Introduction
Diabetic macular edema (DME) is one of the main causes of visual impairment in the world and the main cause of low vision in people with diabetes mellitus.1-3
Optical coherence tomography (OCT) and fluorescein angiography (FA) have been used for DME evaluation and therapeutic monitoring.3,4 An imaging modality of recent advent and application in the assessment of patients with DME is fundus autofluorescence (FAF), a retinal diagnostic method that is used as part of the comprehensive or multimodal evaluation of conditions such as age-related macular degeneration.5,6
Patients with DME may also show abnormalities on FAF, which have been more commonly studied with confocal scanning laser ophthalmoscope systems, and not with flash camera-based systems.5-15 The purpose of this study was to describe the FAF patterns in patients with DME detected by spectral-domain OCT.
Method
Observational, cross-sectional, descriptive, retrospective study in patients with DME assessed at Clínica David, an ophthalmologic unit of the City of Morelia, Michoacán, Mexico, from October 2017 to November 2018. There was access to 280 patients. The research was conducted according to the code of Nuremberg and the principles of the Declaration of Helsinki, and adhering to the guidelines established in the official Mexican standards NOM-004 and NOM-012 of the Ministry of Health.
Patients of either gender and any age, with type 2 diabetes, who presented with clinically and OCT-detected DME, who had undergone a FAF study of adequate quality were included. Patients with intercurrent conditions such as significant cataract, age-related macular degeneration and those who had received intravitreal antiangiogenic treatment or laser therapy were excluded.
Data were extracted from medical records, including information related to the best corrected visual acuity, contrast sensitivity and FA and OCT findings, which are measured in the clinic according to the following standardized procedures:
– Best corrected visual acuity and contrast sensitivity: it was measured with the modified Early Treatment Diabetic Retinopathy Study (ETDRS) chart (Precision Vision, LaSalle, Illinois, USA) at a 4-m distance, under. Contrast sensitivity was measured using the Hamilton-Veale contrast sensitivity chart (Hamilton Veale, Canterbury, New Zealand).
– Fundus photography, FA and FAF: which were obtained with a flash fundus camera (VisucamNM/FA fundus camera, Carl Zeiss Meditec, Oberkochen, Germany). Several photographs were taken and those with artifacts such as shadows were discarded. The selected digital images were saved on a hard disk for subsequent analysis, classification and processing.
– OCT: each patient underwent a spectral-domain OCT scan (Cirrus 5000 SD-OCT model, Carl Zeiss Meditec, Oberkochen, Germany). Of the saved scans, central foveal thickness, macular cube volume and macular average thickness were recorded, as well as DME patterns: cystoid, spongiform (non-cystoid) and serous neuroretinal detachment.
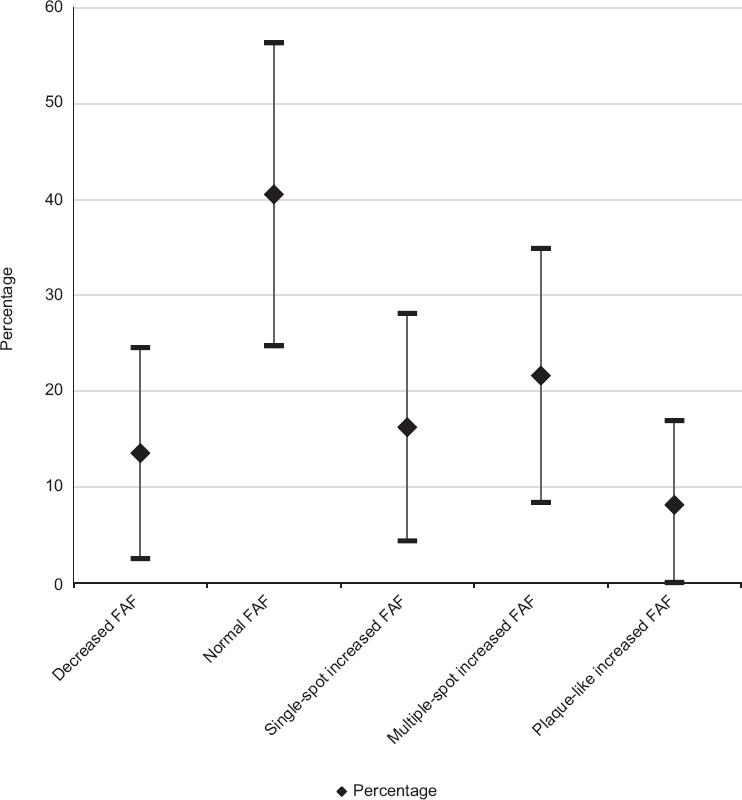
The primary outcome variable was the FAF pattern in the foveal area of each eye. Two expert observers assessed the FAF images, with the following classification being used for this purpose (Figure 1):

Figure 1 Fundus autofluorescence (FAF) patterns in the foveal area: A: Decreased FAF or hypoautofluorescence; B: normal FAF or normoautofluorescence; C: Increased FAF or focal hyperautofluorescence; D: Increased FAF or multifocal hyperautofluorescence; E: Increased FAF or patchy hyperautofluorescence.
– Decreased or hypoautofluorescent FAF pattern.
– Normoautofluorescent or normal FAF pattern.
– Hyperautofluorescent or single-spot increased FAF pattern.
– Hyperautofluorescent pattern or multiple-spot increased FAF pattern.
– Hyperautofluorescent or plaque-like increased FAF pattern.
The percentages and confidence intervals of each autofluorescence pattern in the sample were identified; the kappa coefficient was determined to assess inter-observer variability, with a p-value < 0.05 being regarded as significant.
Results
Forty eyes from 23 patients were assessed (average age 62.8 ± 7.2 years); three eyes of three patients were discarded due to poor image quality, due to a significant cataract. A total of 37 eyes from 20 patients were included; general characteristics of the sample are described in Table 1.
Table 1 General characteristics of the patients in the sample and fundus autofluorescence pattern
| Characteristic | n | % |
|---|---|---|
| Gender | ||
| Male | 12 | 60 |
| Female | 8 | 40 |
| FAF pattern | ||
| Decreased FAF | 5 | 13 |
| Normal FAF | 15 | 40 |
| Single-spot increased FAF | 6 | 17 |
| Multiple-spot increased FAF | 8 | 22 |
| Plaque-like increased FAF | 3 | 8 |
| Edema pattern by fluorangiography | ||
| Focal | 8 | 30.8 |
| Diffuse | 19 | 69.2 |
| Foveal ischemia | ||
| Present | 9 | 32 |
| Absent | 21 | 68 |
| Edema patterns by OCT | ||
| Cystoid | 8 | 22.9 |
| Non-cystoid (spongiform) | 21 | 60 |
| Sub-foveal neuroretina serous detachment | 6 | 17.1 |
| Average ± SD | Range | |
| Age (years) | 62.8 ± 7.2 | 53-59 |
| BCVA, number of letters identified on ETDRS chart | 31.5 ± 16 | |
| SC, number of identified pairs of letters | 7 ± 3.5 | |
| Central foveal thickness by OCT (mm) | 356.3 ± 123.5 | |
| Macular average volume by OCT (mm3) | 10.9 ± 3 | |
| Macular average thickness by OCT (mm) | 363.9 ± 93.9 |
BCVA = best corrected visual acuity, ETDRS = Early Treatment Diabetic Retinopathy Study, SC = sensitivity to contrast, OCT = optical coherence tomography.
The following foveal FAF patterns were detected in the photographic evaluation:
– Hypoautofluorescence (decreased FAF): in five eyes (13.51 %, 95 % CI = 2.50-24.53), a hypoautofluorescent pattern was detected, especially in the peripheral area of the fovea and in the parafoveal area (Figure 1A).
– Normal (normal FAF): in 15 eyes (40.54 %, 95 % CI = 24.72-53.76) a FAF pattern of normal characteristics was detected, i.e. without hyper- or hypoautofluorescent areas within the foveal area (Figure 1B).
– Single-spot hyperautofluorescence (increased single-spot FAF): in six eyes (16.22 %, 95 % CI = 4.34-28.09). In this type of pattern, a single spot of different size was detected within the foveal area, with increased FAF regarding the rest of said area (Figure 1C).
– Multiple-spot hyperautofluorescence (multiple-spot increased FAF): in eight eyes (21.62 %, 95 % CI = 8.36-34.89). In this type, multiple hyperautofluorescent spots were found within the foveal area. Some hyperautofluorescent points corresponded to hard exudates, especially in those with the most refractive appearance in the clinical photographs (Figures 1D and 2).
– Plaque-like hyperautofluorescence (plaque-like increased FAF): it was observed in three eyes (8 %, 95 % CI = 0-16.90). In this type of pattern, a uniform hyperautofluorescent area was observed within the foveal area (Figure 1E).
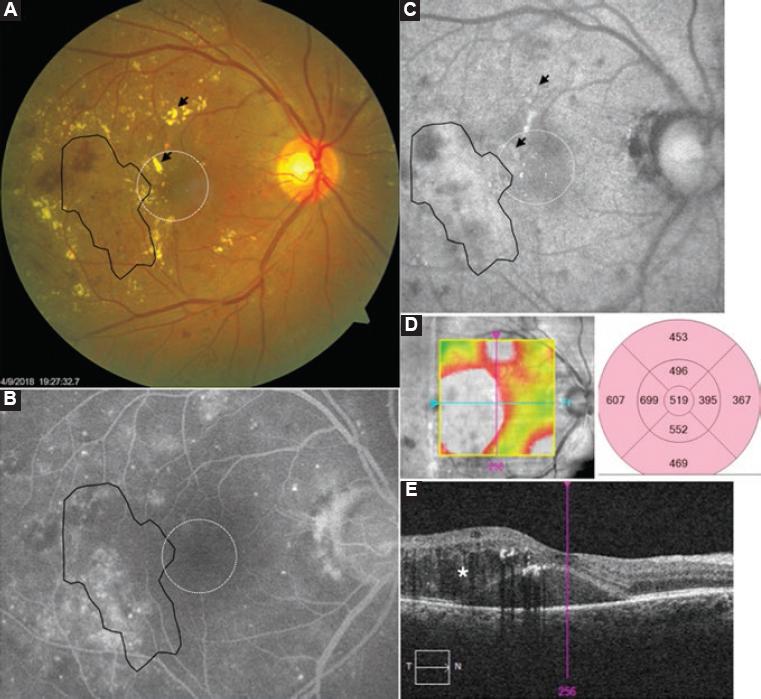
Figure 2 Illustrative case of DME with multifocal hyperautofluorescence foveal pattern (white dotted circle) and patchy fundus autofluorescence (FAF) extrafoveal pattern (black delineated area). A: Posterior pole clinical photograph; arrows indicate hard exudates; B: Arrows indicate increased FAF, which corresponds to the exudates in the clinical photograph. The black delineated area indicates an increased FAF area with a patchy, extrafoveal appearance, which corresponds to the area of leak in the fluorangiography in image C; C: It also corresponds to the area of macular thickening in the infrared image with thickness montage in color of the optical coherence tomography in image D and corresponds to the area with presence of cysts and subfoveal neuroretin serous detachment (*) in image E.
FAF patterns distribution in the sample is presented in Figure 3. Confidence intervals indicate that hypoautofluorescence and hyperautofluorescence patterns were consistently less common than the normal FAF pattern. The kappa coefficient for assessing inter-observer agreement was 0.911 (p < 0.001).
Discussion
FAF has been shown to be a useful tool for the detection and monitoring of various retinal entities such as DME, hereditary retinal disorders and age-related macular degeneration.7
In DME, although FAF has demonstrated its usefulness, its use has been more limited and has spread poorly in the community of doctors dedicated to the treatment of macular pathology.7
Several authors8-15 have described different patterns of FAF change in patients suffering from DME. Pece et al.15 described two types:
– Type 1, which they called multilobed, characterized by multiple areas of increased FAF, similar to the multifocal hyperautofluorescence pattern of our classification.
– Type 2 or unilobed, which corresponds to a large cyst in the OCT image.
– Type 3 or mixed, with types 1 and 2 combined characteristics.
Vujosevic et al.12 described a classification with the following FAF patterns within the foveal area: normal, increased single-spot FAF and increased multiple-spot FAF. In their study, the authors used a confocal scanning laser ophthalmoscope system to obtain the FAF images and considered that those cases that had decreased FAF were the result of the blockage produced by macular pigments on FAF, and thus they considered them to be normal.
In the FAF images obtained by means of flash camera systems, both excitation and emission of the FAF signal occur at a larger wavelength, which translates into a lower density appearance of the macular pigments in the image. There were cases where FAF decreased more than that which we consider a normal pattern, especially in the periphery of the fovea and in the parafovea, which apparently was not caused by the pigments. For this reason, we modified the classification described by Vujosevic et al.12 and added a new pattern: decreased FAF. This pattern might be due to the presence of an increase in retinal thickness at the periphery of the foveal area and should be considered a foveal FAF separate category.
We found three cases with large patches or increased FAF area, which we classified as a plaque-like increased FAF pattern. We believe that the appearance of this pattern is due to the confluence of numerous intra-retinal cysts, which together with the low contrast of FAF images that is characteristic of flash camera systems, gives the appearance of a large patchy or diffuse hyperautofluorescence area in the foveal area.
Another interesting finding was that some points with increased FAF, especially in cases with a pattern of single-spot and multiple-spot increased FAF, corresponded to some exudates of more refractile appearance in the clinical photograph.
Chung et al.10 described a foveolar FAF evaluation system:
– Grade 1, eyes without increased FAF in the foveola.
– Grade 2, eyes with increased FAF in less than half the foveolar area.
– Grade 3, eyes with increased FAF in between half and three quarters of the foveolar area.
– Grade 4, when increased FAF occupied the entire foveolar area.
The classification of the different FAF patterns, especially with confocal systems, has served to design studies whose main purpose has been to assess the correlation between FAF and retinal anatomofunctional variables.9-15
Regarding the limitations of our study, first of all there is the use of a flash camera to obtain the FAF images. Fundus cameras capture more reflected and scattered light in comparison with confocal systems; light scattered from structures outside the retinal plane can artificially increase the FAF signal, a phenomenon known as pseudoautofluorescence.7
Fundus cameras also produce low-contrast images, which can lead to inadequate interpretation of the images due to possible confusion of foveal FAF patterns. In this regard, it would be interesting assessing the role of quantitative FAF methods.
In patients with DME, different FAF patterns occur with flash camera systems. A more accurate phenotypic classification may help determine prognostic factors for visual loss or for the design of other clinical trials for DME.
Finally, FAF is emerging as a study with great potential for the comprehensive assessment of retinal function in current era, in which the diagnostic paradigm based on multimodal retinal imaging prevails.











 nueva página del texto (beta)
nueva página del texto (beta)