have been biased by the authors' geographical expertise or familiarity. Different types of laboratory tests were used to diagnosis HIV, including rapid tests, ELISA, and Western Blot among others. Information on the types of tests, specific tests or diagnostic algorithms was not always available for the included studies. This variability and lack of information limited the ability to compare the results from different studies. Medians and interquartile ranges (IQR) were reported and should be interpreted with care due to the different recruitment methodologies. For the same reason, trend analyses have not been presented in this article.
High prevalence rates among MSM and moderate rates among FSW have been detected in countries across Latin America and the Caribbean. A toolbox of standardized sampling techniques and data collection practices is urgently needed to clear up the varied picture presented by studies in this review. While many researchers continue to question the generalizability of RDS and TLS samples, it is encouraging that researchers are employing probability sampling methods more often than in the past. The implications of this study for prevention include recognizing that in Latin America and the Caribbean sufficient resources should be dedicated to HIV programs for men who have sex with men and sex workers to slow or stop transmission. Historical stigma attached to these key populations and their perceived or estimated population size in comparison to other populations influence decision makers. Widespread efforts are needed to ensure that leaders are aware of the results and that resources are allocated based on burden of disease and prevention needs.54 Periodic surveillance of MSM, FSW and other populations important to the HIV epidemic should continue.
References
1.UNAIDS, World Health Organization. AIDS epidemic update: December 2009. Geneva: UNAIDS, 2009. [ Links ]
2. Joint United Nations Programme on HIV/AIDS (UNAIDS). Global report: UNAIDS report on the global AIDS epidemic 2010. Geneva: UNAIDS; 2010. Report No. UNAIDS/10.11E | JC1958E. [ Links ]
3. Baral S, Sifakis F, Cleghorn F, Beyrer C. Elevated risk for HIV infection among men who have sex with men in low- and middle-income countries 2000-2006: A systematic review. PLoS Med 2007;4:e339. [ Links ]
4.Soto RJ, Ghee AE, Núñez CA, et al. Sentinel surveillance of sexually transmitted infections/HIV and risk behaviors in vulnerable populations in 5 Central American countries. J Acquir Immune Defic Syndr 2007;46:101-111. [ Links ]
5. Mathers BM, Degenhardt L, Phillips B, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet 2008;372:1733-175. [ Links ]
6. Joint United Nations Programme on HIV/AIDS (UNAIDS). Report on the global HIV/AIDS epidemic 2008. Geneva: UNAIDS; 2008 August. Report No. UNAIDS/08.25E / JC1510E. [ Links ]
7. Caceres C, Konda K, Pecheny M, Chatterjee A, Lyerla R. Estimating the number of men who have sex with men in low and middle income countries. Sex Transm Infect 2006;82 Suppl 3:iii3-9. [ Links ]
8.van Griensven F, Thanprasertsuk S, Jommaroeng R, et al. Evidence of
a previously undocumented epidemic of HIV infection among men who have sex with men in Bangkok, Thailand. Aids 2005;19:521-526.
9.Go VF, Solomon S, Srikrishnan AK, et al. HIV rates and risk behaviors are low in the general population of men in Southern India but high in alcohol venues: Results from 2 probability surveys. J Acquir Immune Defic Syndr 2007;46:491-497. [ Links ]
10.Go VF, Srikrishnan AK, Sivaram S, et al. High HIV prevalence and risk behaviors in men who have sex with men in Chennai, India. J Acquir Immune Defic Syndr 2004;35:314-319. [ Links ]
11.Cáceres CF, Pecheny M, Terto V. AIDS and Maleto-Male Sex in Latin America: Vulnerabilities, strengths and proposed measures - Perspectives and reflections from the point of view of public health, social sciences and activism. Lima, Peru: Universidad Cayetano de Heredia; 2002. Report No. UPCH/UNAIDS, 2002. [ Links ]
12.Carael M, Slaymaker E, Lyerla R, Sarkar S. Clients of sex workers in different regions of the world: hard to count. Sex Transm Infect 2006;82 Suppl 3:iii26-33. [ Links ]
13.Morris M, Podhisita C, Wawer MJ, Handcock MS. Bridge populations in the spread of HIV/AIDS in Thailand. AIDS 1996;10:1265-1271. [ Links ]
14.UNAIDS. Practical Guidelines for Intensifying HIV Prevention: Towards Universal Access. Geneva; 2007. Report No. UNAIDS/07.07E / JC1274E. [ Links ]
15.Caceres CF, Konda K, Segura ER, Lyerla R. Epidemiology of male same-sex behaviour and associated sexual health indicators in low- and middle-income countries: 2003-2007 estimates. Sex Transm Infect 2008;84 Suppl 1:i49-i56. [ Links ]
16.Chinaglia M, Tun W, Mello M, Insfran M, Díaz J. Assessment of Risk Factors for HIV Infection in Female Sex Workers and Men who have Sex with Men in Ciudad del Este, Paraguay. Horizons Final Report. Washington, DC: Population Council, 2008. [ Links ]
17. Vázquez-Valls E, Torres-Mendoza B, Soto-Sánchez E, Delgadillo-Madrueño F. Prevalence of Anitbody to HIV in a Group of Homosexual Men in Guadalajara, Mexico. In: Program and abstracts of the IV International Conference on AIDS; 1988; Stockholm; 1988. [ Links ]
18.Harrison LH, do Lago RF, Friedman RK, et al. Incident HIV infection in a highrisk, homosexual, male cohort in Rio de Janeiro, Brazil. J Acquir Immune Defic Syndr 1999;21:408-412. [ Links ]
19.Ramos A, Tanuri A, Schechter M, et al. Dual and recombinant infections: an integral part of the HIV-1 epidemic in Brazil. Emerg Infect Dis 1999;5:65-74. [ Links ]
20.Sanchez J, Lama JR, Peinado J, et al. High HIV and ulcerative sexually transmitted infection incidence estimates among men who have sex with men in Peru: awaiting for an effective preventive intervention. J Acquir Immune Defic Syndr 2009;51 Suppl 1:S47-51. [ Links ]
21. Tabet S, Sanchez J, Lama J, et al. HIV, syphilis and heterosexual bridging among Peruvian men who have sex with men. AIDS 2002;16:1271-1277. [ Links ]
22.Magis-Rodriguez C, Loo-Mendez E, Santarriaga-Sandoval M. [HIV/ AIDS Epidemiologic Surveillance through Sentinel Surveys 1991-1996, CONASIDA]. AIDS-STI Program 1997;3:60-62. [ Links ]
23.Reeves WC, Cuevas M, Arosemena JR, et al. Human immunodeficiency virus infection in the Republic of Panama. Am J Trop Med Hyg 1988;39:398-405. [ Links ]
24.Camejo MI, Mata G, Diaz M. [Prevalence of hepatitis B, hepatitis C and syphilis in female sex workers in Venezuela]. Rev Saude Publica 2003;37:339-344. [ Links ]
25. Zegarra L, Flores J, Bachelet M, et al. Prevalence of HIV among different risk groups in Cochabamba, Bolivia. In: International Conference on AIDS. Meeting held in Switzerland: Escuela Tecnica de Salud Cochabamba Chile; 1998:118 (abstract no. 13166). [ Links ]
26. Padilla IS, Soto RJ. [Central American Multicentre HIV/STI Prevalence and Behavioral Study in Female Sex Workers in Nicaragua]. Final Report. Managua: Nicaraguan Ministry of Health, 2003. [ Links ]
27. Golenbock DT, Guerra J, Pfister J, et al. Absence of infection with human immunodeficiency virus in Peruvian prostitutes. AIDS Res Hum Retroviruses 1988;4:493-499. [ Links ]
28. Trujillo L, Munoz D, Gotuzzo E, Yi A, Watts DM. Sexual practices and prevalence of HIV, HTLV-I/II, and Treponema pallidum among clandestine female sex workers in Lima, Peru. Sex Transm Dis 1999;26:115-118. [ Links ]
29. Castro de Batanjer E. Un abordaje epidemiológico de la infección por VIH-1/2 entre trabajadoras sexuales y hombres homosexuales de la Isla de Margarita, Venezuela. Rev Soc Bras Med Trop 1997;30:255-256. [ Links ]
30. Montano SM, Sanchez JL, Laguna-Torres A, et al. Prevalences, genotypes, and risk factors for HIV transmission in South America. J Acquir Immune Defic Syndr 2005;40:57-64. [ Links ]
31. Paredes M, Soto R. [Central American Multicentre HIV/STI Prevalence and Behavioral Study in Female Sex Workers in Honduras]. Tegucigalpa: Honduran Ministry of Health, 2003. [ Links ]
32. Bastos FI, Caceres C, Galvao J, Veras MA, Castilho EA. AIDS in Latin America: assessing the current status of the epidemic and the ongoing response. Int J Epidemiol 2008;37:729-737. [ Links ]
33. Caceres CF. HIV among gay and other men who have sex with men in Latin America and the Caribbean: a hidden epidemic? AIDS 2002;16 Suppl 3:S23-33. [ Links ]
34. Calleja JM, Walker N, Cuchi P, Lazzari S, Ghys PD, Zacarias F.
Status of the HIV/AIDS epidemic and methods to monitor it in the Latin America and Caribbean region. AIDS 2002;16 Suppl 3:S3-12.
35. Malta M, Magnanini MM, Mello MB, Pascom AR, Linhares Y, Bastos FI. HIV prevalence among female sex workers, drug users and men who have sex with men in Brazil: A systematic review and meta-analysis. BMC Public Health 2010;10:317. [ Links ]
36. Estebanez P, Fitch K, Najera R. HIV and female sex workers. Bull World Health Organ 1993;71:397-412. [ Links ]
37. MacKellar D, Valleroy L, Karon J, Lemp G, Janssen R. The Young Men's Survey: methods for estimating HIV seroprevalence and risk factors among young men who have sex with men. Public Health Rep 1996;111 Suppl 1:138-144. [ Links ]
38. Lacerda R, Gravato N, McFarland W, et al. Truck drivers in Brazil: prevalence of HIV and other sexually transmitted diseases, risk behavior and potential for spread of infection. AIDS 1997;11 Suppl 1:S15-S19. [ Links ]
39. Garcia-Calleja JM, Rio CD, Souteyrand Y. HIV infection in the Americas: improving strategic information to improve response. J Acquir Immune Defic Syndr 2009;51 Suppl 1:S1-3. [ Links ]
40. Bronfman M. Mexico and Central America. Int Migr 1998;36:609-642. [ Links ]
41. Frye V, Latka MH, Koblin B, et al. The urban environment and sexual risk behavior among men who have sex with men. J Urban Health 2006;83:308-24. [ Links ]
42. Mills S, Saidel T, Bennett A, et al. HIV risk behavioral surveillance: a methodology for monitoring behavioral trends. AIDS 1998;12 Suppl 2:S37-46. [ Links ]
43. Schwartlander B, Ghys PD, Pisani E, et al. HIV surveillance in hard-to-reach populations. AIDS 2001;15 Suppl 3:S1-3. [ Links ]
44. Magnani R, Sabin K, Saidel T, Heckathorn D. Review of sampling hard-to-reach and hidden populations for HIV surveillance. AIDS 2005;19 Suppl 2:S67-72. [ Links ]
45. Erickson B. Some problems of inference from chain data. Sociological Methodology Research 1971;10:276-302. [ Links ]
46. Kayembe PK, Mapatano MA, Busangu AF, et al. Determinants of consistent condom use among female commercial sex workers in the Democratic Republic of Congo: Implications for interventions. Sex Transm Infect 2008;84:202-206. [ Links ]
47.Nguyen NT, Nguyen HT, Trinh HQ, Mills SJ, Detels R. Clients of female sex workers as a bridging population in Vietnam. AIDS Behav 2009;13:881-891. [ Links ]
48. Muhib FB, Lin LS, Stueve A, et al. A venue-based method for sampling hard-to-reach populations. Public Health Rep 2001;116 Suppl 1:216-222. [ Links ]
49.Stueve A, O'Donnell LN, Duran R, San Doval A, Blome J. Time-space sampling in minority communities: Results with young Latino men who have sex with men. Am J Public Health 2001;91:922-926. [ Links ]
50.Johnston LG, Khanam R, Reza M, et al. The effectiveness of respondent driven sampling for recruiting males who have sex with males in Dhaka, Bangladesh. AIDS Behav 2008;12:294-304. [ Links ]
51.Broadhead RS, Heckathorn DD, Grund J-PC, Stern LS, Anthony DL. Drug users versus outreach workers in combating aids: preliminary results of a peer- driven intervention. J Drug Issues 1995;25:531-564. [ Links ]
52.Goel S, Salganik MJ. Assessing respondent-driven sampling. Proc Natl Acad Sci USA 2010;107:6743-6747. [ Links ]
53.Gile K, Handcock M. Respondent-driven sampling: An assessment of current methodology. Sociol Methodol 2010;40,1:285-327. [ Links ]
54.Pan American Health Organization. Challenges Posed by the HIV Epidemic in Latin America and the Caribbean 2009. Lima, Peru: PAHO, UNICEF and UNAIDS, 2009. [ Links ]
55. World Vision of Guatemala. [Final report of the baseline study: Initiative for the strengthening of HIV/AIDS prevention and treatment actions among vulnerable groups and prioritized areas]. Final report. Guatemala: World Vision of Guatemala, 2007. [ Links ]
56.Sánchez-Viesca AF. Final report of the follow-up study: Initiative for the strengthening of HIV/AIDS prevention and treatment actions among vulnerable groups and prioritized areas. Final report. Guatemala City: World Vision of Guatemala; Center for Strategic Health Development (CES), 2010. [ Links ]
57.Guardado ME, Creswell J, Paz-Bailey G. [Central American Survey of Sexual Behavior and HIV/STI Prevalence among Vulnerable Populations (ECVC): El Salvador]. Final Report. San Salvador: Ministry of Health (MS-PAS), National STI/HIV/AIDS Program; del Valle University of Guatemala and Centers for Disease Control and Prevention (CDC) Collaboration, Global AIDS Program Regional Office for Central America and Panama (CDC-GAP/CAP), 2010. [ Links ]
58.Padilla IS, Soto RJ. [Central American Multi-centre HIV/STI Prevalence and Behavioral Study in Men Who Have Sex with Men in Honduras]. Final Report. Tegucigalpa: Honduran Ministry of Health, 2003. [ Links ]
59.Morales-Miranda S, Paz-Bailey G, Arambu N, Álvarez B, Paredes M, Monterroso E. [Central American Survey of Sexual Behavior and HIV/ STI Prevalence among Vulnerable Populations in Honduras (ECVC): Men Who Have Sex with Men. Final report. Tegucigalpa: Del Valle University of Guatemala, Honduran Ministry of Health, CDC, USAID, Tephinet, Inc, 2008. [ Links ]
60.Solano T. [Prevalence of HIV, Syphilis and Risky Behavior among MSM in the Greater Metropolitan Area of Costa Rica]. Final report. San José: Costa Rican Ministry of Health, 2010. [ Links ]
61.Galban E, Menendez J, Gil R, Terry H. CUBA: Study of sexual contacts of the HIV seropositive persons. In: International Conference on AIDS; 1989 Jun 4-9; Montreal; 1989. [ Links ]
62.Toro-Alfonso JN. V-D. Proyecto Delta. Informe Final. Santo Domingo. Dominican Republic: CESDEM, 2005. [ Links ]
63. Tabet SR, de Moya EA, Holmes KK, et al. Sexual behaviors and risk factors for HIV infection among men who have sex with men in the Dominican Republic. AIDS 1996;10:201-206. [ Links ]
64. Rojas-Lara G, Caballero-Vaillant T, Mercedes-Valles H, et al. [1st Behavioral Survey with Serological Data among Vulnerable Populations: Gay, Trans and Other Men Who Have Sex with Men; Sex Workers; Drug Users. Santo Domingo, Dominican Republic: Presidencial AIDS [ Links ]
65.Murphy EL, Gibbs WN, Figueroa JP, et al. Human immunodeficiency virus and human T-lymphotropic virus type I infection among homosexual men in Kingston, Jamaica. J Acquir Immune Defic Syndr 1988;1:143-149. [ Links ]
66.Izazola-Licea JA, Valdespino-Gomez JL, Gortmaker SL, et al. HIV-1 seropositivity and behavioral and sociological risks among homosexual and bisexual men in six Mexican cities. J Acquir Immune Defic Syndr 1991;4:614-622. [ Links ]
67. Preciado-Negrete P, Campos-Lopez P, Torres-Mendoza B, Alvarez-Maya I, Vazquez-Valls E. Tendency of anti-HIV antibodies in homosexual men during the last seven years in Guadalajara, Mexico. In: International Conference on AIDS; 1991 June 16-21; Florence; 1991:300. [ Links ]
68.Magis-Rodriguez C, Gayet C, Manrique B. [Report on the results from the prevalence and behavioral surveillance survey on HIV/AIDS in: Men who have sex with men, female sex workers, male sex workers and injection drug users]. Technical report. Mexico, DF: National HIV/AIDS Program (CENSIDA), 2005. [ Links ]
69.Guerena-Burgueno F, Benenson AS, Sepulveda-Amor J. HIV-1 prevalence in selected Tijuana sub-populations. Am J Public Health 1991;81:623-635. [ Links ]
70.Hernandez M, Uribe P, Gortmaker S, et al. Sexual behavior and status for human immunodeficiency virus type 1 among homosexual and bisexual males in Mexico City. Am J Epidemiol 1992;135:883-894. [ Links ]
71. Teran-Toledo X, Hernandez T, del Rio C, Uribe Z. Risk factors for HIV infection in Mexico City. In: International Conference on AIDS; 1996; Vancouver; 1996:40. [ Links ]
72.Gayet C, Magis C, Sacknoff D, Guli L. [Sexual Practices of Populations Vulnerable to the HIV/AIDS Epidemic in Mexico]. Mexico, DF: National Center for HIV/AIDS Prevention and Control (CENSIDA); Latin American School of Social Sciences (FLACSO), 2007. [ Links ]
73. Ribeiro TT, Brites C, Moreira ED, Jr., et al. Serologic validation of HIV infection in a tropical area. J Acquir Immune Defic Syndr 1993;6:319-322. [ Links ]
74.Barcellos NT, Fuchs SC, Fuchs FD. Prevalence of and risk factors for HIV infection in individuals testing for HIV at counseling centers in Brazil. Sex Transm Dis 2003;30:166-173. [ Links ]
75.Carvalheiro J, Spink M, Figueiredo G, et al. Cohort Bela Vista: feasibility of efficacy trials on HIV vaccines. In: International Conference on AIDS 1998; 1998:954-955. [ Links ]
76. Viana L, Toledo A, Antunes C, Greco D. Laboratory status of homo/ bisexual men from a cohort study in Belo Horizonte, Brazil. In: International Conference on AIDS. Vancouver, BC; 1996:301. [ Links ]
77.Carneiro M, Cardoso FA, Greco M, et al. Determinants of human immunodeficiency virus (HIV) prevalence in homosexual and bisexual men screened for admission to a cohort study of HIV negatives in Belo Horizonte, Brazil: Project Horizonte. Mem Inst Oswaldo Cruz 2003;98:325-329. [ Links ]
78.Szwarcwald CL, de Carvalho MF, Barbosa-Junior A, Barreira D, Speranza FA, de Castilho EA. Temporal trends of HIV-related risk behavior among Brazilian military conscripts, 1997-2002. Clinics (Sao Paulo) 2005;60:367-374. [ Links ]
79.Mello M, Pinho AA, Chinaglia M, et al. Assessment of Risk Factors for HIV Infection Among Men Who Have Sex With Men in the Metropolitan Area Of Campinas City, Brazil, Using Respondent-Driven Sampling. Hori-zons Final Report. Washington, DC: Population Council, 2008. [ Links ]
80. Cortes E, Detels R, Aboulafia D, et al. HIV-1, HIV-2, and HTLV-I infection in high-risk groups in Brazil. N Engl J Med 1989;320:953-958. [ Links ]
81. Sutmoller F, Penna TL, de Souza CT, Lambert J. Human immunode-ficiency virus incidence and risk behavior in the 'Projeto Rio': results of the first 5 years of the Rio de Janeiro open cohort of homosexual and bisexual men, 1994-98. Int J Infect Dis 2002;6:259-265. [ Links ]
82. Perisse AR, Schechter M, Moreira RI, do Lago RF, Santoro-Lopes G, Harrison LH. Willingness to participate in HIV vaccine trials among men who have sex with men in Rio de Janeiro, Brazil. Projeto Praca Onze Study Group. J Acquir Immune Defic Syndr 2000;25:459-463. [ Links ]
83. Raxach J, Terto-Jr V, Garcia J, Pimenta C, Almeida V, Parker R. [Sexual practices and AIDS awareness: A study about homo and bisexual men]. Rio de Janeiro: ABIA, 2007. [ Links ]
84.Cabello A, Cabral M, Vera E, Arrom C, Kiefer R, Zoulek G. The risk of sexually-acquired HIV infection in Paraguay. In: International Conference on AIDS; 1991 Jun 16-21; Florence; 1991:354. [ Links ]
85.Berriolo R. PAHO/WHO HIV surveillance report. Montevideo: Uruguayan Ministry of Health, National STI/AIDS Program; PAHO/WHO; 1998 March 3. [ Links ]
86.Muchinik G, Fay O, Cahn P, et al. HIV Seropositivity in High-Risk Groups in Argentina: Future Impact on Heterosexual Transmission. In: IV International Conference on AIDS; 1988; Stockholm; 1988. [ Links ]
87.Cahn P, Perez H, Casiro A, et al. HIV-Infection in Risk Groups In Buenos Aires. Prevalence and Predictive Factors. In: IV International Conference on AIDS; 1988; Stockholm; 1988. [ Links ]
88. Segura M, Sosa-Estani S, Marone R, et al. Buenos Aires cohort of men who have sex with men: prevalence, incidence, risk factors, and molecular genotyping of HIV type 1. AIDS Res Hum Retroviruses 2007;23:1322-1329. [ Links ]
89.Ribero V, Paz-Bailey G, Protto JP. [Study of HIV and Masculinity in Bolivia]. La Paz: Bolivian Ministry of Health, 2010. [ Links ]
90. Agüero G, Wignall FS, Alexander W, et al. HIV Infections in Peru. In: IV International Conference on AIDS; 1988; Stockholm; 1988. [ Links ]
91.McCarthy MC, Wignall FS, Sanchez J, et al. The epidemiology of HIV-1 infection in Peru, 1986-1990. AIDS 1996;10:1141-1145. [ Links ]
92.Caceres C, Gotuzzo E, Wignall S, Campos M. Sexual behavior and frequency of antibodies to type 1 human immunodeficiency virus (HIV-1) in a group of Peruvian male homosexuals. Bull Pan Am Health Organ 1991;25:306-319. [ Links ]
93.Sanchez J, Lama JR, Kusunoki L, et al. HIV-1, sexually transmitted infections, and sexual behavior trends among men who have sex with men in Lima, Peru. J Acquir Immune Defic Syndr 2007;44:578-585. [ Links ]
94. Caceres CF, Konda KA, Salazar X, et al. New populations at high risk of HIV/STIs in low-income, urban coastal Peru. AIDS Behav 2008;12:544-551. [ Links ]
95. Merino N, Sanchez RL, Munoz A, Prada G, Garcia CF, Polk BF. HIV-1, sexual practices, and contact with foreigners in homosexual men in Colombia, South America. J Acquir Immune Defic Syndr 1990;3:330-334. [ Links ]
96.Echeverria de Perez G, Loreto O, Bianco NE, Mendez-Castellanos H, Burczak JD, Lee H. Reappraisal of human retroviral infection in Venezuela. AIDS Res Hum Retroviruses 1992;8:219-220. [ Links ]
97. Pinzón Z, Soto-Hernandez RJ, Aguilar S. [Central American Multi-centre HIV/STI Prevalence and Behavioral Study: Female Sex Workers in Guatemala]. Final report. Guatemala: Ministry of Health; Asociación de Salud Integral (ASI), 2003. [ Links ]
98.Palma-López L, Soto-Hernández RJ. [Central American Multi-centre HIV/STI Prevalence and Behavioral Study: Female Sex Workers in El Salvador]. Final report. San Salvador: Ministry of Health, 2003. [ Links ]
99. Contreras-Arrocha S, Soto RJ. [Central American Multi-centre HIV/ STI Prevalence and Behavioral Study in Female Sex Workers in Panama]. Final Report. Panama City: Panamanian Ministry of Health, 2003. [ Links ]
100.Rosario S, Guerrero E, De Moya E, Volquez C, Alcantara R. The ag-glutinating approach to joint STD/AIDS prevention and control in female sex workers in the Dominican Republic. In: International Conference on AIDS; 1989 Jun 4-9; Vancouver; 1989:708 (abstract no. Th.D.O.10) [ Links ]
101. Gomez E. [HIV Seroprevalence Surveys Based on Sentinel Sites: Results from 2004 surveys]. Final report: Dominican Ministry of Health, 2005. [ Links ]
102.Dominican Ministry of Health. [HIV Seroprevalence Surveys Based on Sentinel Sites: Results from Surveys 2005-2006]. Santo Domingo: Dominican Ministry of Health, 2006. [ Links ]
103.Dominican Ministry of Health. [Results from the "XV Second Generation Serological Sentinel Surveillance Survey" 2006]. Final report. Santo Domingo: Dominican Ministry of Health (SESPAS), 2007. [ Links ]
104. Elie R, Chout R, Lassegue A, Dorlette J, Cesar D, Delaunay B. Antibodies to HIV-1 and HTLV-1 in Haiti. In: International Conference on AIDS. Meeting held in Canada: Laboratoire d'Investigations Biologiques Port-au-Prince Haiti; 1989 77 (abstract no. Th.A.O.30). [ Links ]
105. Torres-Mendoza BM, Vazquez-Valls E, Ayala-Chavira M, Ayala y de Landeros G. Prevalence of antibodies to Human Immunodeficiency Virus (HIV) in prostitutes in Guadalajara, Mexico. In: IV International Conference on AIDS. Stockholm; 1988. [ Links ]
106. Uribe P, Hernandez AM, Ornelas HG, Jesus MR, Chavez PF, Sepulve-da AJ. Analysis of factors related with HIV infection in 961 female sexual workers. In: International Conference on AIDS. Meeting held in United States: AIDS Information Center. CONASIDA. Mexico City. Mexico; 1990 320 (abstract no. Th.D.777). [ Links ]
107. Loo-Mendez E, Hernandes-Tepichini G, Teran-Toledo X. SIT/HIV/ AIDS in male and female sex workers in a center of integral attention in Mexico. In: International Conference on AIDS. Meeting held in South Africa: National AIDS Council CONASIDA; 2000 abstract no. ThPeC5456. [ Links ]
108. Uribe-Salas F, Conde-Glez CJ, Juarez-Figueroa L, Hernandez-Castel-lanos A. Sociodemographic dynamics and sexually transmitted infections in female sex workers at the Mexican-Guatemalan border. Sex Transm Dis 2003;30:266-271. [ Links ]
109. Lurie P, Fernandes ME, Hughes V, et al. Socioeconomic status and risk of HIV-1, syphilis and hepatitis B infection among sex workers in Sao Paulo State, Brazil. Instituto Adolfo Lutz Study Group. AIDS 1995;9 Suppl 1:S31-7. [ Links ]
110. Pires ICP, Miranda AEB. Prevalence and Correlates of HIV Infection and Syphilis in Prostitutes Attending a STD/AIDS Reference Center. Rev Bras Ginecol Obstet 1998;20:151-154. [ Links ]
111.Broutet N, de Queiroz Sousa A, Basilio FP, Sa HL, Simon F, Dabis F. Prevalence of HIV-1, HIV-2 and HTLV antibody, in Fortaleza, Ceara, Brazil, 1993-1994. Int J STD AIDS 1996;7:365-369. [ Links ]
112. Guimaraes K, Godoi A, Mercán-Hamann E, Andrade J. [Evaluation of the effectiveness of prevention activities oriented towards female sex workers in three regions of Brazil]. Brasilia: Brazilian Ministry of Health, Secretary of Health Surveillance, National STI and AIDS Program 2004. [ Links ]
113.Granato C, Johnson W, Brites C, Bianco C, Gerbi L, Zamariol L. Retrovirus infection in prostitutes in Brazil. In: International Conference on AIDS. Meeting held in United States: Inst. Adolfo Lutz-Sao Paulo Brazil; 1990 226 (abstract no. F.C.581). [ Links ]
114.Szwarcwald CL, Bastos FI, Gravato N, Lacerda R, Chequer PN, de Castilho EA. The relationship of illicit drug use to HIV-infection among commercial sex workers in the city of Santos, São Paulo, Brazil. Int J drug policy 1998;9:427-436. [ Links ]
115.Gonzalez de Morell MG, da Silva NG, Lacerda RM, Araujo N. Respondent driven sampling: An effective methodology to estimate vulnerability to HIV transmission in sex workers of Santos, Brazil. In: International Union for the Scientific Study of Population (IUSSP) International Population Conference; 2009 27 Sept- 2 Oct; Morroco; 2009. [ Links ]
116.Benzaken AS, Sabido M, Galban EG, et al. Field evaluation of the performance and testing costs of a rapid point-of-care test for syphilis in a red-light district of Manaus, Brazil. Sex Transm Infect 2008;84:297-302. [ Links ]
117.Berriolo R, Colistro L, Rostkier J, Rivas B, Zessler L. HIV seroprevalence surveys in Uruguay. AIDS 1992;6:884-885. [ Links ]
118.Zapiola I, Salomone S, Alvarez A, et al. HIV-1, HIV-2, HTLV-I/II and STD among female prostitutes in Buenos Aires, Argentina. Eur J Epidemiol 1996;12:27-31. [ Links ]
119. Barrientos JE, Bozon M, Ortiz E, Arredondo A. HIV prevalence, AIDS knowledge, and condom use among female sex workers in Santiago, Chile. Cad Saude Publica 2007;23:1777-1784. [ Links ]
120. Lambert ML, Torrico F, Billot C, Mazina D, Marleen B, Van der Stuyft P. Street youths are the only high-risk group for HIV in a low-prevalence South American country. Sex Transm Dis 2005;32:240-242. [ Links ]
121.Johnston LG, Paz-Bailey G, Morales-Miranda S, et al. High prevalence of Mycoplasm genitalium among female sex workers in Honduras: implications for the spread of HIV and other sexually transmitted infections. Int J STD AIDS 2012;23:5-11. [ Links ]
 Corresponding author:
Corresponding author:
William Miller. 6 Jordan Dr., Pittsboro, NC 27312 USA
E-mail: meihackmiller@gmail.com
Received on: February 11, 2011
Accepted on: July 10, 2012