Introduction
Primary spontaneous hemopneumothorax is a rare pathology, which requires the patient to stay at the hospital to determine the nature of the disease.1 It is defined as the accumulation of >400 mL of blood in the pleural cavity in association with spontaneous pneumothorax.2
Case report
26 years old male, smoker, enters the emergency ward with coughing, left-sided pleuritic chest pain and shortness of breath which developed while he was doing intense physical activity. He had a history of two left spontaneous pneumothorax in the last 8 years which were resolved with a pleural chest tube. On physical examination, the patient was polypneic with dyspneic sounds in the left side of the chest and tympanic percussion. Chest radiography showed complete left lung collapse with hydro-aerial level in the lower zone of the left side (Figure 1).
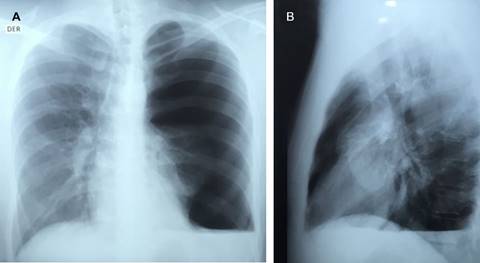
Figure 1: A) Chest radiography showing full collapse of the left lung; B) Hydro-aerial level in the basement of left lung.
We performed a VATS procedure which required intubation with left Robert Shaw 39 and right side decubitus. There were 400 mL of defibrinated blood, clots and a tear near to the emergence of the subclavian artery with active bleeding (Figure 2). Additionally, we found two zones with bullaes in the upper and lower lobe (Figure 3).
Hemorrhage was managed with absorbable hemostat and drainage, furthermore, we performed a wedge resection in the upper and lower lobes with a stapler device in order to treat the bullaes. The patient was discharged on the fourth day of hospital stay in good conditions.
Discussion
The clinical findings of SHP are perilous, they hinge on persistent air quantity in the cavity and blood loss. The most suggestive symptoms are dyspnea, chest pain, anaemia and occasionally shock due to massive intrapleural tension.3,4 The symptomatology can be very similar to primary pneumothorax.
Chest radiography is the most useful diagnostic tool, however, 10% of patients with HNP only display pneumothorax. These patients usually show radiological evidence of hemothorax after the insertion of a pleural catheter.5 This phenomenon can be explained by the early timing of the chest radiograph or the possibility of late haemorrhage due to vascular adhesion.
Three mechanisms have been described (1) tearing of adhesion between the parietal and visceral pleura, (2) rupture of vascularized bullae and underlying lung parenchyma, (3) ripped congenital aberrant vessels attached to parietal pleura.6 The tear of the adhesion at the intrathoracic emergence of the subclavian artery is an almost unique circumstance; in fact there has been only one case report of the literature that is similar to our case.7
Patients with SHP tend to have inefficient hemostasis, given that there are hindering factors that disable correct vasoconstriction. As an example of this event, there have been reported cases of thick, aberrant vessel walls and presence of fibrosis of the intima and middle layer, which contribute to an incomplete vessel closure. Another determining factor is the negative intrapleural pressure due to blood and air stress, which interferes with intraluminal pressure of arteries and veins, which then leads to hemorrhaging that is not proportional to the caliber of the vessel.8
Hemostasis can be obtained by applying pressure in the bleeding site by insufflating the collapsed lung. This principle cannot be applied in the case of hematoma, since the blood does not allow a sufficient lung expansion.9
It has been shown that the most probable bleeding site is the left superior mediastinum and it is relevant to observe this area along with the superior thoracic opening.
The literature reports an incidence of spontaneous hemopneumothorax between 0.5% and 12%.6 However, we only found one case of SHP due to a complete lesion of the left subclavian artery which required hemostatic handling with suture.7 In this case we observed bleeding at the lesion site near to the left subclavian artery that was solved with a hemostatic agent (Surgicel fibrillar™). There was evidence in both cases of adhered bullaes near the bleeding zone. The minimal severity of the lesion allowed a minimally invasive resolution with an excellent post operatory evolution and early discharge.











 text new page (beta)
text new page (beta)




