INTRODUCTION
Clinical situations in intensive care units (ICUs) change rapidly, and many factors, such as comorbidities and disease progression, may prolong the length of stay (LOS). Multiple assessment scores facilitate re-evaluation and risk stratification of patients; however, performing these assessments is time consuming, and high workload of manually entering data can cause an episode to be missed. To err is human; thus, using a supporting system to prevent errors is crucial. Moreover, because too many alarms may result in alarm fatigue, we use an early-warning score to generate effective alarms for indicating deterioration1.
Much relevant clinical data such as the Sequential Organ Failure Assessment (SOFA) score can be translated directly from electronic medical records (EMRs) and automatically calculated and uploaded every 48 h. The SOFA score consists of several physical parameters that include oxygenation, conscious level, and clinical laboratory data such as platelet count and renal function, which is widely used to estimate mortality rates and disease progression (i.e., if the score increases by 2 points every 48 h)2. Artificial intelligence is a promising and developing technology that can assist in the extensive execution of various tasks. Therefore, in this study, we implemented an informatics system combined with an automatic reminder using the SOFA score and care bundle for the daily care of ICU patients to reduce their LOS and improve the quality of care.
METHODS
This is a prospective cross-sectional study conducted in a teaching hospital with 52 ICU beds, and the study period was 12 months (6 months of traditional ICU and 6 months after technology electronic dashboard-ICU [TED-ICU] implementation) (Fig. 1). Basic data were collected from adult patients who were admitted to ICUs, a 10-bed emergency department ICU, an 18-bed surgical ICU, and a 24-bed medical ICU, during the study period. One intensivist and one board-certified physician were responsible for providing care to 12 beds in the ICU during the day and night, respectively. The nurse-to-patient ratio in all the three ICUs was 1:1 or 1:2, depending on the conditions and nursing demands of each patient.
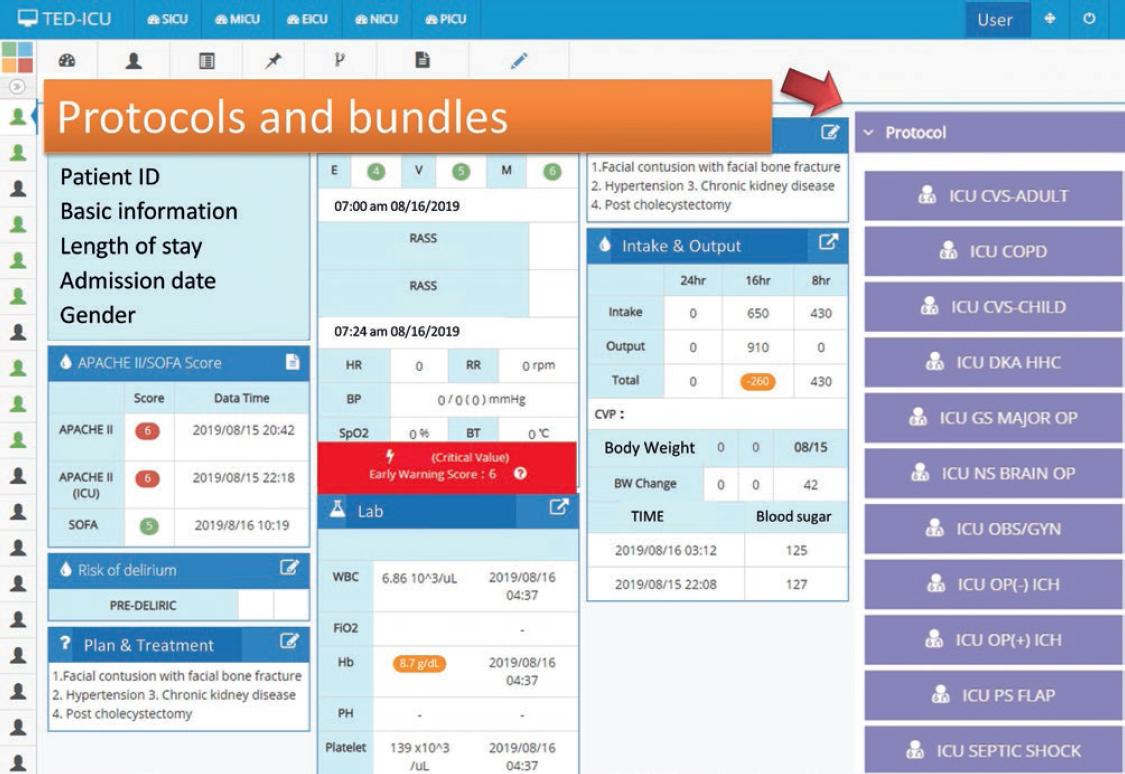
Two types of clinical scores were recorded for every ICU patient using the Acute Physiology and Chronic Health Evaluation (APACHE) II scale on admission, and the SOFA score was automatically retrieved from EMR every 48 h. Points were assigned during each shift for abnormal vital signs, laboratory values, and other clinical factors and procedures, such as recent cardiopulmonary resuscitation, neurological status, mechanical ventilation, and chronic dialysis. Since February 2017, TED-ICU has been implemented in our ICU with automatic uploading of physiological information and a care bundle alarm to provide real-time information to the care team. Ventilator-associated pneumonia bundle and urinary tract infection bundle were also incorporated with our TED-ICU. The SOFA score was automatically calculated every 48 h. If the SOFA score decreased by more than 2 points, the system automatically provided a reminder to the clinical staff to re-evaluate the current condition and determine whether it was suitable to transfer the patient to the general ward. We prospectively collected data from ICUs before and after the implementation of TED-ICU. Basic information, time points of intervention and LOS of the patients who were admitted to our ICUs between July 2016 and July 2017 were collected. Analysis of covariance was used to determine the difference in LOS between traditional ICU systems and TED-ICU, and the covariance for the ANCOVA was age, SOFA score (on the day of transferring to the general ward), and APACHE-II scores. Logistic regression was used to evaluate the effect of potential factors on the in-hospital mortality rate. Patients’ outcome and LOS were also recorded. An assigned observer regularly recorded the response time of each ICU alarm event and measured the care handover durations before and after TED-ICU implementation. The related expenses of each patient were also retrieved through informatics systems. Statistical differences between the TED-ICU and traditional ICU for age and SOFA score were determined using Student’s t-test, and the Chi-square test was used to compare gender and APACHE-II between the two groups. The APACHE-II score is a critical index of a patient’s condition, and our study explored the effect and safety of TED-ICU on outcomes in ICU patients after stratifying them according to risk, namely, a high-risk population (APACHE-II scores of > 24) and moderate-risk population (APACHE-II scores of ≤ 24), according to a previous study2. We used common cutoff point (p < 0.05) for statistical significance. The study was approved by the IRB committee (TMU-JIRB No. 201802064), and the committee waived the requirement of informed consent.
RESULTS
A total of 2248 patients were admitted to our ICUs during the study period (1147 in a traditional ICU system [traditional cohort] and 1101 patients after TED-ICU implementation [TED-ICU cohorts]). The number of male patients was non-significantly higher in both groups (59.9% and 57.0%), and most patients were older than 65 years in both cohorts. The APACHE-II score at ICU admission was 11 (6-17) in the traditional cohort and 10 (6-17) in the TED-ICU cohort. Patients in TED-ICU were older than those in the traditional ICU (mean difference [MD] = 1.73; 95% confidence interval [CI]: 0.30, 3.15). The SOFA score for the day when patients were transferred to the general ward was approximately 7 in both the traditional cohort3-11 and the TED-ICU cohort3-12. Patients in TED-ICU had higher SOFA score than those in the traditional ICU (MD = 0.66; 95% CI: 0.11, 1.21) (Table 1).
Table 1 Characteristics (n = 2248)
| Characteristic | Total (%) | Traditional (%) | TED-ICU (%) | Statistical test | p |
|---|---|---|---|---|---|
| Gendera | 2.01c | 0.156 | |||
| Male | 1314 (58.5) | 687 (59.9) | 627 (57.0) | ||
| Female | 934 (41.5) | 460 (40.1) | 474 (43.0) | ||
| Ageb | 68 (56-81) | 68 (56-81) | 69 (57-82) | 1.73d | 0.017 |
| SOFAb | 7 (5-14) | 7 (5-13) | 7 (5-14) | 0.66d | 0.020 |
| APACHE-IIb | 11 (6-17) | 11 (6-17) | 10 (6-17) | 0.17c | 0.681 |
| ≤24a | 2067 (91.9) | 1052 (91.7) | 1015 (92.2) | ||
| >24a | 181 (8.1) | 95 (8.3) | 86 (7.8) |
aNumbers with percentage,
bMedian with interquartile range,
cChi-square, dMean difference. APACHE-II: Acute Physiology and Chronic Health Evaluation II, SOFA: sequential organ failure assessment.
Overall, patients in the TED-ICU cohort (mean days = 5.53) had shorter LOS than those in the traditional ICU cohort (mean days = 7.26), and the difference in LOS was statistically significant after covariances (age, SOFA score, and APACHE-II score) were statistically controlled (F = 30.2). The adjusted MD for LOS was −1.78 days. In the subgroup of patients with APACHE-II scores of ≤ 24, the patients in the TED-ICU cohort (n = 1015, and mean days = 5.52) had significantly shorter LOS than those in the traditional cohort (n = 1052, and mean days = 7.11), and the adjusted MD in LOS was −1.67 days, which was statistically significant (F = 25.97). Implementing TED-ICU exerted a greater effect on LOS in the subgroup of patients with APACHE-II scores of > 24 than that in the subgroup of patients with APACHE-II scores of ≤ 24. In the subgroup of patients with APACHE-II scores of > 24, the TED-ICU cohort (n = 86, and mean days = 5.70) exhibited shorter LOS than in the traditional cohort (n = 95, and mean days = 8.89), and the adjusted MD in LOS was −3.04 days, which was statistically significant (F = 25.97) (Table 2).
Table 2 Difference in LOS between the TED-ICU and traditional cohorts
| Length of ICU stay | TED-ICU | Traditional | Adj. | 95% CI | |||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | n | M | SD | n | MDa | Lower | Upper | |
| Overalla | 5.53 | 4.99 | 1101 | 7.26 | 9.57 | 1147 | −1.78** | −2.42 | −1.15 |
| APACHE-II scoreb | |||||||||
| ≤24 | 5.52 | 4.94 | 1015 | 7.11 | 9.24 | 1052 | −1.67** | −2.31 | −1.03 |
| >24 | 5.70 | 5.43 | 86 | 8.89 | 12.63 | 95 | −3.04* | −5.99 | −0.10 |
ANCOVA.
*p < 0.05;
**p < 0.001. APACHE-II: Acute Physiology and Chronic Health Evaluation II, CI: confidence interval, LOS: length of stay, M: mean, MD: mean difference, SD: standard deviation.
aCovariances: age, Sequential Organ Failure Assessment score, APACHE-II score.
bStratified by APACHE-II score, Mild to moderate: ≤ 24, Severe: > 24, Covariances: age, Sequential Organ Failure Assessment score, TED-ICU: technology electronic dashboard-intensive care units.
Furthermore, we examined mortality rates for determining the safety of the TED-ICU using multivariate logistic regression analysis. Overall, some significant factors were identified, but the TED-ICU did not show significant predictive power for mortality. By contrast, age (odd ratio [OR] = 1.019, p < 0.001), SOFA score (OR = 1.050, p < 0.001), and APACHE-II score (OR = 1.080, p < 0.001) showed a significant predictive power for mortality. Similar findings were also observed in the subgroup of patients with APACHE-II scores of ≤ 24. In this subgroup, we found that age (OR = 1.025, p < 0.001) and SOFA score (OR = 1.087, p < 0.001) significantly predicted mortality, but implementing TED-ICU did not affect mortality (OR = 0.911, p = 0.387). In the subgroup of patients with APACHE-II scores of > 24, no potential factor was significantly predictive for mortality (Table 3).
Table 3 Logistic regression of the TED-ICU on in-hospital mortality
| Independent | 95% CI | |||
|---|---|---|---|---|
| Variable | B | OR | Lower | Upper |
| Overall | ||||
| Age | 0.019 | 1.019 | 1.012 | 1.026 |
| SOFA score | 0.048 | 1.050 | 1.030 | 1.069 |
| APACHE-II score | 0.077 | 1.080 | 1.063 | 1.097 |
| TED-ICU | −0.019 | 0.981 | 0.801 | 1.201 |
| APACHE-II ≤ 24 | ||||
| Age | 0.024 | 1.025 | 1.017 | 1.032 |
| SOFA score | 0.084 | 1.087 | 1.068 | 1.107 |
| TED-ICU | −0.093 | |||
| 0.911 | 0.739 | 1.125 | ||
| APACHE-II > 24 | ||||
| Age | 0.012 | 1.012 | 0.987 | 1.037 |
| SOFA score | 0.006 | 1.006 | 0.957 | 1.058 |
| TED-ICU | 0.241 | 1.272 | 0.652 | 2.483 |
APACHE-II: Acute Physiology and Chronic Health Evaluation II, CI: confidence interval, SE: standard error, SOFA: Sequential Organ Failure Assessment, TED-ICU: technology electronic dashboard-intensive care units.
Several additional effects were observed after implementing TED-ICU. First, 1121 work hours per month could be saved by simplifying the workflow through automatic uploads. Second, the response time to the alarm for abnormal laboratory and physiological information of a patient decreased by 0.6 min/episode (8.6-8 min). Third, the actual cost of taking paper printouts decreased to USD 600/year.
DISCUSSION
Patients admitted to ICUs receive high-intensity treatment and require high-quality care; numerous types of monitors are present in ICUs, including those for indicating vital signs and physiological parameters. Diverse clinical data are generated, resulting in large amounts of information for ICU team members1. Pre-set thresholds for warning activation result in frequent alarms because of changes in clinical conditions; however, most of these alarms are false. Clifford et al. reported that a high frequency of false alarms causes considerable stress to ICU team members, which results in low-quality care1. A highly stressful work environment is unfavorable for both patients and clinicians. Fatigue caused by false alarms can lead to the ignorance of true alarms and delayed response time.
To reduce fatigue caused by false alarms and work burden on the ICU staff and to achieve a more-effective clinical situation, TED-ICU, an informatics system, was introduced at our hospital for clinical care. TED-ICU incorporates an interface between all bedside devices, including the ventilator settings, physiological monitors, and laboratory results and image findings, and the hospital’s EMR. Consequently, all parameters and laboratory, biological, and radiological findings, such as SOFA, APACHE-II, and early-warning scores, are automatically uploaded, calculated, and integrated into the database by TED-ICU; moreover, a pre-set alarm is activated to provide real-time information to the care team.
Several scoring systems are used for predicting prognosis and for risk stratification in ICUs. The APACHE-II and SOFA scores have been commonly used in ICUs to evaluate the severity of patients’ conditions, and studies have examined its effectiveness13. The SOFA score consists of respiration condition (FiO2 and PaO2), coagulation (platelet count), liver function (bilirubin level), neurological condition (Glasgow coma score), cardiovascular condition (mean arterial pressure and need of vasopressor), and renal function (creatinine level and urine output). Ferreira et al. indicated that sequential SOFA scores are reliable indicators of prognosis; their results revealed that an increase in the SOFA score in the first 48 h in an ICU predicted mortality in approximately 50% of patients2. Raith et al. concluded that an increase in SOFA scores by two or more points showed higher prognostic accuracy for in-hospital mortality than did the systemic inflammatory response syndrome criteria or the qSOFA score14. A recent study showed that SOFA scores calculated automatically from EMRs showed a high correlation with SOFA scores calculated manually, and a similar predictive value was also observed for 30-day in-hospital mortality3. A previous study demonstrated that the SOFA score at ICU discharge predicted post-ICU mortality4. Another prospective cohort analysis demonstrated that absolute risk reductions in 28-day mortality after ICU transfer correlated to SOFA score decrement5. Therefore, using the SOFA scoring system as an indicator for clinical practice and decision-making is reasonable. The auto-calculation combined with reminder function of our TED-ICU guides ICU physicians for evaluating whether to transfer patients to general ward. Although the final decision for transfer after integrating all the information of the patient is still dependent on on-duty ICU physicians, unnecessary stasis in ICU can be avoided and further medical resources expenses can be reduced. Our results showed that LOS significantly decreased after automatic reminders were generated for patients who exhibited a decrease of 2 points in the SOFA score. High SOFA scores indicate longer stay for patients in ICUs. LOS decreased after the introduction of electronic-ICU (e-ICU). Levesque et al. reported similar positive changes after the implementation of an intensive care information system (ICIS) in their medical and surgical ICUs. A significant decrease in LOS in the ICU was observed without changing both the ICU staff and policies during the study period6.
TED-ICU is one type of ICIS, and the use of the ICIS has been increasing since a decade, and several studies have reported numerous advantages of the ICIS. The ICIS shortened the time of medical coding, reduced errors, and positively affected ICU budget distribution7. In addition, information systems assist with nursing activities8, thus leading to shorter latency for urgent examination9, resulting in improved multidisciplinary communication among clinicians10, and reducing mortality and ventilation rates in critically ill patients11. Our experience revealed some additional advantages. First, we saved 11,200 h/year for physician and nurses’ care handovers and 1121 work hours per month by obtaining accurate vital sign inputs through the automatic uploads instead of manual intervention. Second, we achieved a shorter response time to the warning alarms of a patient with an average of 8 min/episode (an average decrease of 0.6 min) and 76.9% decrement in unexpected extubation (26-6 cases). Third, we saved USD 277,425 within 6 months on expenses related to medical services after TED-ICU (average USD 252/case) by reducing the LOS, and we established a more environmentally friendly model by reducing the number of actual paper printouts (USD 600/year). However, the cost of implementing the ICIS poses a challenge for hospitals. Two European studies have reported that one of the major concerns regarding the introduction of the ICIS is the initial cost and the additional cost for its further maintenance12,15. The cost of implementing e-ICU was USD 122,000, which was divided as USD 117,000 and USD 5000 for hardware and software, respectively.
This study has several limitations. First, the study was conducted for only 1 year, in which the first half and second half of the year were used to assess outcomes before and after setting up TED-ICU, respectively. Second, because the assessment was only for ½-year periods, several factors, such as seasonal changes and local epidemics, could have influenced the results. Some ICU patients were do-not-resuscitate patients who agreed to receive aggressive treatment, except for cardiopulmonary resuscitation, endotracheal intubation, and external defibrillation. The in-hospital mortality rate defined as mortality occurred during the entire hospital stay instead of during the ICU stay. Thus, policy, assessment, and treatment during the general ward period without the implementation of an informative system might have exerted an effect on the mortality rate. Because of the limitation of information setting in our hospital, we encountered difficulties in distinguishing the overall true ICU cost for each patient from the overall cost during the total hospital stay.











 nueva página del texto (beta)
nueva página del texto (beta)