Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista de investigación clínica
On-line version ISSN 2564-8896Print version ISSN 0034-8376
Rev. invest. clín. vol.59 n.1 Ciudad de México Jan./Feb. 2007
Carta al editor
Aortic dissection presenting as a febrile disease and atrial fibrillation
Síndrome febril y fibrilación auricular como presentación de la disección aórtica
Jorge Blas–Macedo,* Dolores Márquez–Ramírez,** José de Jesús Gómez–Dominguez**
* Departaments of Internal Medicine and
** Radiology Hospital General del IMSS de Durango.
Correspondence and reprint request:
Jorge Blas Macedo, MD.
Margarita 136
Jardines de Durango.
Fax/Phone Number: 01–618–818–27–33.
E–mail: drjblas@yahoo.com.mx
Recibido el 8 de agosto de 2006.
Aceptado el 11 de enero de 2007.
ABSTRACT
Aortic dissection is a cardiovascular emergency. Its main manifestation is severe chest pain, and approximately 50% of patients present with an elevated systemic blood pressure. Rare reported physical findings include a pulsatile sterno–clavicular joint, dysphagia or testicular tenderness. The absence of sudden onset of pain lowers the likelihood of aortic dissection. We describe a patient in whom aortic dissection was accompanied by fever, nightsweats, suprasternal pain and atrial fibrillation.
Key words. Aortic dissection. Emergency. Nightsweats. Fever. Atrial fibrillation.
RESUMEN
La disección aórtica es una emergencia cardiovascular. La principal manifestación clínica es el dolor torácico severo y agudo. Se acompaña de presión arterial sistémica hasta en 50% de los pacientes en el momento de su presentación. Otras formas inusuales han sido reportadas en la literatura médica como disfagia, movimiento pulsátil en la unión esterno–clavicular y dolor testicular. La ausencia de dolor torácico disminuye la probabilidad de la disección aórtica. Se describe el caso de una paciente en quien la disección aórtica se presentó con fiebre, sudoración profunda, dolor supraesternal y fibrilación auricular.
Palabras clave. Disección aórtica. Emergencia. Sudoración nocturna. Fiebre. Fibrilación auricular.
INTRODUCTION
Dissection is one of the most common disorders of the aorta, with an incidence estimated at 2.9 per 100,000 per year. If the patient survives the acute phase, aortic dissection becomes chronic, its symptoms become less prominent and, past the first 2 weeks, the risk of death decreases rapidly over time.1,2 While abrupt onset and severe chest pain are present in most cases, extraordinary clinical presentations have been reported. In particular, fever or subfebrile temperatures and inflammatory responses have been described in only a few patients.3,4 We observed a patient in whom aortic dissection was manifested as fever, night sweats, suprasternal pain and atrial fibrillation.
CASE REPORT
A 65–year–old woman had suffered from systemic hypertension for 5 years. Her medication regimen included captopril, 50 mg daily, and chlortalidone, 25 mg daily. She presented to the emergency room complaining of abrupt onset of severe pain in the suprasternal notch area, radiating toward the interscapular region. The systemic blood pressure was 150/100 mm Hg, body temperature 39.5 °C, and oxygen saturation 92%. The cardio–pulmonary examination was unremarkable, except for a heart rate at 145 bpm and an irregularly irregular rhythm. The chest roentgenogram showed no abnormalities, the 12–lead electrocardiogram showed atrial fibrillation and non–specific ST segment changes, and all cardiac enzymes were within normal limits. Several hours after admission of the patient to the hospital, the pain resolved. Eight days later, her body temperature was 39.5 °C, the C–reactive protein concentration was elevated at 90 mg/L, erythrocyte sedimentation rate (Westergren method) 100 mm/h, white blood count was 15,000 cells/µL, and hemoglobin concentration 10 mg/d. The blood cultures grew no organism.
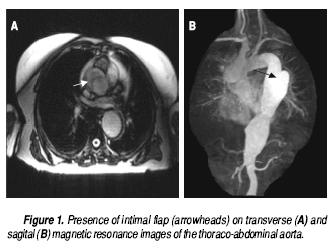
A transesophageal echocardiogram, performed to exclude infective endocarditis, showed normal cardiac valves. However, a dissection flap, starting 1 cm above the aortic valve extending to the thoraco–abdominal aorta, and a small pericardial effusion were present. Computed tomography of the chest showed a Stanford type A dissection of an aneurysmatic ascending aorta, 1 cm above the aortic valve, confirmed by magnetic resonance imaging (Figure 1). Considering her uneventful clinical evolution, stable cardio–pulmonary status, and absence of neurologic deficit, the patient was transferred to another hospital, from which she was discharged 2 weeks later in good condition, on medical treatment only.
DISCUSSION
The diagnosis of aortic dissection is missed on initial presentation in over 50% of patients.5 However imaging methods are currently available, which can confirm the diagnosis when it is suspected. While we favor transesophageal echocadiography the choice of diagnostic methods is often dictated by the resources available, the stability of the clinical status, and the costs involved.6
Aortic dissection rarely presents, as in this case, with fever of unknown origin, sweats, pain in the suprasternal notch area, and during active inflammation, atrial fibrillation. While the etiology of the inflammatory response remains unclear, it has been hypothesized that cytokines are involved since, in patients with abdominal aortic aneurysms, the circulating concentrations of cytokines are elevated and correlate with aneurysm expansion.7,8 While this is a tenable hypothesis in this case, other factors might have caused fever and triggered atrial fibrillation such as acute pericarditis due to the intrapericardial presence of blood. Paroxysmal bouts of sympathetic hyperactivity have recently been described during type A dissection of aorta,9 presenting as fever and arrythmias including atrial fibrillation in a small proportion of cases.10
A long history of hypertension, present in our patient, is a risk factor of both aortic dissection and atrial fibrillation, and the latter can develop in hypertensive patients as a paroxysmal or chronic event.
Current strategies for the treatment of aortic dissection depend on the exent of dissection, but when the ascending aorta is involved, surgical graft replacement must be performed in emergency, since this type of dissection is associated with a high mortality when managed conservatively.11 In this case the decision not to operate was based on the patient's relative clinical stability, as well as on her refusal to consider surgery. The outcomes of surgery are better when it is performed before the development of hemodynamic unstability or worst clinical status.12 Given the elusive presentation of aortic dissection and its similarity to other conditions a high proportion of patients later found to be suffering from aortic dissection are initially suspected to have other disorders, such as acute coronary syndromes, pericarditis, pulmonary embolism or even cholecystitis. In conclusions, physicians should consider the diagnosis of aortic dissection when a patient, particularly elderly, and hypertensive, presents with fever, severe pain in the suprasternal notch area and new onset atrial fibrillation.
REFERENCES
1. Spittell PC, Spitell JA, Joyce JW, et al. Clinical features and differential diagnosis of aortic dissection: experiencie with 236 cases. Mayo Clinic Proc 1993; 68: 642–51. [ Links ]
2. Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA 2000; 283: 897–0. [ Links ]
3. Joya S, del Valle LP, Arenas SS, Sanchez FM, Rodriguez BP. Fever of unknown origin as presentation of chronic aortic dissection. An Med Interna 2004; 21: 569–70. [ Links ]
4. Davutoglu V, Kervancioglu S, Celkan A, Soydinc S, Dinckal H. Painless intimointimal intussusception and fever of unknown origin: an unusual form of aortic dissection. Cardiology 2004; 102: 1–3. [ Links ]
5. Hirst AE, Johns VJ, Kim SW. Diseccting aneurysm of the aorta: a review of 505 cases. Medicine 1958; 37: 217–79. [ Links ]
6. Kasher JA, El–Bialy A, Balingit P. Aortic dissection: a dreaded disease with many faces. J Cardiovasc Pharmacol Ther 2004; 9: 211–18. [ Links ]
7. Swartbol P, Nogren L, Albrechtssson U, et al. Biological responses differ considerably between endovascular and conventional aortic aneurysm surgery. Eur J Vase Endovas Surg 1996; 12: 18–25. [ Links ]
8. Juvonen J, Surcel HM, Satta J, et al. Elevated circulating levels of inflamatory citokines in patients with abdominal aortic aneurysm. Aterioscler Thromb Vase Biol 1997; 17: 2843–7. [ Links ]
9. Rey M, Borrallo JM, Vogel CM, Pereira MA, Várela MA, Diz JC. Paroxysmal sympathetic storms after type a dissection of the aorta. J Cardiothorac Vase Anesth 2005; 19: 654–5. [ Links ]
10. Chew HC, Lim, SH. Aortic disecction presenting with atrial fibrillation. Am J of Emerg Med 2006; 24: 379–80. [ Links ]
11. Nienaber CA, Eagle KA. Aortic dissection: new frontiers in diagnosis and management: part 1: from etiology to diagnosis strategies. Circulation 2003; 108: 628–35. [ Links ]
12. Tsai TT, Nienaber CA, Eagle KA. Acute aortic syndromes. Circulation 2005; 112: 3802–13. [ Links ]














