INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is characterized by nonreversible airflow obstruction, of which emphysema and chronic bronchitis are the most common form1. COPD is a systemic disease that affects lung function and is accompanied by extra-pulmonary comorbidities. Age-related osteoporosis (OP) is a major public health problem which represents an enormous burden of disability and has been recognized as one of the important comorbidities in COPD2. A retrospective study conducted in the US identified COPD as the leading cause of secondary OP, independently of previously known risk factors such as glucocorticoid (GC) use or hypogonadism3. Meanwhile, OP has been proved to be associated with deterioration of lung function, poor quality of life, and excess mortality in COPD patients4. Indeed, the two conditions form a vicious cycle that significantly worsens prognosis.
Recently, increasing evidence supports the correlation between COPD and OP5. These disorders share some risk factors, such as menopause, a low body mass index (BMI), GC therapy, smoking, physical disability, Vitamin D deficiency, and hypogonadism4,5. Menopause appears to be a particularly important risk factor for OP. Unlike younger women, the risk of OP in older women exceeds that of men, coinciding with the decline in estrogen production that marks the end of the protective effect of endogenous estrogens against bone mass loss6. An epidemiological survey showed COPD is the third-leading cause of death in the US, with greater mortality in women than in men7. Management of OP is clinically important in postmenopausal patients with COPD, as they are especially susceptible to decreased quality of life, prolonged times of hospitalization, and higher mortality4.
Several studies have clearly indicated OP to be associated with COPD in male patients; however, to date, few studies have examined the relationship between bone mass density (BMD) and COPD in postmenopausal women, remaining a matter of debate2,8. The aim of this cross-sectional study was to examine the association between BMD and COPD in postmenopausal women in Northwest China.
METHODS
Study population
This cross-sectional study included 133 COPD patients, and 31 age-matched female control subjects free from respiratory symptoms admitted to the Department of Geriatrics, Peoples Hospital of Xinjiang Uygur Autonomous Region, Urumqi, China, from January 1 2014 to August 31 2017. This unit mainly admits elderly patients with cardiovascular diseases and chronic respiratory diseases. The inclusion criteria were: postmenopausal women; age ≥50 years; non-smokers; and not taking medication known to affect bone turnover. The exclusion criteria were: presence of disorders that could influence bone and calcium metabolism, such as thyrotoxicosis, hyperparathyroidism, chronic renal failure, malignancies, and current treatment with oral or inhaled GC.
Clinical features and laboratory examination
Eligible subjects had their weight and height measured, and their BMI calculated as body weight/height2 (kg/m2). Completion of the medical record was based on a standard questionnaire. Subjects who had been living or working with smokers were considered to be exposed to second-hand smoke.
Pulmonary function tests
The degree of airway obstruction was assessed using prebronchodilator spirometry measurements performed according to the standards of the American Thoracic Society9. In COPD patients, the degree of airway obstruction was categorized as follows: (a) mild (forced expiratory volume in 1 second [FEV1]/forced vital capacity [FVC] <0.7, and FEV1≥80% of predicted FEV1), (b) moderate (FEV1/FVC <0.7, and FEV1≥50, and <80% of predicted FEV1), (c) severe (FEV1/FVC <0.7, and FEV1≥30m and <50% of predicted FEV1), and (d) very severe (FEV1/FVC <0.7 and FEV1 <30% of predicted FEV1).
Measurement of bone mass density
Participants were required to have had BMD of left femoral neck bone densitometry measured using a dual X-ray absorptiometry with QDR 4500A fan beam bone densitometer (Bedford, MA, USA) according to the manufacturers instructions. BMD results were reported as T-scores. T-scores were also categorized into three groups according to the World Health Organization criteria for diagnosing OP: normal BMD (T ≥ −1 SD), osteopenia (T < −1SD and > −2.5 SD), and OP (T ≤ −2.5 SD).
Statistical analyses
Analyses were carried out using SPSS version 19.0 software (SPSS Inc., Chicago, IL). Since most continuous variables were normally distributed, as tested by the KolmogorovSmirnov test, they were expressed as mean ± standard deviation (SD). Differences between the groups were evaluated using the unpaired t-test. Categorical variables were compared with the Chi-square test. The four airway obstruction categories in COPD patients were reorganized into three groups (Mild, Moderate, and Severe, or very severe), to improve the statistical reliability of the estimates. To confirm the influence of COPD and airway obstruction category on the T-score, multivariate linear regression analysis was performed after adjustment for age, BMI, 25(OH)-Vitamin D levels, and alkaline phosphatase (ALP) levels.
Multivariate logistic regression analysis was used to assess the association between airway obstruction category and osteopenia/OP after adjustment for age (base model and adjustment for age), and after adjusting for all statistically significant shared risk factors (full model, adjustment for age, BMI, 25[OH] - Vitamin D levels, and ALP levels). Statistical significance was set at p < 0.05 (2-tailed).
RESULTS
The baseline demographics of the study population are presented in table 1. Overall, a total of 164 postmenopausal female patients (mean age 61.38 ± 6.46 years) were included in the present study; encompassing 31 normal controls (mean age 61.28 ± 6.63 years) and 133 COPD patients (mean age 61.40 ± 6.42 years). Subjects in the COPD group had lower FEV1, predicted FEV1, FVC, FEV1/FVC, and T-score, and had a higher prevalence of osteopenia/OP compared with the control group (p < 0.05). There were no differences between the groups with respect to age, BMI, ALP, 25(OH)D, and the prevalence of exposure to second-hand smoke.
Table 1 Baseline characteristics of all subjects
| Characteristics | Controls | Patients | p value |
|---|---|---|---|
| n=31 | n=133 | ||
| Age (years) | 61.28±6.63 | 61.40±6.42 | 0.926 |
| BMI (kg/m2) | 23.15±3.13 | 21.88±3.30 | 0.053 |
| FEV1 (L) | 2.37±0.31 | 1.32±0.32 | <0.001 |
| FEV1% predicted (%) | 90.13±12.31 | 64.90±7.79 | <0.001 |
| FVC (L) | 2.71±0.67 | 2.43±0.52 | 0.012 |
| FEV1/FVC | 0.87±0.05 | 0.53±0.08 | <0.001 |
| ALP, IU/L | 242.27±73.78 | 264.49±80.12 | 0.163 |
| 25(OH)D, ng/ml | 22.41±4.31 | 20.47±5.20 | 0.056 |
| Long acting β2 agonist | 0 | 43 (32.33%) | |
| Exposure to second-hand smoke | 12 (38.71%) | 45 (33.83%) | 0.324 |
| T-score | −0.39±1.12 | −1.01±1.49 | 0.031 |
| Osteoporosis | 5 (16.13%) | 50 (37.59%) | 0.023 |
| Osteopenia | 6 (19.35%) | 53 (39.85%) | 0.032 |
Values are presented as mean ± SD or number (%). 25(OH)D: 25-hydroxyvitamin D, FVC: forced vital capacity, FEV1: forced expiratory volume in 1 second, ALP, alkaline phosphatase.
Based on their FEV1 and predicted FEV1 values, COPD patients were allocated into airway obstruction categories as follows: a mild obstruction group (n=41), a moderate obstruction group (n=65), and a severe/very severe obstruction group (n=27, Table 2). The proportion of patients with osteopenia/OP gradually increased according to the severity of airway obstruction in COPD patients (p < 0.05). In the severe/very severe obstruction group, 59.26% of patients had OP, while 33.33% had osteopenia. FEV1, predicted FEV1, FVC, FEV1/FVC, and T-score were significantly lower in the severe/very severe obstruction group than in the mild and moderate obstruction groups (p < 0.05).
Table 2 Baseline characteristics of COPD in postmenopausal women
| Characteristics | Airway obstruction | p value | ||
|---|---|---|---|---|
| Mild | Moderate | Severe/very severe | ||
| n=41 | n=65 | n=27 | ||
| Age (years) | 60.17±5.79 | 61.79±6.52 | 62.34±7.12 | 0.318 |
| BMI (kg/m2) | 22.53±2.87 | 21.97±3.27 | 20.67±4.01 | 0.078 |
| FEV1 (L) | 1.64±0.23 | 1.31±0.34 | 0.84±0.41 | <0.001 |
| FEV1% predicted (%) | 85.01±7.33 | 61.29±8.29 | 43.07±7.29 | <0.001 |
| FVC (L) | 2.59±0.37 | 2.43±0.45 | 2.18±0.93 | 0.0149 |
| FEV1/FVC | 0.62±0.08 | 0.53±0.07 | 0.38±0.11 | <0.001 |
| ALP, IU/L | 252.19±83.81 | 261.19±77.25 | 291.13±81.43 | 0.1356 |
| 25(OH)D, ng/ml | 20.14±5.24 | 21.09±4.75 | 19.47±6.21 | 0.358 |
| Long-acting β2 agonist | 11 (26.83) | 17 (26.15) | 15 (55.55) | 0.015 |
| Exposure to second-hand | 18 (43.90) | 24 (36.92) | 13 (48.15) | 0.087 |
| Smoke | ||||
| T-score | −0.73±1.31 | -0.91±1.61 | -1.67±1.49 | 0.034 |
| Osteoporosis | 8 (19.51) | 26 (40.0) | 16 (59.26) | 0.004 |
| Osteopenia | 11 (26.83) | 33 (50.77) | 9 (33.33) | 0.037 |
Values are presented as mean ± SD or number (%). 25(OH)D: 25-hydroxyvitamin D, FVC: forced vital capacity, FEV1: forced expiratory volume in 1 second, ALP: alkaline phosphatase.
Results from the analysis of the effect of COPD on the T-score in postmenopausal women are presented in figure 1. Subjects with COPD had significantly lower T-scores (−1.07±1.42) than the control group (−0.38±1.15, p < 0.05, adjusted). Furthermore, among COPD patients, subjects in the severe/very severe obstruction group had lower T-scores (−1.59±1.41) than the mild obstruction group (−0.74±1.26, p < 0.05, adjusted) and the moderate obstruction group (−0.93±1.65, p < 0.05, adjusted).
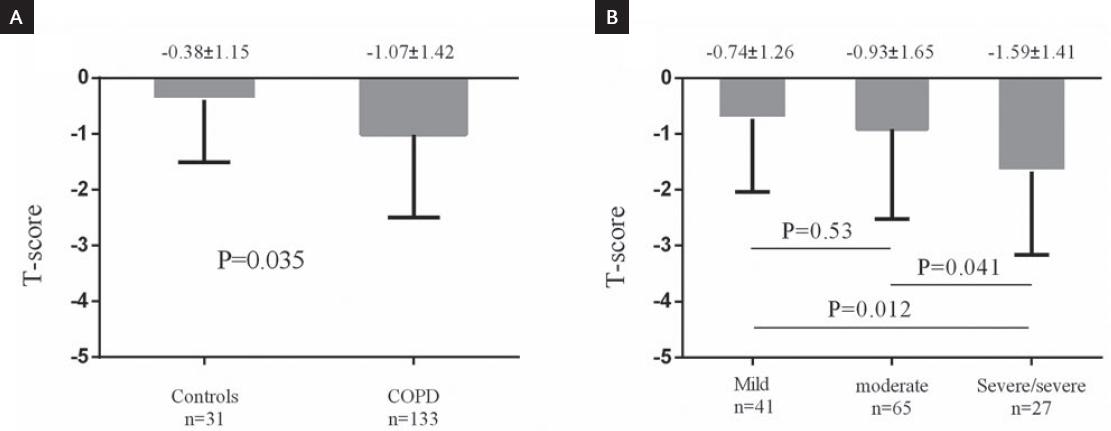
Figure 1 Influence of the chronic obstructive pulmonary disease (COPD) and airway obstruction category on the T-score at the left femoral neck in postmenopausal women. A: Comparison between COPD patients and control subjects. B: Comparison between airway obstruction categories in COPD patients. p values are adjusted by age, body mass index, 25(OH)D, and alkaline phosphatase.
A multivariate logistic regression analysis was used to assess the association between airway obstruction category and osteopenia/OP in all postmenopausal women after adjustment for age (base model), and after adjusting for all risk factors (full model) (Table 3). In the full model, subjects with COPD in the moderate and severe/very severe obstruction groups had higher risks of developing osteopenia (Moderate vs. control, odds ratio [OR] = 1.36, 95% confidence intervals [CI], 1.213-3.693, p=0.038; Severe/very severe vs. control, OR = 3.06, 95% CI, 1.934-9.785, p < 0.001) and OP (Moderate vs. control, 1.94, 95% CI, 1.265-7.676, p = 0.043; Severe/very severe vs. control, OR=3.32, 95% CI, 1.977-7.485, p < 0.001).
Table 3 Multivariate regression analysis between airway obstruction category and osteopenia, osteoporosis
| Characteristics | Osteopenia | Osteoporosis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p value | OR | 95% CI | p value | |
| Base modela | ||||||
| Controls | 1 | 1 | ||||
| Mild | 0.75 | 0.045-1.689 | 0.175 | 0.87 | 0.312-4.874 | 0.582 |
| Moderate | 1.53 | 1.101-3.065 | 0.021 | 2.17 | 1.454-6.983 | 0.017 |
| Severe/very severe | 3.27 | 2.003-7.583 | <0.001 | 4.11 | 2.538-9.535 | <0.001 |
| Full modelb | ||||||
| Controls | 1 | 1 | ||||
| Mild | 0.68 | 0.031-1.896 | 0.245 | 0.73 | 0.543-5.564 | 0.643 |
| Moderate | 1.36 | 1.213-3.693 | 0.038 | 1.94 | 1.265-7.676 | 0.043 |
| Severe/very severe | 3.06 | 1.934-9.785 | <0.001 | 3.32 | 1.977-7.485 | <0.001 |
aAdjusted for age.
bAdjusted for age, BMI, 25(OH)D, and ALP. BMI: body mass index, ALP: alkaline phosphatase, OR: odds ratio, CI: confidence intervals.
DISCUSSION
In this study, postmenopausal women with COPD had lower T-scores and a greater prevalence of osteopenia/OP compared with age-matched female controls. Airway obstruction categories were significantly related to left femoral neck T-scores. Subjects with COPD had higher risks of developing osteopenia and OP than controls. The selection of the study sample aimed to avoid possible confounding factors such as premenopause, smoking and exposure to GCs, and eliminating the contribution of these agents to BMD loss.
In the present study, the prevalence of osteopenia/OP was high, with 39.85% for the former, and 37.59% for the latter. These data appear to be in line with a Japanese study, which found the prevalence of osteopenia/OP in COPD patients to be high, with 46% and 24%, respectively5. Our findings may also be supported by observations from a British study, which showed that 23% of COPD patients had OP in the hip, and 42% had osteopenia10. Moreover, the prevalence of OP has also been reported to be more frequent in postmenopausal women than in age-matched men11. Our research results were significantly higher compared with a published meta-analysis which estimated the prevalence of OP at 35.1%, and the prevalence of osteopenia at 38.4% in COPD patients12. Our findings indicate OP is very common in postmenopausal women with COPD. However, the absolute prevalence is difficult to interpret, as BMD is affected by various characteristics typical of COPD patients, such as race, age, BMI, gender, and exposure to GCs13. OP-associated fractures have been observed to lead to excess mortality in COPD patients4. Therefore, awareness and treatment for OP may be crucial for the management of postmenopausal women with COPD to improve prognosis.
In our study, postmenopausal women with COPD had lower T-scores than those without COPD. The logistic regression analyses confirmed that airway obstruction categories were associated with osteopenia/OP, even after adjustment for potential confounding factors, showing that postmenopausal women with COPD may have a higher risk of osteopenia/OP. Our finding may be supported by observations by Sakurai et al.8, who found that the prevalence of OP in male patients with COPD was significantly higher than in those without COPD, and reduced BMD was associated with airflow limitation in male patients with COPD. Similarly, a casecontrol study showed that COPD was associated with low BMD in the femoral neck in male patients, reporting an OR of 1.5 for OP in COPD male patients compared with controls. However, most of these studies have been based on male COPD patients, while few have focused on postmenopausal women with COPD. A cross-sectional study investigated healthy postmenopausal women and found a correlation between lumbar spine BMD and FEV114. Nevertheless, there are no reports currently available assessing BMD in postmenopausal women with COPD.
In contrast with our study, previous research has failed to find statistically significant differences between the BMD values of COPD and non-COPD subjects. The Fourth and Fifth Korea National Health and Nutrition Examination Surveys (KNHANES IV and V) examined the relationship between BMD and airway obstruction as assessed by FEV1 in 4501 Koreans aged 50 years and older. However, the results do not demonstrate a direct association between BMD and airway obstruction in either gender15. Important factors which could underlie these discrepancies may be the differences in subject characteristics, including race, age, BMI, smoking, Vitamin D intake, menopause, gender, daily physical activity, and GC exposure, all of which can affect BMD in COPD patients13,16-18.
Although the association between COPD and OP has been described extensively in the literature, the exact mechanisms linking these diseases remain unclear. Thesemay include general risk factors such as older age, BMI, and reduced physical activity16,18-20. Weight loss in COPD has been attributed to systemic inflammation and oxidative stress, which may cause metabolic abnormalities in bone tissue indirectly through sarcopenia20. Low BMI has also been shown to predict OP in COPD patients21. Reduced physical activity may equally lead to sarcopenia and reduce sunlight exposure, resulting in Vitamin D deficiency, which may contribute to accelerated bone loss18. On the other hand, disease-specific risk factors, such as systemic inflammation and GC use, also play a key role. Systemic inflammation has been linked to OP and increased bone resorption22. COPD patients with lower BMD have been shown to have higher levels of systemic inflammation as assessed by circulating levels of C-reactive protein and inflammatory cytokines such as TNF-α and interleukin 617. Systemic GC use could decrease the formation of new bone and increase bone loss23-25. The rate of bone loss appears to correlate with the daily dose and duration of therapy; however, reports on this aspect are scarce. Future research should investigate the common pathophysiological links between OP and COPD.
This study has some limitations. First, the cross-sectional design prevents assessment over time. Second, the major limitation of our study is the small sample size, and our findings should be verified in larger samples. Furthermore, information on impaired Vitamin D status, inflammatory cytokines, and physical activity - which may be associated with both COPD and BMD - was not available.
In this study, we investigated the association between BMD and COPD in postmenopausal women. Our results suggest the incidence of osteopenia and OP is higher in COPD patients with no GC exposure compared to ex-smoker controls. Our data also suggest airway obstruction categories may be an appropriate tool for the diagnostic assessment of BMD. This would promote the earlier identification and treatment of OP, which is an important part of the management of COPD in postmenopausal women.











 nueva página del texto (beta)
nueva página del texto (beta)


