Introduction
Cardiac tamponade is reported as a severe complication in nearly 15% of acute purulent pericarditis caused by community acquired infection by Staphylococcus aureus,1-15 agent that has been described in up to 36% of purulent effusions in this group of patients.1 Pericardial involvement more often occurs during bloodstream infections, but may origin as an extension of contiguous infectious foci; the main risk factors of this condition include immunosuppression, thoracic surgery, and percutaneous invasive procedure.1,2,4,9,14-16 Additionally to infections, malignancy, myocardial infarction, autoimmune diseases, uremia, hypothyroidism, radiation, drugs, and iatrogenesis can cause pericardial effusions.4,6,9,10,16-18 Purulent pericarditis is a severe condition with up to 40% of mortality even if treated.1,3,7,8,15
The pericardial sac of normal people contains between 15 to 50 mL of serous fluid.18 An acute increasing from 100 to 150 mL of fluid is sufficient to cause cardiac tamponade, and one to two liters of fluid is needed to origin this condition if the accumulation is gradual.18 Cardiac tamponade is clinically suggested by hypotension, high jugular venous pressure, muffled heart sounds; but paradoxical pulse and electrocardiographic and echocardiographic findings have higher sensitivity and specificity for characterization of this condition.1,7,8),(13,16
Hemopericardium may be idiopathic, or due to pacemaker or catheter insertion, pericardiotomy, aortic dissection, malignancy, trauma, uremia, tuberculosis and drugs.2,16-19 Worthy of note is the overlapping of hemorrhagic with other type of pericardial effusion, as described in cardiac tamponade due to purulent pericarditis by Staphylococcal infection.6,17
The modality of drainage procedure is not yet consensual and depends upon the type of effusion, general patient health, physician experience, and institutional resources.9,18 Despite of elevated rate of idiopathic cardiac tamponades (20%), pericardial tissue biopsy is not an essential procedure in the initial phase of diagnostic evaluations and management.9 Autopsy studies in patients with diagnosis of cardiac tamponade due to acute pericarditis have been scarcely reported; so, some physiopathological mechanisms can remain unclear.
Case presentation
An 18-year-old male searched for medical attention complaining of asthenia, fever, shivering, oppressive thoracic pain and orthopnea that started three days prior to admission. His medical antecedents were unremarkable, without alcohol abuse or use of any illicit drugs. He had been fishing in a lagoon and suffered a contaminated injury in the right index finger that evolved with local inflammatory signs and lymphangitis over the ipsilateral forearm. Instead of proper medical orientation he decided control the wound utilizing topical treatment. Physical examination on admission showed 39 oC, hypotension, tachycardia, low SpO2, and oliguria; so, underwent immediate broad spectrum antimicrobials and intensive care support. There was no peripheral edema, hepatojugular reflux or pericardial friction rub; the chest pain intensity did not change with chest positions, and the breath sounds were decreased. He evolved hypotense, with jugular distention, muffled heart sounds and paradoxical pulse. Routine laboratory tests revealed anemia, neutrophilic leukocytosis, thrombocytopenia, hypoalbuminemia, hyponatremia, hyperglycemia; elevated levels of transaminases, urea and creatinine; and urinalysis showed hematuria, high sodium concentration and granular casts. The determinations of erythrocyte sedimentation rate, neutrophil-lymphocyte count ratio, C-reactive protein, and procalcitonin revealed significant elevated levels; whereas the pro-BNP, and all the markers of myocardial necrosis were detected within the normal ranges. The electrocardiographic low voltage and PR segment depression suggesting pericardial effusion, and the echocardiogram showing huge pericardial effusion, collapse of the right chambers, and abnormal movement of interventricular septum indicated cardiac tamponade. A sudden cardiopulmonary arrest occurred before the hospital care for more than four hours and, in spite of the routine resuscitation maneuvers, the death of the patient was inevitable. Pericardial puncture or other invasive procedures were not done before the patient’s death. On postmortem study, the pericardial section revealed a massive hemopericardium, which caused the cardiac tamponade. The heart weighed 330 g (0.43% of the body weight). The aorta and coronary arteries as well as cardiac cavities and valves were all intact. There was associated fibrinous pericarditis, pulmonary edema, hepatic abscess, and acute tubular necrosis (Figure 1). Pulmonary and renal abscesses were also found. Methicillin-resistant Staphylococcus aureus (MRSA) was isolated in abscesses, blood, and pericardial fluid.
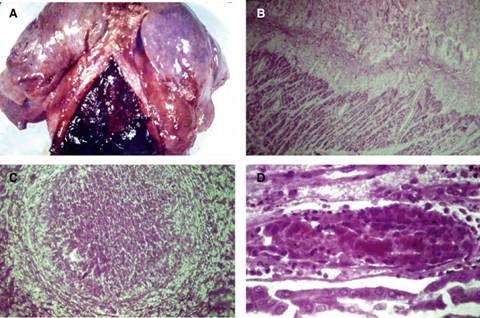
Figure 1: A) Overview of the heart and lungs at autopsy showing, by pericardial section, the partially clotted content of the huge hemopericardium, and edematous lungs; B) (Pericardial biopsy, H&E stain, medium power magnification): presence of edema, mild inflammatory infiltrates and surface fibrin, and absence of abscesses on the serous surface; C) (Liver sample, H&E stain, medium power magnification): histopathological characteristics of the hepatic abscess, which presented with the predominance of neutrophils; and D) (Renal medulla, H&E stain, medium power magnification): features of the acute tubular necrosis characterized by dilation and degenerative changes of tubular cells, and red blood cell casts.
Discussion
Acute pericarditis accounts for nearly 5% of non-ischemic emergency medical help.4 The early diagnosis may constitute a challenging task for primary health care workers. Cardiac tamponade due to purulent pericarditis may be fatal without pericardiocentesis; the echocardiography confirming this diagnosis can be life-saving in emergency attention.7,8,10-13 This clinical condition can be characterized by the following criteria: pericardial chest pain; pericardial rub; new widespread ST elevation or PR depression on ECG; and new or worsening pericardial effusion;18 nevertheless, pericardial effusion is not needed to establish the diagnosis of pericarditis.4 Additional data include elevated inflammatory biomarkers and images of pericardial inflammation by computed tomography and magnetic resonance.4,18 Pericarditis can be categorized in accordance with duration: acute-less than four to six weeks; incessant-more than four to six weeks and less than three months; chronic-more than three months; and recurrent-new episodes occurring at intervals of four to six weeks.4
The infection herein described was acquired in the community, and the agent invaded the blood stream through a skin wound.1 The young patient had an infection by MRSA followed by sepsis that irreversibly evolved to lethal exitus due to cardiac tamponade. Specific causes are easily found in 90% of large effusions, but this occurred after his death;2 the severity of clinical events with very short period for medical support led to this outcome. Based on the autopsy findings, the diagnoses of pericarditis, hemopericardium, and hepatic, renal and pulmonary abscesses, in addition to acute tubular necrosis were characterized. Immediately before death, clinical and complementary data were strongly consistent with the diagnosis of pericarditis and voluminous pericardial effusion evolving to cardiac tamponade. The patient herein reported had an overlap of fibrinous pericarditis with hemopericardium;6,17 the fluid was hemorrhagic, but histologic features were consistent with fibrinous pericarditis. Tuberculosis and viruses are the main causes of pericarditis; a condition categorized as fibrinous, fibrinous purulent, unspecific chronic, hemorrhagic, granulomatous, caseous, constrictive, post-myocardial infarction, and Dressler’s syndrome.2,4,16,19 Hemopericardium is usually associated with tuberculosis, malignant infiltration, and previous cardiac surgery;2,16,19 in the present case study the hemorrhagic fluid had a relationship with S. aureus infection.3 Worthy of note, this agent has been very often associated with blood borne dissemination, evolving to sepsis or shock with acute tubular necrosis, and also myocardial abscess.3,15 Hemorrhagic pericardial effusions found in tuberculosis can be due to eroded lesions into the pericardium;19 similar phenomenon might explain the hemopericardium in the present report. The hypothesis of a S. aureus coinfection with tuberculosis was an initial concern in this patient;13 however, histopathological and microbiological evaluations ruled out this possibility.
The presence of liver abscess might constitute additional concern about differential diagnosis with amebic infection associated with pericardial effusion by the Larrey’s aperture.2 Nevertheless, the autopsy study revealed the bacterial etiology and absence of protozoans; and there were neither open lesions on the hepatic surface, nor fistulous tract to pericardium.
Conclusions
Autopsies can play a significant role to better understanding the physiopathological mechanisms involved in acute pericarditis with effusion causing death by cardiac tamponade. Hemopericardium may be associated with benign and malignant causes of acute pericarditis. Testing biomarkers of bloodstream infection may have clinical value in these conditions. Case studies can enhance the suspicion index, contributing to early diagnosis of pericarditis.











 nueva página del texto (beta)
nueva página del texto (beta)


