INTRODUCTION
In Mexico, where type 2 diabetes (T2D) is highly prevalent, and its incidence and mortality are increasing1-4, type 1 diabetes (T1D) is frequently overlooked and regarded as a low prevalence disease. Although the incidence and prevalence of T1D worldwide varies considerably, it is one of the most common chronic diseases in childhood5. It has been reported that patients living with T1D (PWT1D) receive suboptimal treatment for several years, increasing their possibility of developing chronic complications6. This situation leads to seeking care with private endocrinologists, increasing the out-of-pocket medical costs7. Until 2012, the only data available regarding T1D in Mexico reported in the DIAMOND Study, came from a small urban area in the State of Veracruz8. This report described a mean incidence rate of 1.15 (CI 0.75-1.9) per 100,000 individuals/year. Even though these results were not representative of the whole Mexican population, they positioned our country as one with the lowest incidence rate of T1D. Later, a study performed at the Mexican Social Security Institute (Instituto Mexicano del Seguro Social, IMSS) reported that the incidence of T1D among subjects younger than 19 years increased from 3.4 to 6.2/100,000 between 2000 and 20109. In fact, the data from Mexico included in the 2017 International Diabetes Federation (IDF) Atlas10, comes from this single study9. Data obtained from the 2017 morbidity yearbook from the Dirección General de Epidemiología reported an incidence rate of new cases of 5.45/100,000, showing a marked increase in the incidence rate from 1993 to 201711. However, the precise prevalence of T1D in Mexico is still unknown and there is virtually no information regarding characteristics at diagnosis, treatment, and follow-up.
To provide information on PWT1D, several large-scale population- and clinical center-based T1D registries have been generated. These registries include the DPV Scientific Initiative in Germany and Austria12, the EURODIAB study in Europe13, the DIAbetes MONDiale (DIAMOND)14 and the SWEET15 world-wide studies, the T1D Exchange Clinic Registry16, and the SEARCH for Diabetes Youth Study from the United States of America17,18. All these registries, as well as the IDF10,19, have documented an increase in the incidence and prevalence of T1D in the past 20 years. Nevertheless, none of these registries include Latin-American populations. The few studies are available in Mexico only address the situation of PWT1D in childhood and adolescence8,20, but not the long-term outcomes during adulthood6. To address this and to generate evidence about the characteristics of PWT1D in our country, the RENACED-DT1 (Registro Nacional de Pacientes con Diabetes Tipo 1, National Type 1 Diabetes Patient Registry) was developed. This registry focuses on obtaining health indicators to generate evidence on T1D prevalence, treatment practices, acute and chronic complications, and long-term follow-up21. We aim to describe the characteristics at diagnosis and at the last follow-up of patients recorded in this nation-wide registry, and to evaluate factors associated with adequate glycemic control (Glycated hemoglobin A1c, HbA1c <7%) and the presence of microvascular complications.
METHODS
Study population
The RENACED-DT1 is an initiative currently supported and endorsed by the Mexican Nutrition and Endocrinology Society (Sociedad Mexicana de Nutrición y Endocrinología, SMNE). The first version of the online database was created in 2014, based on the 1989 modified St. Vincent Declaration22. The registry gathers clinical and biochemical information from both private and public centers all over Mexico. All PWT1Ds are eligible to be included in the registry. Clinical diagnosis of T1D by a medical care provider, fulfillment of the ADA diagnostic criteria for diabetes with insulin requirement at diagnosis and thereafter was considered to establish T1D diagnosis. All adult participants signed a written informed consent and confidentiality agreement, which were also signed by the parents or guardians of participant children. In addition, all children provided assent to be included in the registry. The protocol was approved by the medical ethics committee of the Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán. This study followed the principles of the declaration of Helsinki.
Data collection
Data were collected and registered by the attending endocrinologist or an assistant, at each office visit, as an adjunct to the medical record. HbA1c concentration and other laboratory test results were also registered at each visit. Hypoglycemia was defined as glucose concentration < 70 mg/dL and severe hypoglycemia as an event with alteration of mental and/or physical functioning requiring assistance from another person for recovery. The presence of microvascular complications was determined by the attending physician (neuropathy), an ophthalmologist (retinopathy), and laboratory analysis (nephropathy) according to the 2017 American Diabetes Association Standards of Care23. All data were downloaded, de-identified, manually cleaned, and analyzed by a statistician/epidemiologist. All investigators had full access in the database.
Statistical analysis
For continuous variables, central tendency measures were calculated (means for variables with parametric distribution and median for variables with non-parametric distribution). For categorical measures, percentages and proportions were estimated. Differences between quantitative variables were analyzed with Student's t-test. Pearson's Chi-square for qualitative variables was performed. Logistic regression models were performed to explore factors associated with glycemic control and the presence of any chronic complications. The diagnosis and selection for our logistic regression model were conducted by assessing the lowest Bayesian information criterion (BIC) along with the highest R2. Statistical analyses were conducted using STATA version 11. Missing data were excluded from the statistical analyses. p < 0.05 was considered as statistically significant.
RESULTS
Population characteristics
We present the data of patients included between July 2014 and January 2018. Of the 1,035 individuals who have been enrolled during the study period, 64 declined participation and another six were excluded for incomplete data. We extracted and analyzed information of 965 adults and children living with T1D. Data were collected from 29 endocrinology centers distributed among 26 of the 32 Mexican States. Patients registered from Jalisco represented 24.4% of the cases, followed by Mexico City with 20%, Mexico State with 10%, and Nuevo León with 8.7% of the cases (Supplementary Figure S1). We observed that 564 (58%) were enrolled from private practices, whereas 401 (42%) were registered at public institutions; 222 (23%) at the Mexican Social Security Institute (IMSS), and 175 (18%) at clinics belonging to the Ministry of Health (SSA). The median age was 21 years (range 1-81 years). The median age at diagnosis was 11 years (IQR 7-15). We recorded that 85% (n = 772) of the patients were diagnosed before the age of 20 years, whereas 15% (n = 129) after the age of 20.
We observed a female predominance (61%) of registered patients (Supplementary Table S1). Among patients with available diagnosis date (n = 901), median diabetes duration was 8.2 years at enrollment, with 78 patients living with diabetes for 20-30 years and 38 for more than 30 years; 81% (n = 946) of these patients were diagnosed after the year 2000. Fifty-four percent of the patients were hospitalized at diagnosis (n = 282/520 with available information); of those, 72% (n = 204/282) presented diabetic ketoacidosis (DKA) and 17% (n = 47/282) required admission to the intensive care unit. A family history of T1D was reported by 13% of the patients, present in a first-degree family member in only 2%. A family history of T2D was reported by 58% of the participants, and a first-degree family member with T2D was reported by 11%.
Biochemical and anthropometric characteristics
Mean HbA1c registered at enrollment was 8.9 ± 2.2% (74 ± 24 mmol/mol), 16.3% of the patients having an HbA1c concentration below 7% (53 mmol/mol), and 40.8% above 9.0% (75 mmol/mol). In the last follow-up, the mean HbA1c was 8.7 ± 2.1% (72 ± 23 mmol/mol), with 18% of the participants having an HbA1c below 7.0% (53 mmol/mol) and 35% above 9.0% (75 mmol/mol) (Supplementary Table S1). Figure 1 shows HbA1c at the last follow-up according to age categories.
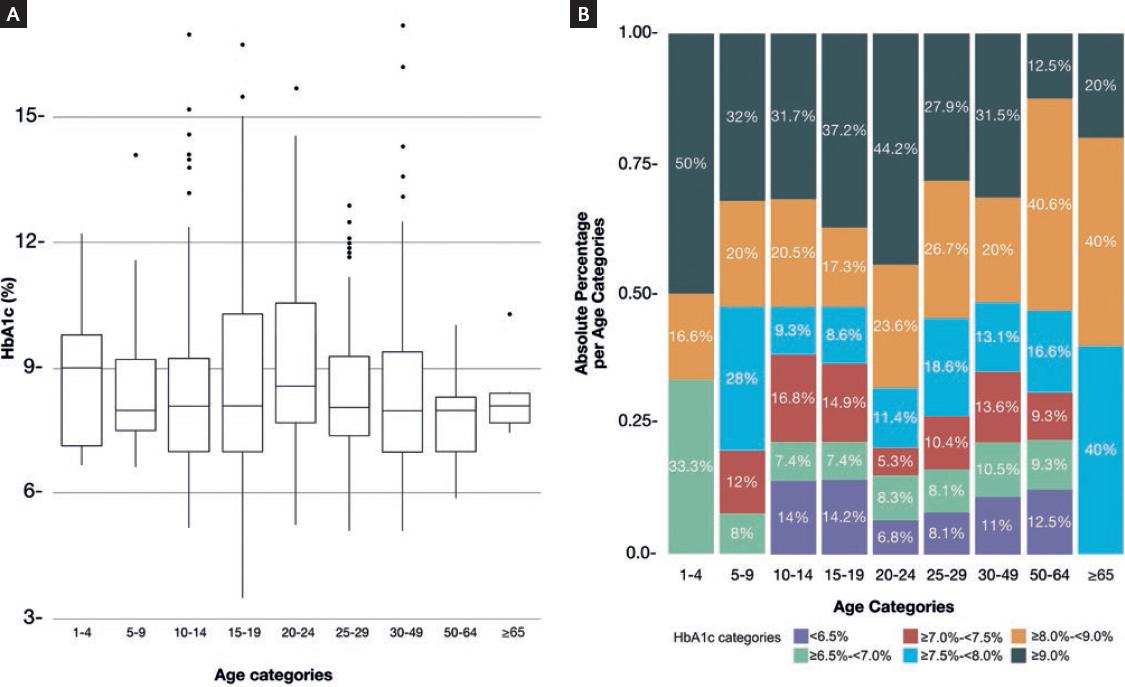
Figure 1 Box-plot of HbA1c levels in the RENACED-DT1 database stratified by age categories (A). Proportion of HbA1c categories according to age categories in the RENACED-DT1 (B).
Height and weight information were recorded in 469 patients, of whom 42.4% had overweight or obesity (≥ 85th percentile for ages 2-< 20, and ≥ 25 kg/m2 for ages ≥ 20) and 8.1% had obesity (≥ 95th percentile for ages 2-< 20 and ≥ 30 kg/m2 for ages ≥ 20). At the last follow-up visit, 44.3% had overweight or obesity and 8.9%, obesity.
Treatment and glucose monitoring
Among patients with treatment information available (n = 750), 61% were on basal-bolus therapy by injection with insulin analogs, 21% were insulin pump users and 9% were using real-time continuous glucose monitoring (CGM) (Supplementary Table S1). These two latter were more common in patients with private medical care. Self-monitoring of blood-glucose (SMBG) ≥ 4 times/day was performed in 33.3% of patients.
Associated factors related to adequate glycemic control
At the last follow-up (n = 545), mean HbA1c levels on insulin pump users (n = 144) were 7.9 ± 1.4% (62 ± 15.3 mmol/mol), whereas in those treated by basal-bolus injections (n = 401) the mean HbA1c was 8.8 ± 2.2 (73 ± 23 mmol/mol) (p < 0.01). Figure 2 shows the percentage of patients on basal-bolus injections or insulin pump with HbA1c < 7% (< 53 mmol/mol), 7-8.9% (53 mmol/mol-75 mmol/mol) and n 9% (75 mmol/mol).
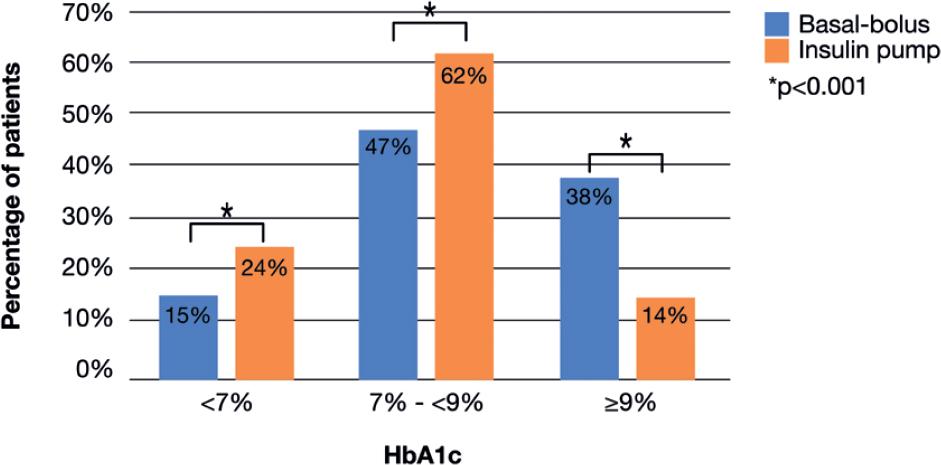
Figure 2 Percentage of patients with HbA1c <7% (<53 mmol/mol), 7 to <9% (53 mmol/mol-75 mmol/mol) and ≥ 9% (75 mmol/mol) according to the treatment regimen: basal-bolus regimen (blue), insulin pump therapy (orange), in RENACED-DT1 National Registry.
The bivariate analysis showed an association with lower HbA1c levels and private health-care setting, insulin pump use, CGM use and SMBG ≥ 4 times/day. After adjusting for sex, education, age and time since diagnosis (≥ 10 years), only SMBG ≥ 4 times/day remained associated with better glycemic control: adjusted odds ratio (AOR), 2.62 (95% confidence interval [CI], 1.13-6.04) (Table 1).
Table 1 Multivariate logistic regression analysis for adequate glycemic control (HbA1c <7%)
| Beta | SE | OR (95% CI) | p | |
|---|---|---|---|---|
| SMBG ≥ 4 times/day | 0.96 | 0.43 | 2.62 (1.13-6.04) | 0.024 |
| Insulin pump use | 0.53 | 0.54 | 1.69 (0.59-4.88) | 0.328 |
| CGM use | 0.67 | 0.64 | 1.95 (0.56-6.81) | 0.293 |
| Time since diagnosis (≥ 10 years) | -0.17 | 0.40 | 0.85 (0.39-1.84) | 0.675 |
| Private health-care setting | -0.25 | 0.47 | 0.78 (0.31-1.98) | 0.607 |
| Female | 0.23 | 0.41 | 1.26 (0.57-2.82) | 0.569 |
| Completed High School | 0.25 | 0.41 | 1.28 (0.57-2.88) | 0.550 |
SMBG: self-monitoring of blood glucose; CGM: continuous glucose monitoring; BIC:228.49; R2 = 0.0564.
Chronic complications and related factors
Of the 901 individuals with a registered diagnosis date, we recorded 12.0% (n = 108) of patients with any chronic complication; 6.3% (n = 57) reported diabetic neuropathy, followed by diabetic retinopathy in 5.4% (n = 49) in and diabetic nephropathy in 4.6% (n = 41) in our population of study (Table 2). As expected, with increased diabetes duration, the proportion of patients with chronic complications increased, with up to 45% (n = 17/38) in those with >30 years of diabetes duration (Table 2). In our logistic regression models, we found that time since diagnosis (> 10 years), female sex, obesity status, SMBG < 4 times/day, and the presence of hypoglycemia were associated factors to any chronic complication. After adjusting for HbA1c, private health-care setting, insulin pump use and CGM use, the association of the previously mentioned variables persisted (Table 3).
Table 2 Presence of chronic diabetes complications (nephropathy, neuropathy and retinopathy) according to type 1 diabetes duration, in RENACED-DT1 National Registry
| Diabetes duration at enrollment | Patients with available information | Chronic complications n (%) | Retinopathy n (%) | Neuropathy n (%) | Nephropathy n (%) |
|---|---|---|---|---|---|
| Overall | 901 | 108 (12) | 49 (5.4) | 57 (6.3) | 41 (4.6) |
| 0 < 10 years | 534 | 28 (5) | 8 (1) | 17 (3) | 8 (1) |
| 10 < 20 years | 251 | 42 (17) | 19 (8) | 23 (9) | 20 (8) |
| 20 < 30 years | 78 | 21 (27) | 12 (15) | 8 (10) | 6 (8) |
| ≥ 30 years | 38 | 17 (45) | 10 (26) | 9 (24) | 7 (18) |
p < 0.0001.
Table 3 Multivariate logistic regression analysis for T1D associated chronic complications
| Beta | SE | OR (95% CI) | p | |
|---|---|---|---|---|
| SMBG <4 times/day | 0.992 | 0.472 | 2.69 (1.11-7.18) | 0.036 |
| CGM use | 0.689 | 1.088 | 1.99 (0.19-16.98) | 0.526 |
| Time since diagnosis (≥10 years) | 1.029 | 0.3102 | 2.78 (1.53-5.21) | 0.020 |
| Private health-care setting | −0.057 | 0.509 | 0.94 (0.33-2.51) | 0.909 |
| Female | 0.874 | 0.385 | 2.39 (1.15-5.26) | 0.023 |
| Obesity (BMI ≥30 kg/m2) | 1.05 | 0.461 | 2.87 (1.13-7.04) | 0.022 |
| Insulin pump use | −0.535 | 0.616 | 0.58 (0.16-1.86) | 0.384 |
| HbA1c | 0.063 | 0.081 | 1.05 (0.89-1.23) | 0.438 |
| Hypoglycemia Event | 0.719 | 0.312 | 2.09 (1.13-3.92) | 0.021 |
SMBG: self-monitoring of blood glucose; CGM: continuous glucose monitoring; BIC: 255.2216; R2 = 0.8364463.
DISCUSSION
RENACED-DT1 is the first longitudinal online registry for T1D in Mexico, from different states of the country, and includes data from children and adults who are being followed at both public and private health-care settings. Enrollment of patients in the RENACED-DT1 registry is ongoing and open to all physicians in the country. In the 1st 3.5 years since its inception, a little over 1000 patients have been registered in RENACED-DT1. This figure illustrates the difficulty of gathering patient data for T1D in Mexico and the relevance of this initiative.
Our results are similar to those of the T1D Exchange Clinic Registry and SEARCH for Diabetes Youth Study, in which most of the participants do not reach the HbA1c targets recommended by the American Diabetes Association24. Furthermore, in concordance with other registries25-27 we found a high prevalence of patients with overweight (35.4%) and obesity (8.9%). The SEARCH for Diabetes in Youth Study found an obesity rate of 12.6% in PWT1D25, and the T1D Exchange Study found an obesity rate of 13.1% in adolescents26. The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research (DCCT-EDIC) found that obesity prevalence, in the intensive treatment arm, increased from 1% at baseline in the DCCT Study to 31% at 12-year follow-up of the EDIC Study27. Mexico has one of the highest prevalence of metabolic diseases worldwide, including mixed dyslipidemia, hypoalphalipoproteinemia, hypertriglyceridemia, and obesity28. The evolution of PWT1D in Mexico, who may have other metabolic diseases, deserves a closer surveillance.
In the bivariate analysis of our registry, as in other registries around the world, more frequent SMBG, insulin pump therapy and the use of CGM devices are associated with an improved metabolic control29-31. However, after adjustment for covariables, only SMBG ≥ 4 times/day remained an associated factor for good glycemic control as measured by HbA1c < 7%. Future studies will address whether the use of technology is associated with adequate metabolic control in our population. In several countries, especially in Europe, this knowledge has led to changes in clinical practices, which have improved metabolic control with decreased incidence of severe hypoglycemia, throughout the years32-34.
In Mexico, little is known about T1D, especially about the long-term follow-up and complications of people living with the disease6,35. As expected, in our cohort, longer diabetes duration was associated with an increased presence of chronic complications. In addition, female sex, lower SMBG, hypoglycemia, and obesity were also associated variables. It is possible that hypoglycemia is associated with chronic diabetes complications, as it is associated with higher glycemic variability. The prospective and longer follow-up of the patients in our registry will aid to confirm the current findings.
We found a female predominance (61%) in our registered patients, in contrast to what occurs in other registries that report no gender difference. This finding needs to be tracked further as the number of patients registered increases to ascertain whether or not Mexican PWT1Ds are more frequently female, or if this is linked to a selection bias, related to women being more willing to participate.
In our country, government coverage for PWT1D is limited, leading to considerable out-of-pocket expenses. PWT1D require careful medical care36,37. It would be desirable to have universal access to therapy (insulin analogues and glucose monitoring) and up-dated diabetes education for all PWT1D during their lifetime, to minimize complications and increase quality of life.
Some limitations of our work should be acknowledged. This is not a population-based study, which limits the extrapolation of the data to all PWT1D in Mexico. If we consider the prevalence of 26,578 cases reported by the IDF in 201938, and the 25,695 cases notified in the period between 2010 and 2018 by the Mexican Ministry of Health39, our sample population is a small proportion (approximately 6%) of the diagnosed cases with T1D in Mexico. Our results are similar in gender and age distribution to those reported by the Mexican Ministry of Health in 201940. In this analysis, there is limited representation of the public sector and there are missing data, as it occurs in all registries.
This work represents a description of the data obtained from the online T1D registry in Mexico RENACED-DT1. Increased SMBG is associated with better metabolic control and lower presence of diabetes complications. The percentage of patients achieving HbA1c < 7% must be expanded to reduce the incidence of chronic complications and improve the quality of life of those living with the disease.











 nueva página del texto (beta)
nueva página del texto (beta)


