INTRODUCTION
The widespread use of face masks is becoming a standard practice in some countries with the emergence of coronavirus disease 19 (COVID-19) pandemic. However, disagreements between health authorities on their policy have led to controversy within the medical community. Some recommendations are being made despite the lack of high quality of evidence to support the use of face masks as a preventive measure during this pandemic. A general outlook of recent research in this matter and areas of opportunity are discussed in this review.
TYPES OF FACE MASKS AND REGULATIONS
The types of masks currently available vary depending on the material, design, and purpose for which they are made1. To be used in professional or health-care settings, safety and health standards need to be fulfilled and these are regulated by specific agencies. In the United States and many parts of America by the Food and Drug Administration (FDA), the National Institute for Occupational Safety and Health (NIOSH), and the Occupational Safety and Health Administration (OSHA).
The terms face mask, medical mask, and surgical mask are often used interchangeably, but under standardized definitions, a face mask is not under industry regulation. Another difference to be considered is the one between a mask and a respirator, which is the ability of the latter to provide a reliable level of protection from large and small airborne particles. This varies depending on the filtration capability and is designated with a number, meaning that a N95 respirator filters at least 95% of airborne particles. Despite this difference, both the medical/surgical mask and the N95 respirator are tested for fluid resistance, filtration efficiency, flammability, and biocompatibility under the NIOSH and FDA regulations2. For the official definitions and regulations, Tables S1 and S2 in the Supplementary Appendix.
Table S1 Definitions of the different types of face coverings
| Definition | |
|---|---|
| Face mask | Loose fitting, disposable device, with or without a face shield that creates a physical barrier between the mouth and the nose of the wearer and potential contaminants in the environment. Not considered a respiratory protection. |
| Face shield | A device used to protect the user’s eyes and face from bodily fluids liquid splashes or potentially infectious materials. |
| Surgical or medical mask | Loose fitting, disposable type of face mask. Fluid resistant, flammable, and provide protection from splashes, sprays and splatter. Can be labeled as dental or medical masks. Not considered a respiratory protection. |
| N95 filter | A type of NIOSH-approved filter or filter material, which captures at least 95% of airborne particles and is not resistant to oil (N). |
| N95 respirator | A generally used term for a half-mask air-purifying respirator with NIOSH-approved filter or filter material. |
| Personal protective equipment (PPE) | Specialized clothing or equipment worn by employee or health-care personnel to protect the respiratory tract, mucous membranes, skin, and clothing from infectious agents or other hazards. |
Definitions from the Food and Drug Administration (FDA) and the National Institute for Occupational Safety and Health (NIOSH)2.
Table S2 Characteristics of the face mask, medical mask, and N95 respirator
| Face mask | Medical mask | N95 respirator | |
|---|---|---|---|
| Material characteristics | Unspecified | – Fluid resistant – Biocompatible |
– Fluid resistant – Biocompatible |
| Flammability* | Not regulated | Class I or II | Class I |
| Filtration efficiency | Not regulated | Not reliable, up to 85% of airborne particles | 95% of airborne particles |
| Face seal | Loose | Loose | Tight |
| Intended use or indications | Blockage of large particles | Health care and patient fluids protection | Health-care respiratory protection |
| Limitations | – Single use – Unreliable protection |
– Single use – Leakage |
– Single use**
– Appropriate wear |
| Testing and approval regulations | Not regulated | FDA 21 CFR 878.4040 | NIOSH 42 CFR 84 |
| Fit testing requirement | No | No | Yes OSHA standards |
Adapted from the National Institute for Occupational Safety and Health (NIOSH)2.
FDA: Food and Drug Administration; OSHA: Occupational Safety and Health Administration.
*Flammability classes are Class I or normal (average burn time > 7 s); Class II or intermediate (0-7 s); and Class III or rapid (< 7 s) according to 16 CFR 1610 standards.
**Unless specified by the manufacturer as single use only, the NIOSH establishes a possible extended use of 8 h.
With the emergence of novel respiratory pathogens, much research has been done to explore the efficacy of face masks in filtering respiratory viruses or reducing their transmission and to be used for protection or prevention, respectively. Most of the studies have been done on influenza outbreaks and it has been concluded through systematic reviews and meta-analysis that there is limited evidence to support the use of masks in health care or community settings as prevention methods due to the heterogeneity of the studies and inconsistent methodology3. Nevertheless, this research has provided knowledge about the mode of transmission and led to the implementation of coordinated preventive measures, such as hand hygiene and social distancing.
MECHANISMS OF VIRUS TRANSMISSION
A comparison of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) with three emergent respiratory viruses, two coronaviruses (CoV) and influenza virus, is summarized in table 1. The data were collected from latest WHO and Center for Disease Control and Prevention (CDC) reports5-8 and from reviews9-11.
Table 1 Comparison between emergent respiratory viruses
| H1N1 (2009) | MERS-CoV (2012) | SARS-CoV1 (2002) | SARS-CoV2 (2019) | |
|---|---|---|---|---|
| Disease | Influenza A | Middle East respiratory syndrome (MERS) | Severe acute respiratory syndrome (SARS) | Coronavirus disease (COVID-19) |
| Confirmed cases | 100.5 million | 2494 | 8096 | 2,471,136* |
| Human-to-human transmission (of relevance) | Droplets > Aerosols Contact Airborne | Contact droplets > Aerosols Airborne | Aerosols > Droplets Indirect Contact Airborne | Aerosols > Droplets Indirect Contact** Airborne** |
| Incubation period (days) | 1-4 | 4.5-5.2 | 3.6-4.4 | 2-15 |
| Reproductive number | 1.2-1.6 | < 1 | 2-5 | 1.4-5.5*** |
| Case fatality rate | 2% | 34.4% | 9.6% | 0.9-2.1%*** |
Droplets: > 5 μm; aerosols: < 5 μm.
*As of April 22, 2020.
**The importance is controversial, discussion on text.
***Estimates vary and depend on the number of confirmed cases; fatality rate is based on last estimates in Wuhan, China 11.
The most accepted and studied human-to-human transmission mechanisms of respiratory viruses are the droplet, airborne, and contact transmission (direct and indirect) routes9. Wells introduced the concept of emissions and proposed two categories: large and small droplets, based on the size and evaporation times12. To date, droplets below a diameter of 5 µm (micrometers) are known as aerosols or droplet nuclei, and those larger than 5 µm are called spray droplets or simply droplets; although diameter values vary along the literature, the 5 µm cutoff is currently recommended according to the WHO guidelines13. This classification system continues to be the reference for risk management, recommendations, and allocation of resources.
New experimental models of respiratory emissions have proposed that the rapid spread of SARS-CoV-2 might not be efficiently prevented following this droplet transmission pattern, suggesting that the present recommendations may underestimate the exposure range14. These models propose that the trajectory of sneezes and coughs is multiphase, creating a turbulent cloud of respiratory emissions rather than a formation of droplets before ejection and that speaking also contributes to the release of numerous particles with a mean diameter of 1 µm and interperson variability15,16.
The contact and airborne transmission routes appear to be viable for SARS-CoV-2 based on a recent experiment done by van Doremalen et al. They compared the stability between SARS-CoV-1 and SARS-CoV-2 in five environmental media: aerosols, plastic, stainless steel, copper, and cardboard and found similar half-lives between the viruses in all conditions with exception of stainless steel and plastic, where SARS-CoV-2 had longer stability. These findings suggest that the epidemiological differences between these viruses might be due to other virulence factors17.
A series of investigations are trying to understand the high virulence of SARS-CoV-2 given the concern of the potential high transmissibility from asymptomatic patients. This began with reports of patients who had presumably acquired the disease during the incubation period18,19. A case series from two family clusters20 found that the viral load of SARS-CoV-2 on nasal and throat swabs was similar between asymptomatic patients and symptomatic patients. Findings from Woelfel et al.21 suggest an active replication of SARS-CoV-2 in the nasopharynx, which might explain the positive tests in the prodromal stage and the risk of asymptomatic transmission.
All of these elements are important to be taken into account to understand that limiting the transmission of a virus, with the current concern on SARS-CoV-2, in both health care and community settings, requires a coordinated approach. In the same way, when evaluating the outcomes of preventive measures, it becomes challenging to measure individual contributions.
UNIVERSAL MASKING: DEFINITION, CONTROVERSIES, AND EVIDENCE
There is not an official definition of the term universal masking but rather a recent and growing use on behalf of the general and medical community in reference to a widespread use of masks with the intention of preventing community transmission of COVID-1922. This has led to appeal health authorities to make decisions on the matter.
The latest WHO statement on the use of masks from April23 expresses that “there is no evidence that wearing a mask (whether medical or other types) by healthy persons in the wider community setting can prevent infection from COVID-19” and does not make recommendations for or against their use. However, it is specified that if local policy-makers consider otherwise, they should define the purpose of use, risk of exposure, vulnerability of the user, setting, suitability, and type of mask to make a “risk-based approach.”
Feng et al. compared the recommendations from different countries and found that while there is an agreement on reserving medical masks for health-care personnel and symptomatic patients, discrepancies arise in community settings24. In China, South Korea, Japan, Hong Kong, Singapore, and Czech Republic, the widespread use of masks has been implemented. In some countries like China, it was enforced by the authorities and the type of mask recommended is based on risk stratification while others, such as Hong Kong and Taiwan, have reached this by “social advocacy.” Health authorities in countries such as the UK and Germany have abstained from making recommendations in the absence of evidence. Something similar has happened in Mexico where the federal health ministry has not made official recommendations attending the use of cloth masks25. The CDC, on the other hand, updated their advice on April 4 and now recommends that people should wear homemade cloth masks in public areas and released instructions on how to make and wear them26.
This discrepancy between health authorities and the lack of evidence has raised discussion within the medical community. Some authors propose the use of indirect evidence (inferred evidence from primary studies) to support the use of face masks until better evidence becomes available27. Nevertheless, clinical decisions based on indirectness require a complex analysis of prospectively collected data28. To complicate matters further, the problem is being addressed based on different populations (medical workers and community), interventions (medical masks and cloth masks), and outcomes (protection and source control). Therefore, a consensus becomes challenging when the clinical question is inconsistent.
In terms of protection, as mentioned earlier, much of the research has been done on influenza, and currently, there are no studies on SARS-CoV-2. A recent systematic review29 on the efficacy between medical masks and N95 respirators in preventing viral infection, including CoV, found no increase of laboratory confirmed infections (odds ratio [OR] 1.06; 95% confidence interval [CI] 0.90-1.25) or clinical respiratory illness (OR 1.49; 95% CI 0.98-2.28) with the use of medical mask compared to N95. However, none of the trials identified SARS-CoV-2 and the authors graded the overall studies as very low to low quality of evidence (GRADE).
When focusing on source control, which is the arising concern given the asymptomatic transmission of SARS-CoV-2, there are no randomized controlled trials evaluating the effectiveness of face masks on reducing the transmission of SARS-CoV-2 in neither health care nor community settings, but meta-analysis and systematic reviews have been conducted trying to answer this question.
Two systematic reviews30,31 did not find strong evidence to support the use of masks within the community as a protective measure during this pandemic; however, they are quick reviews and one of them has not been peer-reviewed30, which lowers their quality. An update32 to a previously conducted systematic review on physical barriers as prevention measures done by Jefferson et al. in 201133 found that the use of masks alone versus no masks (9 trials in health care workers and 7 in community) shows no significant reductions in influenza-like illness or in confirmed influenza infections, 7% (relative risk [RR] 0.93 CI 95% 0.83-1.05) and 16% (RR 0.84 CI 95% 0.61-1.17), respectively. They recommended the use of masks combined with other measures (social distancing), grading the studies on “variable quality of evidence.” The 2011 review was the basis for the respiratory hygiene recommendations (use of medical masks and handwashing during respiratory infections) in the current WHO guidelines34 (very low quality of evidence [GRADE], strong consensus recommendation); however, the update has not been peer-reviewed to guide clinical practice35.
A recent trial on virus shedding in exhaled breath showed promising implications for this matter36. Leung et al. studied 111 patients with confirmed respiratory viral infection (seasonal coronavirus, influenza, and rhinovirus) and compared the viral load in respiratory droplets and aerosol samples with and without the use of a surgical mask. They found significant reductions in the detection of the CoV in both droplets (30%-0%, p = 0.09) and aerosols (40%-0%, p = 0.04). However, since no SARS-CoV-2 was identified, the applicability of this study is uncertain.
So far, there is no high quality of evidence to demonstrate the effectiveness of medical masks in the community during this pandemic, neither as source control nor as protection. Some authors have pointed out that implementing the use of medical masks in the community would lead to shortage of personal protective equipment for the health-care personnel. This challenge is already happening in many countries. Therefore, focusing on the use of cloth masks appears to be more sustainable37. However, the same limitations arise since the effectiveness of cloth masks in community settings has not been tested. In health-care settings, a randomized trial38 showed that the use of cloth mask compared to medical masks had significantly higher rates of influenza-like illness (RR 13.25; 95% CI 1.74-100.97) and did not recommend its use. The authors discussed that moisture retention and reuse of the cloth masks may have contributed to those findings.
Some important aspects to be considered before encouraging the use of homemade cloth masks are outlined in an expert consultation review39. Two main elements would determine the potential effectiveness of a cloth mask: the mask itself and the wearer. Consequently, for a mask to adequately fulfill its function, other variables intervene such as the type of fabric (woven or knitted), material (e.g., cotton or polyester), number of layers, and design. These variables will define its filtration efficacy (blockage of particles), leakage, and differential pressure (how much they difficult breathing) in a wide variation.
The filtration efficiency on various types of cloth masks has been tested using different size particles with ranges varying from 39% to 65% under laboratory conditions40 and 48% to 83% using different household materials41. A recent study42 aimed to evaluate the effectiveness of two-layered cotton masks compared to three-layered polypropylene surgical masks in filtering SARS-CoV-2 and found that both were ineffective in filtering the virus during coughs. However, this was a small study, which only included four symptomatic patients.
The role of the wearer is important since it determines how well and often they use the mask, the amount of moisture produced, and the breathing difficulty; where the last two are interrelated and depend on the type of fabric and differential pressure, respectively. Evidence from the past pandemics could indirectly estimate wearer’s role, in which observations from the H1N1 pandemic found < 50% of mask adherence43. In addition, MacIntyre and Chughtai observed other determinants of compliance such as level of discomfort and reduced risk perception from SARS and influenza pandemics44.
Given the uncertainties of the filtering efficiency and the level of adherence during this pandemic, Howard et al.45 proposed an estimation of the impact of wearing masks on the reproductive number (R0). They used a model46 based on possibilities of a full range efficacy and a full range mask adherence at an estimated R0 of 2.4 and suggest that on a 50% efficacy and 50% adherence, the R0 could go down to 1.35, arguing that such reduction would be comparable to seasonal influenza (R0 ≈ 1.28). However, even if SARS-CoV-2 could resemble the transmission dynamics of influenza, the estimates of the R0 can vary depending on several factors, such as the population studied, other public health interventions, and surveillance intensity47.
To put if briefly, encouraging the use of masks, whether medical or cloth masks, without standardized instructions and adequate teaching, would result in a wide range of efficacy profiles with potential disadvantages that could outweigh the advantages in an uncertain degree (Fig. 1).
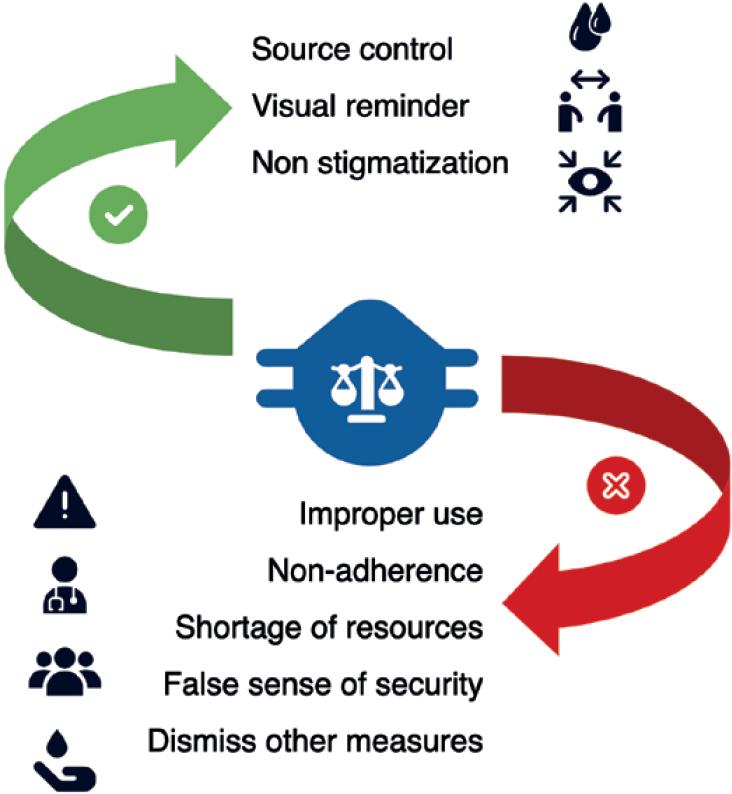
Figure 1 Potential advantages and disadvantages on the use of face masks. Reproduced with permission from SlidesCarnival (https://www.slidescarnival.com).
CONCLUSIONS
Future investigations on the use of face masks within the community and their effectiveness, as well as cost-effectiveness studies, are needed to provide high quality of evidence to address these uncertainties and guide decisions. Randomized controlled studies performed at community levels are required to plan future public policies. The study samples should be stratified according to their risk profile (elders, health workers, inmates, etc.) and predefined outcomes should be prospectively assessed. The main challenge will be to capture the majority of the clinically relevant outcomes with enough precision.











 nueva página del texto (beta)
nueva página del texto (beta)


