Introduction
Bronchogenic cyst (BC) is a rare condition that may evolve unsuspected and is incidentally detected.1-5 BC has origin from disordered budding of the primitive tracheobronchial tube before 40 days of gestation.1-5 Clinical manifestations of mediastinal cysts depend upon their site, volume, and regional complications; therefore, progressive chest pain and compressive symptoms of bronchi, trachea, esophagus, or central veins may occur.1-5 Dysphagia, hoarseness, arrhythmia, and hemoptysis are described, in addition to pain, cough and dyspnea.1-5 Chest radiographs show non-calcified masses with soft tissue or water density, or containing air-fluid levels.4 Complete removal of the mass is the recommended procedure for definitive treatment of this condition and allows rule out differential hypotheses with other benign and malignant conditions to establish the final diagnosis.1-5 Classical histopathological findings are respiratory epithelium, cartilage, smooth-muscle and mucous glands.2-5 Late recurrences are rare, but may develop up to 25 years after the incomplete removal of cystic structures; and the possibility of infectious or malignant changes are concerns related to the need of early surgical procedure.2,5 Case studies may help to enhance the suspicion index of non-specialists about scarcely described conditions.
Case presentation
A 40-year-old woman was referred from the outpatient service because of a chronic history of moderate oppressive precordial pain associated with the forward bending movement. Two years before, she started with mild dyspnea on exertion, and in the last ten days the intensity of the chest pain enhanced in spite of analgesic utilization. She did not have palpitations, cough or edema; and denied smoking, alcohol use, illicit drug use, and chest trauma. On admission, she was eutrophic, temperature: 36.8 oC, blood pressure: 120 x 80 mmHg, heart rate: 80 bpm without heart murmurs, respiratory rate: 20 irpm; whereas SpO2 and the rest of physical parameters were unremarkable. Routine laboratory tests, including NT-proBNP, D-dimmers, and the tumor biomarkers were within normal ranges. The electrocardiogram and the transthoracic echocardiogram were normal, but the frontal view of the plain chest radiography showed an ill-defined area of increased opacity at the silhouette of right atrial border (figure 1A). Furthermore, the computed tomography (CT) scans revealed a well delimited soft-tissue-attenuation mass adherent to the pericardial sac behind to the right atrium; and the cystic mass did not show contrast-enhancement in CT evaluation. Worthy of note, there was neither intrapericardial development nor significant compression of the surrounding vital structures of mediastinum by the long growing of the cystic mass. After confirming diagnosis, the mediastinal cyst was removed by posterolateral thoracotomy. Gross and histopathological features of the bronchogenic cyst are shown (figures 1B to 1D). Early postoperative hospital stay was unremarkable, and patient’s discharge occurred on D5; moreover, longstanding outpatient control confirmed the absence of thoracic manifestations.
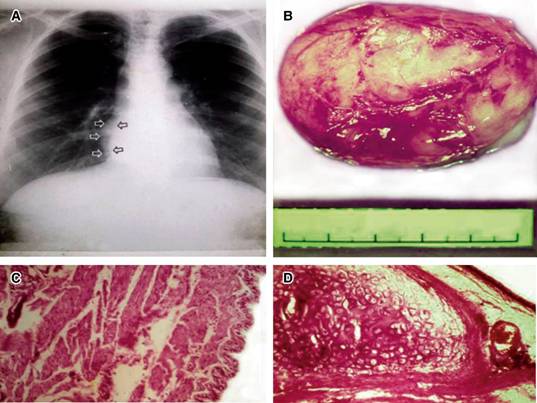
Figure 1: A: Plain radiograph of thorax shows a non-specific image close to the right atrium (arrows); B: Gross aspect of the excised cyst measuring 5.5 x 5.0 cm; C and D: Photomicrographs of samples from cystic wall revealing bronchial structure with ciliated pseudostratified columnar epithelium, submucosal bundles of smooth muscle, cartilage plates and mucous glands, characteristic features of bronchogenic cyst (H & E, high-power).
Discussion
This middle-aged woman presented longstanding thoracic symptoms related to the unsuspected mediastinal BC, which was incidentally detected during the analysis of an abnormal image observed in a chest plain radiography. This occurrence is accordingly with other described cases of thoracic BC diagnosed in the group of adult patients. Her symptoms were dull chest pain not responsive to common analgesics and breathlessness associated with physical efforts, which raised a challenging list of differential diagnoses including benign and malignant conditions. As occur in most of low-income regions, initial investigation was only by plain radiograph that showed abnormal image with water density adjacent to the right atrium, but the exact nature of the mass persisted as a conundrum. Computed tomography (CT) evaluation of the thorax in the case herein described revealed details of the mediastinal mass and thoracotomy was established as the best surgical procedure option, which was promptly performed with success. There was no involvement of lungs, esophagus or vessels by the round cystic mass adhered to the pericardial sac, and was totally removed with special concern on preservation of the cystic wall to prevent relapse. Clinical and imaging routine controls have been done and she follows asymptomatic and in a good health status.
Grozavu C et al. described a case of mediastinal BC in a 42-year-old Romanian woman with a dull central pain in the thorax, which worsened during several weeks and the major concern was about some cardiologic disorder. Routine laboratorial tests and the electrocardiogram were normal, whereas the plain chest radiograph showed a mediastinal mass, also evaluated by angio-CT and found adjacent to the left atrium and adhered to pericardium. Another similarity with the Brazilian case herein reported was the surgical treatment by thoracotomy; however, this BC was intrapericardial and the cystic wall was not entirely removed due to firm adhesions to the great vessels. The authors emphasized the rarity of their findings, and clinical and imaging challenges in patients with BC. Moreover, they commented the commonest sites (mediastinal and intrapulmonary), and less frequent locations as cutaneous, subcutaneous, neck, pericardium, diaphragm, abdomen, vertebral column, and dumbbell presentation.1
Gou C et al. compared 65 video-assisted thoracic surgeries (VATS) [50.8% males, average age of 47 (16-79) years] with 34 thoracotomies [44.2% males, average age of 42 (19-78) years] to treat mediastinal BC in China. They found no significant differences related to the cystic size, incomplete removal, surgical complications, duration of the intensive care support, as well as postoperative complications. The authors concluded that VATS should be preferred with base on shorter operative time, shorter duration of chest drainage, shorter hospital stay, and less perioperative blood loss; but they considered the small size and bias among surgeons as limitations of the study. The possibility of relapses up to 25 years after incomplete removal of the cyst walls was also commented; however, in their opinion this is not related to surgical approaches, but due to the relationships with surrounding structures.2
Hernández-Solís A et al. evaluated clinical data, locations and infectious agents in 12 Mexican cases of BC. The major symptoms were cough and dyspnea (80% each) and fever (40%), and one third were asymptomatic. Males and females were equally (50%) affected, with average age of 49 (22-77) years; the cysts were mediastinal (50%) and intrapulmonary (50%), with average size of 5.3 (1.5-12) cm; and seven (58%) of them were infected. The detected infectious agents were S. aureus, P. aeruginosa, S. pneumonia, H. influenza, and M. tuberculosis. They commented the presence of adherences, and the role of cystic drainage to facilitate the complete removal, in addition to the identification of infectious microorganisms and to decide about the adequate antimicrobial drugs.3
Conclusions
BC is considered a rare condition, more often evolving asymptomatic for long span of time, but it is a potential cause of severe complications that may include compression of the adjacent intrathoracic structures and infections. Diagnostic hypothesis is usually incidental and histopathologic study is mandatory to establish a definite diagnosis. Total removal of the cyst constitutes the best modality of treatment, and the procedure depends upon each case.











 nueva página del texto (beta)
nueva página del texto (beta)


