INTRODUCTION
In March 2020, the World Health Organization declared that the new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection was a global pandemic1. Severe COVID-19 disease develops in vulnerable populations that include the elderly, patients with chronic diseases such as diabetes mellitus (DM), hypertension, chronic kidney disease (CKD), neoplastic and autoimmune entities requiring immunosuppressive therapy, obesity, and cardiovascular disease2.
End-stage renal disease (ESRD) patients on hemodialysis (HD) are a particularly relevant group vulnerable to this viral infection since their attendance to an HD center for treatment two or three times a week is mandatory, limiting their ability to isolate. Further, they are patients with multiple comorbidities that must travel to the HD units, often by public transportation; these patients are also exposed to infection in HD waiting rooms and are permanently in contact with the health personnel3,4. Therefore, the nephrology community throughout the world established guidelines in the early phases of the pandemic, to prevent and diagnose COVID-19 in a timely manner in this susceptible population4,5. In Mexico, we also dealt with two particular situations of local and global relevance; one was the high rate of infections among healthcare workers6 and the other was the type of epidemiological surveillance implemented during the pandemic7. Thus, our study aimed to determine the incidence, characteristics, and outcomes of SARS-CoV-2 infection in ESRD patients on HD and to describe the availability of confirmatory tests.
METHODS
This is a multicentric, observational, and prospective study conducted in 19 HD units in Mexico, in the following states: Mexico City, State of Mexico, Querétaro, Nuevo León (Monterrey City), Guanajuato, and Jalisco. The study was approved by the Local Ethics and Research Committee of the National Institute of Medical Sciences and Nutrition Salvador Zubirán, Mexico City (reference NMM-3360-20-21-1). Prevalent adult HD patients were included between March 2020 and March 2021. Data were collected for each center on sheet forms designed specifically for the study purpose (Table S1). Variables included: demographic features, comorbidities, clinical data at presentation, the need for hospitalization, and outcomes (discharge or death).
Operational definitions
Suspicious COVID-19 case
A patient who in the past 10 days has presented at least one of the following signs and symptoms: cough, dyspnea, fever, or headache, associated with at least one of the following: myalgias, arthralgias, sore throat, chills, chest pain, rhinorrhea, polypnea, anosmia, dysgeusia, or conjunctivitis8.
Confirmed COVID-19 case
A patient that fulfills the operational definition of a suspicious case and had a laboratory-confirmed PCR-RT diagnosis emitted by the National Public Health Laboratory Network (Red Nacional de Laboratorios de Salud Pública), recognized by the Institute of Diagnostic and Epidemiological Reference (Instituto de Diagnóstico y Referencia Epidemiológicos, InDRE)8.
Statistical analysis
Categorical variables are represented as frequencies and proportions, and the χ2 test was used for comparisons. Continuous variables are presented as means and standard deviations (SD, ±) and were analyzed with Student's t-test or median and interquartile ranges (IQR), and with the Mann–Whitney U-test according to their distribution. All analyses were performed with SPSS 25.0 (Chicago, IL) software. A two-tailed p-value below 0.05 was considered statistically significant.
RESULTS
Incidence of SARS-CoV-2 infection and baseline characteristics
Throughout the study period, 955 suspicious cases of SARS-CoV-2 infection were detected in patients from 19 HD units in the country; this is equivalent to 16.5% of a total population of 5779 prevalent HD patients. Infection was confirmed by reverse transcription polymerase chain reaction (RT-PCR) in 483 (50.6%) of the 955 cases, and 472 (49.4%) were highly suspicious yet they lacked a confirmatory PCR test, or the results were not reported to the HD unit. Demographics and comorbidities are shown in Table 1. When suspicious cases without a confirmatory test were compared with the confirmed cases, the latter patients were older (54 vs. 50 years, p < 0.001), and there was a greater proportion of patients with DM (62% vs. 42%, p < 0.01) and ischemic heart disease (13% vs. 5%, p = 0.02).
Table 1 Clinical characteristics and outcomes of confirmed and suspicious patients with COVID-19
| Characteristics | All patients (n=955) | Confirmed (n=483) | Suspicious (n=472) | p-value |
|---|---|---|---|---|
| Age, years (mean ± SD) | 52 ± 16 | 54 ± 16 | 50 ± 16 | < 0.01 |
| Male, n (%) | 526 (55) | 279 (58) | 247 (47) | 0.12 |
| Diabetes, n (%) | 250/458 (55) | 184/299 (62) | 66/159 (42) | < 0.01 |
| Hypertension, n (%) | 328/458 (72) | 219/299 (73) | 109/159 (69) | 0.28 |
| Obesity, n (%) | 40/432 (9) | 31/279 (11) | 9/153 (6) | 0.07 |
| Ischemic heart disease, n (%) | 42/410 (10) | 35/277 (13) | 7/133 (5) | 0.02 |
| Use of RAAS inhibitors, n (%) | 85/412 (9) | 61/218 (30) | 24/133 (18) | 0.37 |
| Hospitalization, n (%) | 426 (45) | 285 (59) | 141 (30) | < 0.01 |
| Length of hospitalization (days), (mean, IQR) | 12 (7-17) | 11 (6-15) | 5 (2-8) | 0.05 |
| Management in ICU, n (%) | 47 (5) | 32 (6.6) | 15 (3.2) | 0.02 |
| IMV, n (%) | 58 (6) | 41 (8.5) | 17 (3.6) | 0.01 |
| Mortality, n (%) | 255 (27) | 131 (27) | 124 (26) | 0.74 |
RAAS: Renin-angiotensin-aldosterone system; ICU: intensive care unit; IMV: invasive mechanical ventilation; IQR: interquartile range.
In terms of the number of cases throughout the year of the study, we observed two peaks: the first occurred between May and June 2020, and the second, between December 2020 and January 2021, and both coincided with an upsurge in cases in the country´s general population (Fig. 1). The evolution along time from March to February 2021, in the number of tests performed in hospitalized and non-hospitalized patients is displayed in the Supplementary Table 2. After November 2020, the number of diagnostic tests performed increased significantly, and also, significantly more suspicious cases treated as outpatients were also tested (Table S2).
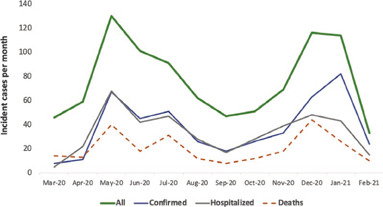
Figure 1 Incident cases by month in the period studied, confirmed, and hospitalized cases and deaths are specified.
Table 2 Comparative data of our HD population with other registries reported15-18 and with the general population of Mexico19 affected by COVID-19
| Characteristics | Our HD population | HD in Spain | HD in Switzerland | HD in Italy | HD in France | Mexican general population |
|---|---|---|---|---|---|---|
| Age, years (mean) | 52 | 65 | 71 | 72 | 72 | 43 |
| Male (%) | 55 | 64 | 65 | 62 | 64 | 50.1 |
| Diabetes (%) | 55 | 22 | 32 | 43 | 51 | 13.3 |
| Hypertension (%) | 72 | NA | 85 | 93 | 17.3 | |
| Obesity (%) | 9 | NA | NA | NA | 27 | 14.5 |
| Hospitalization (%) | 45 | 65 | NA | 63 | 48 | 18.7 |
| IMV (%) | 6 | 10 | NA | NA | 3 | 2.5 |
| Management in ICU (%) | 6 | 8 | NA | NA | 9 | 1.47 |
| Mortality (%) | 27 | 23 | 21 | 29 | 21 | 9 |
ICU: intensive care unit; IMV: invasive mechanical ventilation; NA: not available
Clinical presentation and actions implemented in HD units
The most often reported symptoms were cough (30%), fever (23%), dyspnea (20%), fatigue (18%), and diarrhea (9%). Table 2 shows the comparison between confirmed and suspicious cases. A greater proportion of confirmed cases developed fever (47 vs. 38%) and dyspnea (42 vs. 34%). Among patients followed on an ambulatory basis, 70% were isolated in separate areas of the HD unit; 27% were assigned to a specific shift for COVID-19 patients, and in the remaining 3% of patients, no changes were implemented. Positive or suspicious patients were isolated for an average of 13 ± 6 days.
Clinical course and outcomes
Among the 955 patients suspected of having COVID-19, 426 required hospitalizations for respiratory symptoms. A greater proportion of confirmed cases were hospitalized compared with those classified as suspicious (59% vs. 30%, p ≤ 0.001). Five percentages of the entire study population required management in an intensive care unit (ICU), particularly confirmed cases (6.6% vs. 3.2%, p = 0.022). Invasive mechanical ventilation (IMV) was also more frequently required in confirmed vs. suspicious patients (8.5% vs. 3.6%, p = 0.001) (Table 1). The overall mortality of the population was 27%. There was no between-group difference, and death occurred in 131 (27%) patients with a confirmatory RT-PCR while in the suspicious cases group, there were 124 deaths (26%).
DISCUSSION
This multicentric study of Mexican patients on HD revealed a 16.5% incidence of suspected COVID-19; yet, to our knowledge, only 50% of cases underwent confirmatory testing reported to the HD unit, in which they were being treated. If we only considered confirmed cases (8.3%), the incidence of SARS-CoV-2 infection would be falsely low in this high-risk population. However, if all cases are considered (suspicious and confirmed), an incidence of 16.5% appears to be more consistent with values reported in similar series in other countries (10-26%)9,10. Most documented cases developed in two distinct periods, May-June 2020, and December 2020-January 2021, and as expected, they coincided with the two waves or peaks of cases detected in Mexico.
The number of cases confirmed by RT-PCR is striking, since the population on HD is particularly vulnerable to developing severe COVID-19 and because their HD visits are mandatory, the probability of these patients transmitting the disease is high if pertinent measures are not implemented by the HD unit.
The percentage of patients lacking a confirmatory PCR test may be explained by two situations. The first is the epidemiological surveillance model implemented in the country. This particular model was chosen by the health authorities to optimize human and material resources at the beginning of the pandemic, thus minimizing the use of diagnostic tests. Under this model, a laboratory diagnosis was obtained in only 10% of cases with an ambulatory acute respiratory infection, and in 100% of patients with a severe, acute respiratory infection8 (in agreement with the findings of our study as of November 2020, Fig. 1). The second explanation for this high percentage of patients classified as suspicious (without an RT-PCR result) is that HD units would refer patients with symptoms to their corresponding hospitalization units; after their evaluation, their reference hospital did not provide a detailed summary of the patient's course nor did it explicitly communicate the result of an RT-PCR test; hence, the HD unit reported those patients as suspicious to our study's database. Either way, both situations must be minutely evaluated since they represent clear areas of opportunity for the country's health system to improve the availability of SARS-CoV-2 diagnostic tests, particularly among highly vulnerable populations, in which 100% of patients must have a confirmatory test, and to improve communication between hospitals and HD units. Our registry included patients before vaccination regimens were available in Mexico; many other reports have shown that this particular population develops less immunogenicity not only as a result of the underlying baseline immune suppression, but also due to the vaccine dosage, the interval between vaccines, and the type of administered vaccine11-14. Therefore, in this population, confirmatory tests for SARS-CoV-2 should always be performed when the disease is suspected.
The average age of our study population was lower than that reported in other populations on HD15-18 but clearly greater than that of the Mexican general population with COVID-1919 without CKD or renal replacement therapy. As expected, the most frequent comorbidities were DM, hypertension, obesity, and ischemic heart disease that, as we know, are highly prevalent in patients undergoing HD20,21. All these comorbidities are clear risk factors for the development of severe disease due to SARS-CoV-2.
The percentage of patients in need of hospitalization was lower than reported in other international studies that have evaluated this population15,17,18. However, as expected, the proportion of individuals with CKD requiring hospital admission is greater than that of the Mexican general population16, clearly reflecting these patients' vulnerability to developing severe COVID-19. Perhaps the low percentage of recorded hospitalizations was also due to a paucity of hospital beds at several moments during the pandemic. The percentage of HD patients who required IMV was lower than that reported for HD patients in Spain15; however, this value should be cautiously interpreted since, during pandemic peaks, a significant proportion of patients in need of IMV had no access to an ICU nor to a ventilator due to hospital saturation22. In comparison, the need for IMV in the Mexican general population was 2.5%19.
Finally, the mortality in our study population was similar to that reported among HD populations in other countries (18-30%)21,23-25, but clearly above the one observed in the Mexican general population19. Interestingly, there was no difference in mortality between confirmed and suspicious cases, suggesting that perhaps, most if not all suspicious patients actually had COVID-19 despite the lack of a confirmatory RT-PCR test. It is important to recognize the assertiveness of the personnel in HD units that implemented isolation techniques in all cases, either suspected or confirmed, and despite the lack of confirmatory testing. This practice certainly prevented the transmission of SARS-CoV-2 to other patients and health-care personnel in most dialysis units.
This study only reflects results that were voluntarily submitted by a limited number of HD units in our country (19 units). We must therefore recognize that the incomplete report of some variables may preclude deeper analysis.
SUPPLEMENTARY MATERIAL
Supplementary data are available at Revista de Investigación Clínica online (DOI: 10.24875/RIC.23000002). These data are provided by the corresponding author and published online for the benefit of the reader. The contents of supplementary data are the sole responsibility of the authors.











 nueva página del texto (beta)
nueva página del texto (beta)


