Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Salud Pública de México
versão impressa ISSN 0036-3634
Salud pública Méx vol.54 no.1 Cuernavaca Jan./Fev. 2012
ORIGINAL ARTICLE
Optimal cutoff points for the detection of undiagnosed type 2 diabetes, hypertension and metabolic syndrome in Mexican adults
Puntos de corte óptimos para la detección de diabetes tipo 2, hipertensión y síndrome metabólico no diagnosticados en adultos mexicanos
Rosalba Rojas-Martínez, MC PhDI; Carlos A Aguilar-Salinas, M EspII; Aída Jiménez-Corona, MC, PhDI
IInstituto Nacional de Salud Pública. Cuernavaca, Morelos, México
IIInstituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán. México, DF, México
ABSTRACT
OBJECTIVE: To compare the waist circumference cutoff points established by the American Heart Association and the National Heart, Lung and Blood Institute (AHA/NHLBI) with those of the International Diabetes Federation (IDF) for the screening of diabetes, hypertension, and metabolic syndrome in Mexican adults.
MATERIAL AND METHODS: This study comprised a subsample of the ENSANUT 2006. Subjects without diabetes and hypertension and non-pregnant women were included. Sensitivity, specificity, and predictive values were compared using AUC and the positive likelihood ratio test [LR(+)].
RESULTS: In subjects aged ≥40 years, sensitivity for detection of diabetes and hypertension was higher for the IDF thresholds (85.34 and 86.87%, respectively) compared with those of the AHA/NHLBI (59.49 and 52.41%, respectively). LR(+) were higher for IDF thresholds compared with AHA/NHLBI. Similar results in subjects aged ≥65 years were observed.
CONCLUSIONS: The measurement of abdominal obesity defined by the IDF was a better screening tool for diabetes and hypertension, considering that initially a high sensitivity and low cost tool at population level is required.
Key words: waist circumference; diabetes; hypertension; metabolic syndrome; Mexico
RESUMEN
OBJETIVO: Comparar los puntos de corte de circunferencia de cintura de la American Heart Association and the National Heart, Lung and Blood Institute (AHA/NHLBI) y la International Diabetes Federation (IDF) para escrutinio de diabetes, hipertensión arterial y síndrome metabólico en adultos mexicanos.
MATERIAL Y MÉTODOS: Se analizó una submuestra de la ENSANUT 2006 incluyendo sujetos sin diabetes o hipertensión y mujeres no embarazadas. Se comparó la sensibilidad, especificidad y valores predictivos mediante AUC y la razón de verosimilitudes positiva [LR(+)].
RESULTADOS: En personas ≥40 años, la sensibilidad para detección de diabetes e hipertensión usando el criterio de la IDF fue de 85.34% (LR(+)=1.1) y 86.87% (LR(+)=1.1); mientras que para el criterio de la AHA/NHLBI fue de 59.49% (LR(+)=1.34) y 52.41% (LR(+)=1.21). Los resultados fueron similares en personas ≥65 años.
CONCLUSIONES: La obesidad abdominal según la IDF fue superior como procedimiento de tamizaje de diabetes e hipertensión, considerando que se requiere de una prueba inicial más sensible y de bajo costo para ser aplicada a nivel poblacional.
Palabras clave: circunferencia de cintura; diabetes; hipertensión; síndrome metabólico; México
Obesity stands as an important risk factor for the development of chronic diseases such as type 2 diabetes1,2 and cardiovascular diseases.3 Central or abdominal obesity as measured by waist circumference has been proven to predict diabetes4,5 and cardiovascular risk.6-8 The etiology of obesity is rather complex; this disease results from a combination of genetic9 and environmental10 factors. The process of urbanization and modernization plays a key role, particularly in indigenous populations. In Mexico, prevalence, morbidity, and associated risk factors for obesity have been studied for several decades, as well as the outcomes of prevention and treatment programs.11-15 The prevalence of obesity in Mexican adults has shown a remarkable increase over time. Data from the 1993 National Survey of Chronic Diseases (ENEC 1993) revealed an obesity prevalence of 21.5% in adults,16 which rose to 24%17 according to the 2000 National Health Survey (ENSA 2000), and further to 30% in adults from the 2006 National Health and Nutrition Survey (ENSANUT 2006).18 In that survey, the prevalence of central obesity, using the cutoff points suggested by the American Heart Association and the National Heart, Lung and Blood Institute (AHA/NHLBI) (≥102 cm in men and ≥88 cm in women)19 and by the International Diabetes Federation (IDF) (≥90 cm in men and ≥80 cm in women)20 was 22.8% and 62.9% in men and 61.4% and 83.8% in women, respectively.21
Several researchers have recommended the use of body mass index and waist circumference measurements as screening tools for the detection of chronic non-transmissible diseases.5,7,8 Their diagnostic power must be evaluated in a representative sample of a study population, such as that of the ENSANUT 2006, because predictive values of a screening tool depend on the prevalence of a given disease. The aim of this paper was to describe the diagnostic properties of waist circumference as a screening tool for defining abdominal obesity using different cutoff points of waist circumference for the detection of diabetes, hypertension, and metabolic syndrome. Cases with physician-diagnosed diabetes or hypertension were excluded; hence we were able to estimate the proportion of population at risk for the above mentioned diseases and to quantify the number of cases that needed to modify their lifestyles or to receive pharmacological treatment. The Research, Ethics, and Biosecurity Boards of the National Institute of Public Health (INSP) approved the methodology of the ENSANUT 2006. All participants signed an informed consent letter.
Material and Methods
The ENSANUT 2006 gathered information about health and nutritional status of Mexican population, including the prevalence of some chronic and infectious diseases as well as the people's perceptions of the quality and response of health care services. A probabilistic, multistage, stratified, and clustered sample design was employed for the survey. The sample was representative of the population from the 32 states of the country and permitted to make the calculation of state indicators representative of urban and rural areas for each state. Localities with less than 2 500 inhabitants were regarded as rural. A total of 47 152 households were visited and information from 45 446 adults aged 20 years or older was obtained. Individuals were asked about previous physician diagnosis of diabetes, hypertension, and cardiovascular disease, among other chronic diseases. Anthropometric (weight, height, and waist circumference) and blood pressure measurements were taken. Thirty percent of randomly chosen individuals gave a fasting blood sample. In order to estimate the prevalence of diabetes in Mexico, a subsample of 6 613 individuals were also randomly selected and the levels of glucose, insulin, triglycerides, total cholesterol, HDL-cholesterol and LDL-cholesterol in their blood were determined in a standardized laboratory. After excluding people with prior physician diagnosis of diabetes and hypertension and pregnant women, we had a total of 4 687 individuals for our analysis.
Diabetes was defined as fasting venous glucose levels (8 to 12 hours) ≥126 mg/dL. Hypertension was defined as systolic blood pressure (SBP) ≥140 mm Hg or diastolic blood pressure (DBP) ≥90 mm Hg (average of two readings taken 5 minutes apart). Overweight was defined as BMI between 25 kg/m2 and 29.9 kg/m2 and obesity, as BMI ≥30 kg/m2. According to the AHA/NHLBI, abdominal obesity was defined as waist circumference ≥102 cm in men and ≥88 cm in women, and according to the IDF, as waist circumference >90 cm in men and >80 cm in women. Hypercholesterolemia was defined as total cholesterol concentrations ≥200 mg/dl and high LDL as concentrations ≥150 mg/dl. According to the AHA/NHLBI, metabolic syndrome was defined as the presence of at least three of the following components: waist circumference ≥102 cm in men and ≥88 cm in women, triglycerides ≥150 mg/dl, HDL-cholesterol <40 mg/dl in men and <50 mg/dl in women, SBP ≥135 or DBP ≥85 mm Hg or physician's diagnosis of hypertension, and fasting glucose ≥100 mg/dl or physician's diagnosis of diabetes.
Statistical analysis
Means and prevalence with their respective standard errors were obtained when appropriate. In stratified analysis by age ≥40 and <40 years, sensitivity, specificity, and positive and negative predictive values were estimated and compared by analysis of receiver operating characteristics (ROC) and examination of the areas under the ROC curves (AUC) using the DeLong method.22 Also positive and negative likelihood ratios (LR) were obtained. In addition, an analysis in individuals aged ≥65 year was carried out. Crude and age and sex-adjusted logistic regression were carried out to determine the association between diabetes, hypertension and metabolic syndrome and cut-off points of waist circumference of interest. Odds ratio (OR) and its corresponding 95% confidence interval (95%CI) were obtained as a measure of the association. Analyses were conducted using SAS 9.2 taking into account the sample complex design.
Results
The study population was composed of 4 687 individuals (1 901 men and 2 786 women). After weighting, the sample represented about 40-million Mexican adults. The mean of age was 37.9 years in women and 38.4 years in men. The average waist circumference was 90.7 in women and 92.6 in men. The prevalence of undiagnosed diabetes, hypertension, and metabolic syndrome was 5.2, 14.3, and 27% in women, respectively, and 8, 21, and 18.4% in men, respectively (table I).

After stratifying by age <40 and ≥40 years, the sensitivity for the detection of diabetes, high blood pressure and the metabolic syndrome was higher for the IDF thresholds compared with the AHA/NHLBI cutoff points whereas the positive predictive value was pretty similar for both definitions. In contrast, in both age groups, specificity and negative predictive value were better for the AHA/NHLBI cutoff points for all diseases. As for the LR(+) estimation in subjects ≥40 years old, when the AHA/NHLBI cutoff points were used, the values for diabetes, hypertension and metabolic syndrome were 1.34, 1.21 and 2.82, respectively whereas when the IDF cutoff points were applied the LR(+) were 1.1, 1.1 and 1.3, respectively. For both diabetes and hypertension a small value of the C-statistic whatever the waist circumference cutoff point used was observed. As for metabolic syndrome the C-statistic was higher when the AHA/NHLBI cutoff points (C-statistic=0.77) compared with the IDF cutoff points (C-statistic=0.61). In subjects <40 years old, the LR(+) for diabetes, hypertension and metabolic syndrome were 1.71, 1.29 and 3.69, respectively when the AHA/NHLBI cutoff points were used; while the LR(+) were 1.29, 1.25 and 1.5, respectively when the IDF cutoff points were applied. In this age group differences on the C-statistic were evident only for metabolic syndrome. (tables II and III).
In an additional analysis in subjects aged ≥65 years, when the AHA/NHLBI cutoff points were used, for diabetes and hypertension similar sensitivity (61.38 and 49.19%, respectively) and specificity (58.89 and 60.23%, respectively) with a significant increment on the positive predictive value (17.07 and 41.15%, respectively) compared with subjects aged ≥40 years was observed. For diabetes and hypertension the LR+ was 1.49 and 1.23, respectively. When the IDF cutoff points were applied, the sensitivity decreased modestly whereas the specificity increased; however, the LR+ was close to 1.
The age and sex-adjusted AUCs to identify subjects with diabetes, hypertension, and metabolic syndrome using the cutoff points suggested by the AHA/NHLBI and the IDF are shown in figure 1. The AUC for diabetes was significantly (p=0.0032) higher with the AHA/NHLBI cutoff points (AUC=0.61, CI95% 0.58-0.64) than with those of the IDF (AUC=0.57, CI95% 0.55-0.59). Similar results were observed for the metabolic syndrome using the AHA/NHLBI cutoff points (AUC=0.78, CI95% 0.77-0.79) as compared with those of the IDF (AUC=0.65, CI95% 0.64-0.66) (p<0.0001). Regarding the AUCs for hypertension, no significant differences were noted.
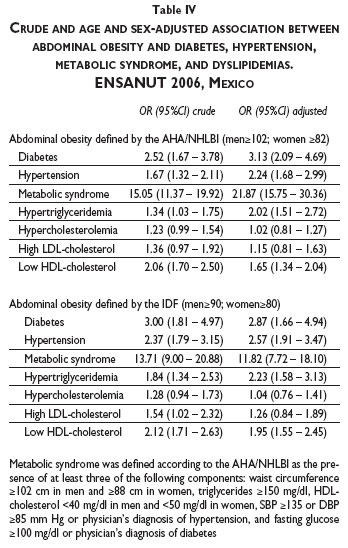
Age and sex-adjusted significant association between diabetes, hypertension, and metabolic syndrome and abdominal obesity defined by the AHA/NHLBI was observed. Subjects with abdominal obesity were 3.13 (CI95% 2.09-4.69) times more likely to have diabetes, 2.24 (CI95% 1.68-2.99) times more likely to have hypertension, and 21.87 (CI95% 15.75-30.36) times more likely to have metabolic syndrome than were subjects without obesity. When using the IDF criterion to define abdominal obesity, we observed that the association between abdominal obesity and the three diseases was weaker than that found with the AHA/NHLBI definition, particularly for metabolic syndrome (OR=11.82, CI95% 7.72-18.10) (table IV).
The use of the AHA/NHLBI definition for abdominal obesity revealed that in Mexico there are about 1.5 millions of undiagnosed cases of diabetes, 30% of which are younger than 40 years old. With respect to hypertension, there are about 1.5 millions of undiagnosed cases and 1.2 millions are younger than 40 years old. Finally, 7 million people have metabolic syndrome and 50% of them are younger than 40 years old.
Discussion
Mexico is undergoing an epidemic prevalence of chronic diseases as a result, in part, of the high prevalence of obesity in the last decades. In the present study, we observed that a high percentage of adult population with a waist circumference above the healthy level had at the same time undiagnosed diabetes, hypertension, or metabolic syndrome. When we examined the diagnostic power of abdominal obesity we found that the highest sensitivity and positive predictive value on the identification of these diseases was obtained with the IDF definition.
Several studies carried out in the 80s showed that the risk for cardiovascular complications increased linearly with a BMI greater than 25 kg/m2. while the increment was exponential with a BMI higher than 30 kg/m2. Recently, the independent effect of abdominal obesity on the risk for cardiovascular diseases was demonstrated in an analysis that included about one million participants.23
The usefulness of waist circumference as a screening tool for diagnosing chronic diseases is still on debate;8 however, its use on public health is based on its low cost and on results from investigations that showed its diagnostic and prognostic capacity for those conditions. The selection of the threshold to identify individuals at risk is influenced by ethnicity then the identification of specific cutoff points in specific population is required. Until now, it is not clear if the variation in cut-off points is a true biological phenomenon or an effect of the method for identifying optimal cut-off points. Regrettably, the IDF committee did not decide the abdominal obesity definition for Latin-Americans after analyzing population-based studies; they extrapolate information obtained in Asians.20 Furthermore, the AHA/NHLBI cutoff points were selected using information obtained mainly in Caucasians.19 Thus, analyses are required in study samples capable to represent Mexican adults. In addition, the properties of waist circumference as a screening tool should be explored confirmed.
Our results show that the IDF thresholds have a remarkably higher sensitivity than the AHA/NHLBI cutoff points; this is especially true in cases younger than age 40 and for the screening of diabetes and high blood pressure. In addition, this criterion has a high negative predictive value. However, the specificity of the IDF criteria is significantly lower, especially in individuals above age 40. The low specificity for the detection of diabetes or arterial hypertension becomes a concern in the older population; this rate is half of that observed in the younger group. As a result, the false positive rate increases from 63% to 79% when the waist circumference is applied in cases older than age 40, instead of young individuals. Overall, the AHA/NHLBI thresholds have a higher exactitude. The area under the ROC curve, and the predicted risk, is greater with the AHA/NHLBI definition of abdominal obesity for the detection of diabetes, hypertension and metabolic syndrome. However, the difference is not statistically significant for hypertension. In addition, the positive predictive values for the detection of diabetes or hypertension were not different between criteria.
The properties of waist circumference as a screening tool, rather than a prognostic variable, should be explored, since this is the most common indication in clinical practice. A screening tool should be highly sensitive in the first step. Rare conditions requires a highly specific test; in contrast, the screening of common conditions (i.e. type 2 diabetes and arterial hypertension) may not be negatively impacted by a moderate specificity, meanwhile the cost of the test (or the subsequent evaluation) is not too high. The IDF definition of abdominal obesity has a remarkably higher sensitivity compared to the AHA/NHLBI criteria. This characteristic clearly makes the IDF criteria the option to be applied in clinical practice in Latin American countries with a high prevalence of undiagnosed diabetes and/or high blood pressure. However, the major weakness of the IDF criteria is the low specificity, which becomes a problem in subjects older than age 40. Clinicians should be aware of the high false positive rate of the test in this subset of the population. On the other hand, the IDF criteria have high negative predictive value. This characteristic helps practitioners to avoid additional testing for the diagnosis of diabetes in subjects with a waist circumference lower than 90cm for men and 80 cm in women. On the other hand, in clinical settings with limited resources to do diagnostic tests for diabetes, physicians may consider using the AHA/NHLBI criteria to select cases in which a glucose measurement is required among subjects older than age 40. Finally, it should be emphasized that the main limitation of waist circumference measurement is the lack of standardization of the health professionals.
In conclusion, our results showed that a high proportion of adults in Mexico with diabetes, hypertension and metabolic syndrome, mainly older that 40 years and with abdominal obesity, remain undiagnosed by a physician. The IDF criteria of abdominal obesity are a useful screening tool for the identification of these cases. However, its systematic use is limited by its high false negative rate, especially in cases older than age 40. Clinicians should be aware of these characteristics of the test to avoid excessive costs.
Acknowledgment
This study was supported by the Ministry of Health of Mexico and the National Institute of Public Health in Mexico. The authors would like to thank the ENSANUT 2006 group, which developed the methodology of the survey. We also acknowledge all persons who accepted to participate in the survey.
References
1. Carey VJ, Walters EE, Colditz GA, Solomon CG, Willett WC, Rosner BA, et al. Body fat distribution and risk of non-insulin-dependent diabetes mellitus in women. The Nurses' Health Study. Am J Epidemiol 1997;145:614-619. [ Links ]
2. Wild SH, Byrne CD. ABC of obesity. Risk factors for diabetes and coronary heart disease. BMJ 2006;333:1009-1011. [ Links ]
3. Kannel WB, D'Agostino RB, Cobb JL. Effect of weight on cardiovascular disease. Am J Clin Nutr 1996;63(3 Suppl):S419-S422. [ Links ]
4. Hu D, Xie J, Fu P, Zhou J, Yu D, Whelton PK, et al. Central rather than overall obesity is related to diabetes in the Chinese population: the InterASIA study. Obesity (Silver Spring) 2007;15:2809-2816. [ Links ]
5. Janiszewski PM, Janssen I, Ross R. Does waist circumference predict diabetes and cardiovascular disease beyond commonly evaluated cardiometabolic risk factors? Diabetes Care 2007;30:3105-3109. [ Links ]
6. Lin WY, Lee LT, Chen CY, Lo H, Hsia HH, Liu IL, et al. Optimal cut-off values for obesity: using simple anthropometric indices to predict cardiovascular risk factors in Taiwan. Int J Obes Relat Metab Disord 2002;26:1232-1238. [ Links ]
7. Schneider HJ, Glaesmer H, Klotsche J, Böhler S, Lehnert H, Zeiher AM, DETECT Study Group. Accuracy of anthropometric indicators of obesity to predict cardiovascular risk. J Clin Endocrinol Metab 2007;92:589-594. [ Links ]
8. Klein S, Allison DB, Heymsfield SB, Kelley DE, Leibel RL, Nonas C, et al. Waist circumference and cardiometabolic risk: a consensus statement from shaping America's health. Diabetes Care 2007;30:1647-1652. [ Links ]
9. Rankinen T, Zuberi A, Chagnon YC, Weisnagel SJ, Argyropoulos G, Walts B, et al. The human obesity gene map: the 2005 update. Obesity (Silver Spring) 2006;14:529-644. [ Links ]
10. Hill JO, Peters JC. Environmental contributions to the obesity epidemic. Science 1998;280:1371-1374. [ Links ]
11. Vázquez-Martinez JL, Gómez-Dantés H, Gómez-García F, Lara-Rodríguez MA, Navarrete-Espinosa J, Pérez-Pérez G. Obesity and overweight in IMSS female workers in Mexico City. Salud Publica Mex 2005;47:268-275. [ Links ]
12. Sánchez-Castillo CP, Lara JJ, Villa AR, Escobar M, Gutiérrez H, Chávez A, James WPT. Unusually high prevalence rates of obesity in four Mexican rural communities. Eur J Clin Nutr 2001;55:833-840. [ Links ]
13. Williams K, Stern MP, Gonzalez-Villalpando C. Secular trends in obesity in Mexico City and in San Antonio. Nutr Rev 2004;62(7 Pt 2):S158-S162. [ Links ]
14. Flores-Huerta S, Acosta-Cázares B, Gutiérerz-Trujillo G. Prevalencia de peso bajo, sobrepeso, obesidad general y obesidad central. Rev Med Inst Mex Segur Soc 2006;44(Supl 1):S55-S62. [ Links ]
15. Arroyo P, Fernández V, Loria A, Pardio J, Laviada H, Vargas-Ancona L, et al. Obesidad, morfología corporal y presión arterial en grupos urbanos y rurales de Yucatán. Salud Publica Mex 2007;49:274-285. [ Links ]
16. SSA. Encuesta Nacional de Enfermedades Crónicas. México, DF. Secretaría de Salud. 1993. [ Links ]
17. Olaiz G, Rojas R, Barquera S, Shamah T, Aguilar C, Cravioto P, et al. Encuesta Nacional de Salud 2000. La Salud de los Adultos. México: Instituto Nacional de Salud Pública, 2006. [ Links ]
18. Olaiz G, Rivera J, Shamah T, Rojas R, Villalpando S, Hernández M, et al. (ed). Encuesta Nacional de Salud y Nutrición 2006. México: Instituto Nacional de Salud Pública, 2006. [ Links ]
19. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the Metabolic Syndrome. An American Heart Association/National Heart, Lung, and Blood Institute. Scientific Statement. Circulation 2005;112:2735-2752. [ Links ]
20. Alberti KG, Zimmet P, Shaw J, IDF Epidemiology Task Force Consensus Group. The metabolic syndrome: a new worldwide definition. Lancet 2005;366:1059-1062. [ Links ]
21. Rojas R, Aguilar-Salinas CA, Jiménez-Corona A, Shama-Levy T, Rauda J, Ávila-Burgos L, et al. Metabolic syndrome in Mexican adults. Results from the National Health and Nutrition Survey 2006. Salud Publica Mex 2010;52(suppl 1):S11-S18. [ Links ]
22. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988;44:837-845. [ Links ]
23. Berrington-de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med 2010;363:2211-2219. [ Links ]
 Correspondence to autor:
Correspondence to autor:
Dra. Aída Jiménez-Corona.
Instituto Nacional de Salud Pública.
Av. Universidad 655, col. Santa María Ahuacatitlán.
62100, Cuernavaca, Morelos, México.
E-mail: ajimenez@correo.insp.mx
Received on: August 5, 2011
Accepted on: October 11, 2011
Declaration of conflict of interests: The authors declare that they have no conflict of interests.














