INTRODUCTION
The risks of residing or visiting sites at a high altitude above sea level (usually considered if > 2500 m) and derived hypoxemia were gradually discovered throughout history but are also important to know the behavior of populations that live at moderate altitudes (between 1500 and 2500 m, but for some 2000 m to 2800 m above the sea level), where a large number of individuals live in several countries in the world, especially in Latin America. A recent review on the impact of moderate altitude was published1 dealing mainly with the impact on asthma, chronic obstructive pulmonary disease (COPD), pulmonary hypertension, and sleep apnea. Basic mechanisms of acclimatization to moderate altitude centered on studies done in Latin America were also reviewed recently2.
This review is primarily focused on the impact on patients with respiratory and cardiovascular health with temporary or long-term exposure to moderate altitudes, but also on previously normal individuals reporting adverse events on visiting places or cities at moderate altitudes.
SEARCH PROCEDURE
To gather the information, we searched publications in PubMed with the following keywords: Altitude, mountain sickness (acute and chronic), high altitude pulmonary edema (HAPE), high altitude cerebral edema (HACE), arterial blood gases, hypoxemia, combined with Mexico, City of Mexico, Latin America, or moderate altitude. Furthermore, we searched Google scholar web pages in Spanish with the equivalent terms, to find articles primarily of Latin American origin published in local or regional journals not incorporated into PubMed.
IMPACT OF MODERATE ALTITUDE ON GENERAL HEALTH AND RESPIRATORY DISEASES
The population that permanently inhabits sites with moderate altitude is considerable in the world and Latin America, especially in Peru and Bolivia3. An estimate of 140 million people lives in the world at altitudes > 2500 m4 including 25% of Peruvians, and 4.5% of Mexicans. In Mexico, 50% of the population lives at altitudes > 1500 m5. The Cities of Mexico, Puebla, and Tlaxcala with altitudes of around 2200 m and Zacatecas and Pachuca of 2400 m are examples of Mexican cities where a large population is concentrated at moderate altitudes. Settlements located at similar altitudes abound in Latin America. Above 2500 m, al high altitude, several large cities are also located: for example, Cuenca Ecuador (2550), Soacha and Sogamoso Colombia and Cochabamba Bolivia (2570), Toluca Mexico (2650 m), Bogotá Colombia (2640 m), Quito Ecuador (2850 m), Cusco Peru (3400), and La Paz Bolivia (3690 m).
With altitude, the partial pressure of oxygen progressively drops in the air and the arterial blood, as well as the environmental temperature and humidity, whereas the presence of ultraviolet radiation increases. The impact of altitude on several diseases depends on the interplay of these factors (Table 1). The lower temperature and humidity at altitude eliminates, for practical purposes, the “tropical diseases” (malaria, typhus, and diarrheal diseases) and considerably reduces allergens and allergic reactions, as several of them for example, fungus, and mites, are favored by hot temperatures and high humidity. This has been one of the great health advantages of residing at moderate altitude. On the other hand, altitude increases skin damage by ultraviolet radiation, which may lead to skin cancer6.
Table 1. Conditions associated with altitude
| In the non-acclimatized |
| Acute mountain sickness: cerebral form and pulmonary form |
| Peripheral edema |
| Retinopathy and high altitude retinal hemorrhage |
| Thromboembolism |
| Periodic breathing |
| In the acclimatized |
| Chronic mountain disease (Monge's disease) |
| Re-entry high altitude pulmonary edema |
| Pregnancy and perinatal conditions |
| Conditions worsened with altitude |
| Deaths were due to pneumonia-influenza, COPD, and other chronic respiratory diseases. |
| Pregnancy and Perinatal abnormalities |
| Persistent ductus arteriosus and glomus tumor |
| Drepanocitic crisis and splenic infarction |
| Systemic and pulmonary hypertension (primary and secondary) |
| Ischemic heart disease and cerebrovascular diseases |
| Interatrial or interventricular septal defect |
| Common ailments at altitude |
| Dryness of airways (due to hyperventilation and low environmental humidity) often leads to persistent cough (altitude cough) |
| Altitude syncope |
| Headache |
| Conditions predisposing to acute mountain sickness |
| Absence of carotid bodies |
| Chronic respiratory diseases: COPD, neuromuscular weakness, sleep apnea, pulmonary fibrosis, and cystic fibrosis |
| Cardiac right to left shunts and pulmonary hypertension |
| Impact of altitude on patients with pulmonary diseases |
| More ventilation (more dyspnea at same exercise) and hemoglobin |
| Reduction in aerobic capacity (estimated 9% in Mexico City) |
| More requirements for supplementary oxygen |
| Likely a reduced life expectancy |
| Conditions improved with altitude |
| Gastrointestinal diseases |
| Malaria and “tropical diseases” |
| Tuberculosis |
| Asthma and allergies |
COPD: chronic obstructive pulmonary disease.
Altitude hypoxia-induced hyperventilation increases insensible water loss, and a lower ambient temperature may exacerbate airway reactivity, triggered to a great extent by airways cooling and drying. Hyperventilation also increases the likelihood of dyspnea as the basal ventilatory requirements are higher than at sea level, taking a higher percentage of the ventilatory reserve, and this may be especially important to healthy individuals during exercise or to individuals with respiratory or cardiovascular disease (Table 1).
On the other hand, air density decreases with altitude, improving measurements depending on a turbulent flow such as peak expiratory flow, and maximal voluntary ventilation7.
The main adverse impact of altitude on health is secondary to, hypoxemia which favors mortality in acute respiratory diseases, in which there is no time for acclimatization (for example, pneumonia, severe influenza, ARDS, and COVID-19)8-10 (Fig. 1). Chronic respiratory diseases also present at altitude with greater hypoxemia11,12, which in principle would lead to increased mortality13 and more likely a requirement of supplementary oxygen14. It is also expected that other conditions with hypoxemia or hypoxia had higher frequency and worse outcomes such as perinatal mortality, nocturnal hypoxemia due to sleep apnea or pulmonary disease, and in consequence, lead to higher needs for chronic oxygen therapy.
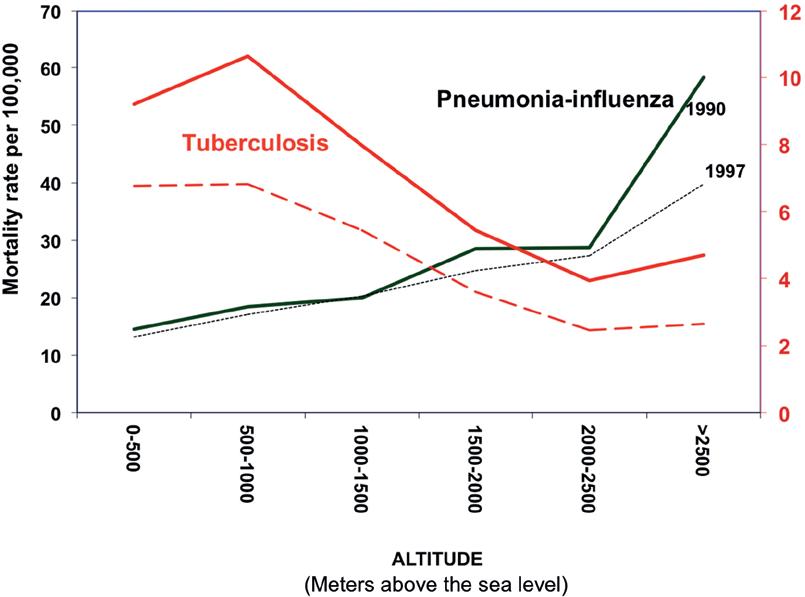
Figure 1. Mortality rate (per 100,000) due to tuberculosis (red lines) and pneumonia-influenza (black lines), in 1990 (continuous line) and 1997 (dashed line) in Mexico as a function of altitude above sea level. Mortality increases for pneumonia influenza and other diseases such as perinatal mortality but decreases consistently for tuberculosis.
The PLATINO study designed primarily to estimate the prevalence of COPD was conducted in five cities in Latin America at different altitudes (Montevideo, Sao Paulo, Santiago, Caracas, and Mexico): the main determinant of hypoxemia was the altitude of residence above sea level15. Hypoxemia (SpO2 ≤ 88%) with or without chronic oxygen therapy was found basically in people residing in Mexico City15. The other risk factors for hypoxemia in PLATINO were older age, high body mass index, and abnormal spirometry15.
Especially, hypoxemic are those patients combining several risk factors, the so-called overlap syndromes, for example, obese individuals residing at altitude, with sleep apnea, and who also have COPD or interstitial lung disease or both11,12. These patients with overlapping risk factors for hypoxemia, form, without doubt, a priority group for treatment, and supplemental oxygen. Sleep hypoxemia at moderate altitude is extremely common and may be severe (Fig. 2). Patients with sleep apnea often need supplementary oxygen in addition to continuous positive airways pressure the standard treatment. Simulated ascent to 2750 m of altitude of patients with sleep apnea increased hypopneas and Cheyne-Stokes breathing and decreased obstructive apneas16. Periodic breathing is uncommon in adult residents of Mexico City.

Figure 2. Sleep-induced oxygen desaturation in patients with idiopathic lung fibrosis studied at sea level (black lines) and Mexico City (red dashed lines), matched by lung function (vital capacity). Oxygen desaturation is substantially worse in Mexico City, from left to right, when awake, in Non-REM sleep, REM sleep, and at minimal SaO2 during sleep.
TUBERCULOSIS AT ALTITUDE
At altitude, the rate of infection, disease, and death due to tuberculosis is reduced9,17,18, probably because the mycobacterium tuberculosis is an obligate aerobic organism, but other environmental aspects such as lower humidity, temperature, and ultraviolet radiation could contribute (Fig. 1). These findings lend credence to the selection of sites at moderate altitudes to build sanatoriums for tuberculosis patients since the mid-nineteenth century, including the first in Mexico, the sanatorium for tuberculosis of Huipulco at 2240 m altitude, the current headquarters of the National Institute of Respiratory Diseases. A similar transformation occurred in other tuberculosis sanatoriums in Latin America. Altitude could improve now individuals with drug-resistant tuberculosis, as happened apparently in the pre-chemotherapy tuberculosis era with prolonged stays in sanatoria.
OTHER HEALTH PROBLEMS AT ALTITUDE
Conditions more frequent at altitude include paragangliomas, glomus tumors19,20, and patent ductus arteriosus21,22. Visitors to moderate altitudes may have a sympathetic response with an increase in blood pressure and heart rate that may decompensate susceptible individuals23,24.
On the other hand, beneficial effects of a hiking vacation at moderate altitudes on metabolic syndrome have been described25, but are difficult to separate the improvement due to altitude, and that due to exercising and other healthy habits incorporated.
Asthma prevalence and incidence tend to decrease with altitude26,27 as well as its severity. Asthmatic patients likely improve moving to higher altitudes if triggered by allergens such as mites and fungi, but also patients with non-allergic asthma28, whereas those with exercise-induced asthma may worsen with altitude due to lower temperatures and humidity, especially in competitive athletes.
Mortality due to COPD rises with altitude29-31: patients experience increased hypoxemia32, especially during sleep11. In addition, increased ventilatory needs may lead to exercise ventilatory limitation32 and more dyspnea for any workload. The need for oxygen and the presence of pulmonary hypertension33 increases in altitude residents compared with patients residing at sea level at the same lung function abnormality. Unfortunately, no vasodilator treatment for pulmonary hypertension in COPD demonstrated a significant improvement in mortality, and even an improvement in the 6 min walking distance has been inconsistent34.
Acute hypoxemia due to altitude exposure leads to immediate increases in pulmonary artery pressure due to hypoxic vasoconstriction. However, prolonged exposure to altitude hypoxemia may lead to structural changes or remodelation in the pulmonary circulation that become irreversible even with oxygen therapy. Pulmonary hypertension may lead to right heart failure and cor pulmonale with increased mortality. In addition, pulmonary hypertension of several origins may worsen at moderate altitudes.
IMPACT OF ALTITUDE ON PaO2/FIO2 AND OXYGENATION INDICES
Acute respiratory injury is defined by radiological opacities and acute hypoxemia, quantified by a decrease in the PaO2/FIO2 ratio35. This quotient is a popular index of oxygenation in acute lung disease that requires only arterial blood for its estimation, while the most reliable venoarterial shunt requires arterial and mixed venous blood (blood from the pulmonary artery with a Swan-Ganz catheter) or the shunt measured with other methods. However, the PaO2/FIO2 ratio is modified by FIO2 and altitude36, a situation that can easily be understood by thinking that FIO2 is constant in ambient air at different altitudes, while the PaO2 is inexorably falling on ascending from sea level. At the same level of lung damage, the quotient falls with altitude, and conversely, at the same level of PaO2/FIO2, patients who reside at sea level have more lung damage than residents at moderate altitudes (Fig. 3). In other words, to make a comparison of patients residing at different altitudes at an equivalent degree of lung damage (at the same shunt), an adjustment to the measured PaO2/FIO2 ratio is required37. The adjustment raises the PaO2/FIO2 of patients at altitude to make them comparable to those at sea level.

Figure 3. PaO2/FIO2 at sea level (black line) and 2000 m above sea level (red line) as a function of the veno-arterial shunt (horizontal axis). Notice that PaO2/FIO2 drops with increasing shunt and with altitude. The presence of a PaO2/FIO2 of 300mmHg, a common threshold to identify clinical significant gas exchange abnormality, represents different shunts and therefore lung damage at different altitudes: at sea level shunt is 19% and at Mexico city (2240 m) is 13%.
MOUNTAIN SICKNESS AT MODERATE ALTITUDES
Altitude sickness, acute or chronic, generally referred to as mountain sickness, occurs in people free of lung disease and leads to health problems that solve by going down to a place closer to sea level, or by giving oxygen. Mountain sickness is a consequence of acute or chronic hypoxemia. Of course, similar phenomena could also occur in obese people or those with respiratory disease, but the causality of altitude would be less clear-cut than if happens in previously healthy individuals. This type of ailment occurs more frequently above 2500 m, and especially above 3000 m, reached by road rapidly when visiting several touristic centers in many countries. The fact that they are more frequent among residents or visitors to sites above 3000 m does not mean that they are impossible at moderate altitudes such as the valley of Mexico at 2240 m. In reality, altitude is a continuous risk that occurs progressively. In fact, in acute exposures to altitude (by decompression chambers), subtle changes in visual and neuropsychological performance are identified above 1500 m in some individuals38. Syncope in otherwise healthy young individuals visiting from sea level is also reported at 2770 m above sea level, compared with residents39.
In addition, patients with hypoxemia or cardiopulmonary problems (Table 1) may be exacerbated if ascend from sea level to moderate altitudes and should consider the use of supplementary oxygen.
Transient exposures to high altitudes are now more common and dangerous. Near Mexico City, several parks are at considerable altitudes and can be reached quickly by car: the Nevado de Toluca National Park, with an altitude up to 4680 m, the Izta-Popo national park, at 3400 m, or Tlamacas, at 3900 m: the three include hikes above that altitude, that may constitute a substantial risk not only for patients, but also for some individuals even if previously healthy, and unfortunately often unaware of these risks.
ACUTE MOUNTAIN SICKNESS (AMS)
The most common acute forms of altitude illness are AMS, and the potentially fatal-extreme forms: HAPE and HACE, all responding to descent or oxygen therapy. In South America, AMS has been called Soroche, and it is a syndrome that is characterized by headache, nausea, malaise, occasionally fever, and vomiting that occur after rapid ascent to a considerable altitude but can occur at moderate altitudes40,41. In ski resorts at moderate altitudes similar to those in Mexico City up to 12% of visiting lowlanders develop AMS40,41, and is considered relatively common above 1800 m (6000 feet). It is, therefore, expected that a proportion of travelers arriving mainly at the airport in Mexico City (2240 m) and even more in Toluca (2600 m) from sea level, or to other cities at similar altitudes, meet the criteria of AMS obtained with standardized questionnaires42. In its most severe forms, AMS derive in HACE, cerebral form of AMS or HAPE, pulmonary form of AMS, both caused by hypoxemia leading to marked and heterogeneous vasoconstriction, endothelial dysfunction (poor nitric oxide production and excessive endothelin), and reduced fluid clearance, all significantly favored by genetic predisposition leading to fluid leakage and expansion of the extracellular space. Although there is a wide variation in the capacity to acclimatize, all individuals would develop AMS if exposed quickly to hypobaric hypoxia of sufficient magnitude.
PULMONARY EDEMA OF ALTITUDE
HAPE occurs usually above 2500 m in people who reside at sea level, and who have a predisposition characterized by intense hypoxic pulmonary vasoconstriction, but can present at moderate altitudes43-45. Doing on arrival intense exercise before acclimatization has been considered a risk factor, deriving a higher cardiac output in areas with less hypoxic vasoconstriction, but also risky are past episodes of AMS, HAPE, or HACE, rapid rate of ascent, and cardiorespiratory comorbidities.
In Mexico City (and in Toluca at 2600 m) and other cities at similar altitudes, there have been reports of high-altitude pulmonary edema of a particular type called re-entry HAPE, a recurring condition in the same individuals when they travel to sea level and return to altitude46,47 (Fig. 4). It occurs occasionally in young residents at moderate altitude who travel at sea level for several days or weeks and return by plane, especially if they are physically active (Fig. 4). They develop pulmonary edema in the 1st h after arrival, usually interpreted as multifocal pneumonia, but with the peculiarity of presenting a rapid improvement with oxygen and clearing of the opacities in a short time, 1-2 days, which is unexpected in infectious pneumonia.

Figure 4. Chest roentgenograms of two healthy physically active young patients with re-entry high altitude pulmonary edema (HAPE), the third attack in a 13-year-old woman (upper roentgenograms A and B) and the second is a 16-year-old male (C and D), at arrival (left) and 2 days later (right). Both show bilateral patchy alveolar opacities with normal heart shadow which cleared quickly after admission, Both lacked evidence of infection and had a normal echocardiogram.
The diagnosis of those patients usually is not clarified until the same event repeats under similar circumstances and a normal echocardiogram is documented with an absence of infectious markers or viral or bacterial cultures. Similar hemodynamic results are expected in re-entry-HAPE as those in patients with HAPE who reside near sea level48. It may be prevented by gradual slow ascent and if unfeasible, in individuals considered of high risk, by acetazolamide as well as vasodilators that may oppose hypoxic vasoconstriction including nifedipine and phosphodiesterase-5 inhibitors, as well as oxygen. Similar general preventive measures should be considered for HACE including medications acetazolamide or dexamethasone.
CHRONIC MOUNTAIN SICKNESS, MONGE'S DISEASE
Chronic mountain sickness has been considered the result of a loss of acclimatization to altitude and is manifested by exaggerated polycythemia for altitude often with severe hypoxemia, alveolar hypoventilation, pulmonary hypertension, and related symptoms such as dyspnea, fatigue, and headache. There is a report of a patient with chronic mountain sickness resident at 2000 m above sea level49, similar to that of Mexico City but there must be more. In the strict criterion, to be sure that altitude is the only causal factor, lung disease should be ruled out, but at present, it would be essential to eliminate obstructive sleep apnea, especially in obese patients, or the hypoventilation-obesity syndrome. Moving to sea level, receiving chronic oxygen therapy or Acetazolamide may help them.
ALTITUDE CHALLENGE TESTS
The ease of travel currently results in frequent exposure to considerable altitudes, which can be harmful to previously healthy people but especially for lung patients, since it can trigger severe hypoxemia. On the other hand, a variety of patients treated at moderate altitude centers may reside at sea level, or in places above 3000 m, and pulse oximetry or arterial blood gases measured in the city of evaluation, do not reflect the day-to-day condition of the patient.
To estimate more accurately the impact of a different altitude from the one in the evaluation site of a patient, it has been proposed to perform the so-called altitude challenge tests, in which an altitude is simulated by varying the FIO2 of a gas mixture, a much more accessible strategy than through an expensive hypohyperbaric chamber (Fig. 5). In the Valley of Mexico, it is relevant, for example, to simulate sea level and also an altitude of 3100 m, which is reached driving through almost all the exit highways of the Valley of Mexico50, 3100 m simulated by breathing in Mexico City a mixture with 18% and sea level, with 28% oxygen, respectively. These tests provide the immediate blood gases changes to the variation in altitude, information that is undoubtedly important, but which does not necessarily predict changes that would occur after acclimatization.
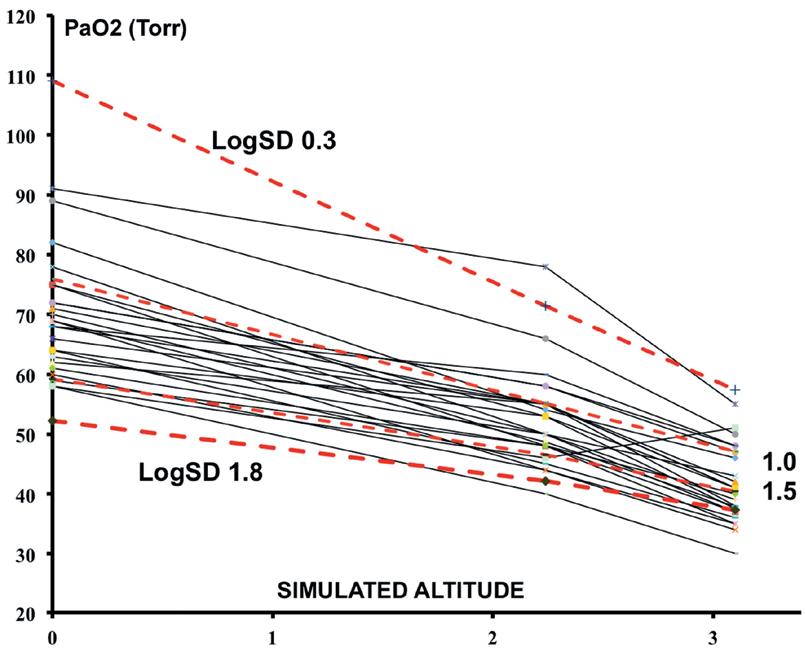
Figure 5. Altitude challenge tests in pulmonary patients (chronic obstructive pulmonary disease and pulmonary fibrosis) studied at 2240 m, simulating 3100 m (with FIO2 0.18), and sea level (with FIO2 0.28). Red dashed lines represent levels of V/Q mismatch (logSD values 0.3 normal, 1.0 moderate, and 1.5 and 1.8 severe) in lung models of gas exchange. The observed drop of PaO2 was on average 9 mm per km of increase in altitude, consistent with a moderate V/Q mismatch. At simulated 3100 m, reached on leaving Mexico City by highways, the majority of the patients, had a SaO2 < 90%.
In Mexico City, it was estimated that for each 1000 m of altitude change, PaO2 is modified by 9 mmHg, for typical patients with COPD and pulmonary fibrosis50. This change is expected in models of gas exchange in the lungs with moderate abnormalities in the V/Q ratio distribution50.
The cabins of modern aircraft are pressurized to varying altitudes (1600-2400 m) so in a simplified, conservative way, the level of hypoxemia when using commercial flights can be approximated to the existing condition at around 2000 m or moderate altitudes if no more information is available. Otherwise, the impact of a different altitude can be estimated by calculating the altitude change of 9 mmHg/km.
In other words, if a patient residing at a moderate altitude requires supplementary oxygen, oxygen is also required during standard commercial flights.
RESEARCH ISSUES ON MODERATE ALTITUDE ON LUNG DISEASES AND ALTITUDE-ASSOCIATED ILLNESS
Some relevant research issues on acclimatization to moderate altitudes are described elsewhere2 A better knowledge of normal values for arterial blood gases at different altitudes and the factors, environmental or genetic, and impacting hypoxemia is important. Furthermore, important is to improve the knowledge of the whole integrated function required to produce energy, with the pulmonary, circulatory, and tissue components. A better understanding of the impact of altitude on mortality due to various diseases, overall life expectancy, reproduction, brain functioning, and requirements for oxygen therapy in different countries would help support patients.
Although in general, it is recommended to maintain the same criteria for oxygen prescription at different altitudes, in some countries, professional organizations decide to reduce the PaO2 required to receive oxygen, arguing for better tolerance to hypoxemia, which to our knowledge can only be hypothesized. Residing at moderate altitudes provides better tolerance to hypoxemia, at least in some circumstances51-53. For example, the inhabitants of Mexico City are more likely to reach the top of Popocatépetl volcano (5426 m) than those who try to reach it from sea level. Better tolerance to hypoxemia in patients could be demonstrated by a randomized controlled trial of oxygen with the same criteria as the Nocturnal Oxygen Trial14 unlikely to be approved or held.
Measurements more sound to evaluate hypoxemia need to be longer than just an instantaneous measurement of PaO2, for example, measurement of SpO2 during sleep, or 24 h, measurements at rest and exercise, or the traditional consequences of hypoxemia polycythemia and pulmonary hypertension. It is uncertain if activation of genes related to hypoxemia, hypoxia-induced factor (HIF), and those activated by HIF such as erythropoietin as a well-known example) could be of clinical value, but should be evaluated to identify physiologic responses to hypoxemia and hopefully identifying individually the optimal level of hypoxemia to prescribe oxygen.
A country or a city may select further requirements to provide home oxygen to those with more urgent requirements in scarcity conditions, those with the most severe hypoxemia, pulmonary hypertension, or polycythemia.
On the other hand, there is a lack of reliable data on the incidence of AMS in visitors to cities at moderate altitudes such as Mexico City and Toluca (in the State of Mexico), Bogotá, and Quito, that arrive quickly from sea level by plane. Another question is how frequent is the presence of HAPE between 2000 and 2800 m high, as in the Valley of Mexico and Puebla (Mexico), Toluca, Bogota, Quito, and sites at similar altitudes.
Of great interest also would be to study subjects with re-entry HAPE in cities at moderate altitude, including vascular and ventilatory responses to a challenge of hypoxemia.
The impact of altitude-induced hyperventilation on the damage caused by highly concentrated pollutants in the large cities of several Latin American cities and, where appropriate, the need to adjust permissible standards of contaminants for altitude is of great relevance for the best protection of the health of the inhabitants has been discussed previously2.
CONCLUSIONS
The health consequences of residing at moderate altitudes may be widespread and considerable and available information is very limited, especially that originated in Latin American countries. Patients with respiratory diseases living at moderate altitudes are more susceptible to severe deoxygenation, leading likely to rapid deterioration, with an urgent need for supplemental oxygen or moving to sea level. Altitude hyperventilation of the inhabitants increases their exposure to air pollutants. Acute or chronic mountain sickness may occur at moderate altitudes in susceptible individuals or those with additional causes of hypoxemia, more often than before, because of the common fast travel. The increased requirement of oxygen by itself becomes a heavy load on the already financially stressed health systems. The current pandemic of SARS-COV-2 leads to a widespread scarcity of supplementary oxygen and pulse oximeters, likely more important at moderate altitudes. Oxygen and measurements of oxygenation are key to consider in the health system, but vital for communities at altitude. Conversely, altitude has to be taken into account for planning health institutions and residences for the elderly among other things.











 nueva página del texto (beta)
nueva página del texto (beta)


