Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Salud Pública de México
versión impresa ISSN 0036-3634
Salud pública Méx vol.56 no.4 Cuernavaca jul./ago. 2014
Artículo original
Some current challenges in research on air pollution and health
Desafíos actuales de la investigación sobre contaminación del aire y salud
Jonathan M Samet, MD, MS.(1)
(1) Department of Preventive Medicine, Keck School of Medicine, USC Institute for Global Health, University of Southern California. USA.
Abstract
This commentary addresses some of the diverse questions of current interest with regard to the health effects of air pollution, including exposure-response relationships, toxicity of inhaled particles and risks to health, multipollutant mixtures, traffic-related pollution, accountability research, and issues with susceptibility and vulnerability. It considers the challenges posed to researchers as they attempt to provide useful evidence for policy-makers relevant to these issues. This commentary accompanies papers giving the results from the ESCALA project, a multi-city study in Latin America that has an overall goal of providing policy-relevant results. While progress has been made in improving air quality, driven by epidemiological evidence that air pollution is adversely affecting public health, the research questions have become more subtle and challenging as levels of air pollution dropped. More research is still needed, but also novel methods and approaches to address these new questions.
Key words: air pollutants; health effects; environmental exposure; risk assessment; epidemiology; research challenge; research methodology; public health.
Resumen
Este comentario aborda algunos de los temas de interés actual en relación con los efectos de la contaminación del aire sobre la salud, tales como las relaciones exposición-respuesta, la toxicidad y riesgos para la salud de las partículas inhaladas, las mezclas de contaminantes múltiples, la contaminación relacionada con el tráfico, la investigación sobre responsabilidad, y los problemas de susceptibilidad y vulnerabilidad. Considera los retos que se presentan a los investigadores que intentan proporcionar evidencia para los responsables políticos en estas cuestiones. Este texto acompaña otros trabajos con resultados del proyecto ESCALA, un estudio en varias ciudades de América Latina que tiene como objetivo general proporcionar resultados relevantes para la política pública. Aunque ha habido avances para mejorar la calidad del aire, gracias a la evidencia epidemiológica de que la contaminación aérea está afectando negativamente a la salud pública, las preguntas de investigación se han vuelto más sutiles y difíciles a medida que los niveles de contaminación se reducen. Se necesita más investigación, pero también nuevos métodos y enfoques capaces de enfrentar estas preguntas.
Palabras clave: contaminantes del aire; efectos en la salud; exposición ambiental; medición de riesgo; epidemiología; desafíos en investigación; metodología de la investigación; salud pública.
Serious research on the health effects of air pollution dates to the 1950s, following the London fog of 1952 and other air pollution disasters.1,2 At that time, the motivating concern was the threat to public health of acute excess mortality during times of very high pollution. While this concern persists for much of the world's population living in the growing number of polluted megacities in low- and middle-income countries, air quality control and changes in industry, motor vehicles, power plants, and other sources have greatly lowered air pollution concentrations in many high-income countries. Nonetheless, even in these countries epidemiological studies continue to link current air pollution levels to risk for adverse health effects, leading to a need for ongoing research to provide evidence for policy formulation.3–5 Additionally, levels of air pollution are currently reaching dangerous peaks in many of the megacities in Asia, and recently long unseen high levels of air pollution were measured in London and Paris.
This paper addresses the diverse questions of current interest with regard to the health effects of air pollution (table I). It considers the challenges posed to researchers as they attempt to provide useful evidence for policy-makers relevant to these questions. Appropriately this commentary accompanies papers giving the results from the ESCALA project, a multi-city study in Latin America that has an overall goal of providing policy-relevant results.

Over the decades, epidemiologists addressing air pollution and health have faced methodological challenges, resulting primarily from the non-specificity of outcomes linked to air pollution and the difficulties of exposure estimation. Because of this lack of specificity of the health outcomes of interest, researchers need to take into account the effects of other factors that may also contribute to the occurrence of the measure(s) under study. Such potential confounding is of concern for studies on both short- and long-term time frames, except for situations with abrupt changes in exposure –the London fog of 1952 representing an extreme example– that decouple potential confounders from exposure.6 There has already been substantial consideration of methodological issues arising in epidemiological studies of air pollution.7–9 This manuscript describe ongoing challenges as epidemiologists seek to address topics of greatest relevance to current policy formulation (table I).
Exposure-response relationship
The form of the exposure-response relationship at ambient concentrations is critical to formulating policies protective of public health (figure 1). Figure 1 presents several different exposure-response relationships which might lead to different policy choices. For example, the Clean Air Act in the United States calls for national standards for major pollutants that "... protect the public health with an adequate margin of safety."10 If a threshold can be identified (figure 1, curve D), then a standard set below the point of inflection would meet the Clean Air Act requirements and the degree of protection afforded would depend on the concentration at which the standard was set (figure 1). If risks for a susceptible population follow curve A, then a standard based on curve B might not adequately protect the susceptible group. For two major air pollutants, particulate matter (PM) and ozone (O3), the evidence for diverse outcomes has remained consistent with a linear relationship without threshold,4,11–16 leading to regulatory strategies in the United States that attempt to minimize the burden of pollutant-attributable disease.17–19
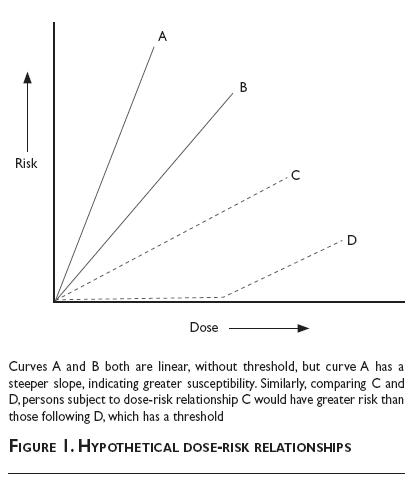
The challenge of describing exposure-response relationships at even lower concentrations is obvious, reflecting the need for a sufficiently large study population, the consequences of exposure measurement error, and the potential for uncontrolled confounding. Large sample sizes are needed, particularly in the setting of the inevitable misclassification of exposure to some extent. Measurement error has many sources and its consequences depend on the underlying patterns of error. Typical "non-differential" measurement error diminishes the signal-to-noise ratio, making it more difficult to detect an effect. Also challenging is distinguishing alternative exposure-response relationships as in figure 1; curvi-linearity may also be of interest. Robust and flexible statistical methods have been proposed for characterizing exposure-response relationships and for taking measurement error into account.20–25 For obtaining sufficiently large sample sizes, investigators have turned to large health-care administrative databases and also pooled data sets from separate studies.15,16,26,27
For example, our team at Johns Hopkins used national databases for mortality and morbidity in time-series analyses, thereby maximizing sample size and the potential to explore informative heterogeneity in effect estimates across the country.7,26,28,29 The mortality analyses were based on data for the 100 largest cities in the US, while the morbidity analyses used the records of the Medicare program, which covers most persons 65 years and older. We also teamed with investigators in Canada and Europe to pool and analyze multi-countries time-series data with a common protocol, one goal being assessment of exposure-response relationships.4 Even analyses of such large databases may leave uncertainty on the key policy issues of the linearity of the exposure-response relationship and the presence of a threshold.
Sources and characteristics of particles and risks to health
Airborne particles have diverse sources and vary substantially over space and time in physical and chemical characteristics. Most air quality standards for particulate matter use mass of airborne particles as the indicator, thus lumping all particles equally, regardless of characteristics and sources. To move from mass-based standards towards more targeted strategies for management of particulate matter air pollution, evidence is needed that addresses whether particular particle characteristics or sources of particles increase the risk of inhaled particles. Over the last decade, motivated by this decision-making need, substantial research has been directed at this topic.30 It was highlighted as pivotal in the series of reports from the US National Research Council's Committee on Research Priorities for Airborne Particulate Matter.31,32
Research on this topic needs to sort through the diverse health effects associated with general indicators of particulate matter and the array of related chemical and physical characteristics. To sift through the many potential associations of risk for adverse health effects with particulate matter characteristics, large data sets are needed, absent strong prior hypotheses. In the United States, the Environmental Protection Agency (EPA) implemented its Speciation Trends Network to provide a platform for research on this topic. The data were organized by the Health Effects Institute (HEI) as a starting point for planning research based in this network (https://hei.aer.com).
Our team at Johns Hopkins used these data to address components of particulate matter and health. Initially, we explored the data descriptively to characterize the extent of correlation among the components, given the common sources of many of them. Bell and colleagues33 showed that most of the variation in mass from day to day came from a limited number of components, implying that potential toxicity of some components might not be readily isolated from that of others. Further analyses addressed associations of components with hospitalization rates. The data on composition were used to explore risk-determining characteristics of particulate matter, using Medicare hospitalization as the outcome measure.34,35 The analyses identified nickel, vanadium, elemental carbon, along with organic carbon matter as associated with higher risk.36,37
These analyses, though based in large national databases, lacked sufficient power to disentangle the separate effects of mixture components. Continued data collection will facilitate further, more powerful analyses as the database grows. Ongoing collection of particle characteristics is to be encouraged to facilitate research. Developing robust evidence on the issue of particulate matter components will require multidisciplinary approaches that combine epidemiology and toxicology.
Characterizing the risks of multipollutant mixtures
The complexity of pollution mixtures, particularly in urban environments, has long been recognized, as have the associated challenges in characterizing the risks to health posed by mixtures. Typically, pollution mixtures vary across urban areas across the day, as traffic and stationary sources vary, and spatially, reflecting the distribution of sources. In the US and many other countries, regulations and control strategies have been directed at single pollutants (e.g., the "criteria" pollutants in the US). The World Health Organization has also published guidelines for major outdoor pollutants.5 While this single pollutant strategy has proved successful so far, there is increasing recognition of the need for multipollutant strategies.32
Dominici and colleagues38 commented on the challenges of carrying out research directed at multiple pollutants or at the toxicity of mixtures, rather than attempting to isolate the effects of particular components through design or analysis. An initial requirement is the availability of data on multiple components that are relevant to health. As mentioned, EPA's Speciation Trends Network facilitates research on particulate matter characteristics. There are not, however, national systems in place in the United States or elsewhere that characterize atmospheric mixtures on an ongoing basis. One approach is to intensely monitor within a defined geographic area and to investigate risks to health of residents within the area in relation to temporal and spatial variation in the mixture. This approach was followed in the ARIES study (Aerosol Research and Inhalation Epidemiology Study) in Atlanta.39–42 A comprehensive monitoring program for particulate matter and components and gaseous pollutants was established and various community-level morbidity and mortality indicators were tracked.
Concern about the health effects of mixtures is not new and the complexities of investigating the health risks of mixtures using epidemiological and toxicological approaches have long been recognized. Even assessing interactions between two components of a mixture has proved challenging.43 Nonetheless, research on mixtures is needed to better characterize those sources contributing to the ongoing burden of morbidity and mortality associated with urban air pollution.
Understanding the risks of traffic-related pollution
Over the last several decades, substantial evidence has accumulated linking exposure to air pollution from traffic with a wide range of adverse effects.44 A systematic review on the topic by the HEI reached the overall conclusion that "...traffic-related emissions affect ambient air quality on a wide range of spatial scales, from local roadsides and urban scales to broadly regional background scales."44 The review also found sufficient evidence to conclude that there is a causal relationship of traffic exposure with exacerbation of asthma. Evidence was judged suggestive of causation for a number of other health outcomes. The possibility that exposure to traffic-related air pollution harms public health has potentially profound and far-reaching implications for the design of cities and transportation planning.45 Research on the topic needs to bring greater certainty to the evidence, given these implications, and to enhance understanding of how the mixture of traffic-related pollutants damages health.
The principal challenge to epidemiological research on traffic lies in exposure characterization. Traffic-related pollution comprises a heterogeneous mixture that varies in composition on brief time frames and over short distances. Fresh vehicle emissions contain immense numbers of small particles, 10-20 nanometers in aerodynamic diameter at their formation; as distance from the roadway increases, the particles quickly grow in size through agglomeration and change in composition through loss of volatile components and chemical transformations.46 The exposures received indoors, presumably directly leading to the associated risks, reflect further changes to the mixture.
Research on traffic continues, using both epidemiologic and toxicologic approaches. Epidemiologists are using modeling approaches to develop indicators of exposure at locations of residences; this approach is feasible but needs to be complemented by more in-depth exposure characterization to generate the evidence-base for air quality management.47,48 Toxicological approaches involve the exposure of animals to real-world traffic pollution, using mobile exposure facilities. This line of investigation is useful for better understanding mechanisms of injury.
Accountability research
In the face of generally improving air quality in a number of countries, including the United States, governments have been asking for estimation of the resulting public health gains. So-called "accountability research" has the objective of characterizing such gains, whether from shorter-term or longer-term initiatives to improve air quality. Several examples of such research are widely cited: the studies by Pope on the consequences of the interruption of the operation of a steel mill in the state of Utah in the United States49–51 and the tracking of mortality in Dublin, Ireland and then other cities in Ireland after the implementation of a ban on coal burning.52,23 Such studies of interventions, particularly if implemented abruptly, have the potential to provide evidence for a causal association by decoupling the change in air pollution from other factors that may confound the association.
In 2003, the HEI published Communication 11, Assessing health impact of air quality regulations: Concepts and methods for accountability research.6 The monograph defined the concept of accountability and accountability research; set the historical and regulatory context for its application; considered methodological issues; and offered a research agenda for accountability. While not explicitly defining accountability, it offered a general framework, the "chain of accountability", for considering accountability research and the implication of its findings (figure 2). The HEI also initiated a program of accountability research.
A review of the resulting studies funded by HEI highlighted the potential limitations of accountability research, particularly for providing clear evidence of benefits.54 Across a diverse portfolio of studies, power had proved to be a key limitation, particularly as interventions had led to smaller effects than anticipated in the design of the accountability studies. There was also a blurred distinction between evaluation of interventions and research that would generate new and deeper understanding of air pollution and health. Recommendations for further accountability research were offered in a report of a workshop held by the HEI.53 The recommendations point to methodological needs as well as refining those circumstances in which accountability research might be considered.
Susceptibility and vulnerability
Although often used interchangeably, susceptibility and vulnerability should be considered as distinct: susceptibility implies a greater risk for outcome at any particular level of exposure while vulnerability refers to a greater likelihood of being exposed or having higher exposure.55 With regard to susceptibility, genetic factors are a current focus but emphasis has long been given to age (e.g., infants and children, and the elderly) and to underlying disease status (e.g., asthma, chronic obstructive pulmonary disease [COPD], and coronary heart disease). For vulnerability, socioeconomic status has been of interest. Those with lower income are more likely to live near point sources of pollution and busy roadways and consequently to be exposed to higher concentrations than the more affluent.56 This issue of vulnerability fits under the general concept of "environmental justice".57
Now, there is rising interest in genetic factors that may affect susceptibility to air pollution. The understanding of mechanisms by which air pollution causes disease, such as oxidative injury and multistage carcinogenesis, provides some insights as to genes that may determine susceptibility. Research has been directed at genes and the respiratory58 and cardiovascular effects59 of air pollution. The AIRGENE Study, for example, is a multi-center European study addressing gene by environment (air pollution) interactions and the oxidative response in survivors of a myocardial infarction.60 Gilliland has addressed the implications of genetic determinants of air pollution effects in children with asthma; he comments on the complex clinical, public health, and regulatory implications of genetically determined susceptibility to air pollution in the large population of children with asthma.61
Susceptibility and vulnerability are considered in setting air quality standards. The US Environmental Protection Agency always considers susceptibility and vulnerability in revising the National Ambient Air Quality Standards (NAAQS), which cover the major pollutants. Susceptibility across the population needs consideration in setting concentration limits for pollutants in outdoor air. Vulnerability needs to be considered in developing control strategies.
Conclusions
Remarkable progress has been made in improving air quality in many cities and regions of the world. This progress has been driven by epidemiological evidence that air pollution is adversely affecting public health. Research questions have become more subtle and challenging as levels of air pollution have dropped in some countries (table I). More research is still needed, but new methods and approaches are required for the new questions. In those places where air pollution concentrations exceed WHO guidelines, at times many-fold, urgent action is needed to control sources and to assure that the pollution does not worsen.
References
1. Bell ML, Samet JM. Air pollution. In: Frumkin H, ed. Environmental health: from global to local. 2nd ed. San Francisco: Jossey-Bass, 2010:387-415. [ Links ]
2. Brimblecombe P. Air pollution and health history. In: Holgate ST, Samet JM, Koren HS, Maynard RL, ed. Air Pollution and Health. San Diego: Academic Press, 1999:5-18. [ Links ]
3. Brook RD, Rajagopalan S, Pope CA, 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 2010;121(21):2331-2378. [ Links ]
4. Katsouyanni K, Samet JM, Anderson HR, Atkinson R, Le Tertre A, Medina S, et al. Air pollution and health: a European and North American approach (APHENA). Res Rep Health Eff Inst 2009(142):5-90. [ Links ]
5. World Health Organization. Air Quality Guidelines: Global Update 2005-Particulate matter, ozone, nitrogen dioxide and sulfur dioxide. Copenhagen: World Health Organization, 2006. [ Links ]
6. Health Effects Institute. Assessing Health Impact of Air Quality Regulations: Concepts and Methods for Accountability Research. HEI Communication 11. Boston, MA: HEI Accountability Working Group, 2003. [ Links ]
7. Samet JM, Zeger S, Dominici F, Dockery D, Schwartz J. The National Morbidity, Mortality, and Air Pollution Study (NMMAPS). Part I. Methods and methodological issues. Cambridge, MA: Health Effects Institute, 2000. [ Links ]
8. Zeger SL, Thomas D, Dominici F, Samet JM, Schwartz J, Dockery D, et al. Exposure measurement error in time-series studies of air pollution: concepts and consequences. Environ Health Perspect 2000;108(5):419-426. [ Links ]
9. Berhane K, Gauderman WJ, Stram DO, Thomas DC. Statistical issues in studies of the long-term effects of air pollution: The Southern California Children's Health Study. Statistical Science 2004;19(3):414-449. [ Links ]
10. U.S. Environmental Protection Agency. The Clean Air Act Amendments of 1990 [accessed July 8, 2014]. Available from: http://www.epa.gov/air/caa. [ Links ]
11. Bell ML, Peng RD, Dominici F. The exposure-response curve for ozone and risk of mortality and the adequacy of current ozone regulations. Environ Health Perspect 2006;114(4):532-536. [ Links ]
12. Pope CA, 3rd, Burnett RT, Krewski D, Jerrett M, Shi Y, Calle EE, et al. Cardiovascular mortality and exposure to airborne fine particulate matter and cigarette smoke: shape of the exposure-response relationship. Circulation 2009;120(11):941-948. [ Links ]
13. Daniels M, Dominici F, Samet JM, Zeger SL. Estimating PM 10 -mortality dose-response curves and threshold levels: an analysis of daily time-series for the 20 largest US cities. Am J Epidemiol 2000;152:397-406. [ Links ]
14. Miller KA, Siscovick DS, Sheppard L, Shepherd K, Sullivan JH, Anderson GL, et al. Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med 2007;356(5):447-458. [ Links ]
15. Beelen R, Raaschou-Nielsen O, Stafoggia M, Andersen ZJ, Weinmayr G, Hoffmann B, et al. Effects of long-term exposure to air pollution on natural-cause mortality: an analysis of 22 European cohorts within the multicentre ESCAPE project. Lancet 2014;383(9919):785-795. [ Links ]
16. Brook RD, Cakmak S, Turner MC, Brook JR, Crouse DL, Peters PA, et al. Long-term fine particulate matter exposure and mortality from diabetes in Canada. Diabetes Care 2013;36(10):3313-3320. [ Links ]
17. U.S. Environmental Protection Agency. National Ambient Air Quality Standards (NAAQS) 2009 [accessed July 8, 2014]. Available from: http://www.epa.gov/air/criteria.html. [ Links ]
18. U.S. Environmental Protection Agency. Policy Assessment for the Review of the Particulate Matter National Ambient Air Quality Standards (Second external review draft). Report No.: EPA 452/P-10-007. Washington, DC: US Environmental Protection Agency, 2010. [ Links ]
19. U.S. Environmental Protection Agency. Health Risk and Exposure Assessment for Ozone (Second External Review Draft). Research Triangle Park, NC: U.S. Environmental Protection Agency, 2014. [ Links ]
20. Dominici F, Zeger S, Samet J. A measurement error correction model for time-series studies of air pollution and mortality. Biostatistics 2000;1(2):157-174. [ Links ]
21. Schwartz J, Zanobetti A. Using meta-smoothing to estimate dose-response trends across multiple studies, with application to air pollution and daily death. Epidemiology 2000;11(6):666-672. [ Links ]
22. Welty LJ, Peng RD, Zeger SL, Dominici F. Bayesian distributed lag models: estimating effects of particulate matter air pollution on daily mortality. Biometrics 2009;65(1):282-291. [ Links ]
23. White RH, Cote I, Zeise L, Fox M, Dominici F, Burke TA, et al. State-of-the-science workshop report: Issues and approaches in low-dose-response extrapolation for environmental health risk assessment. Environ Health Perspect 2009;117:283-287. [ Links ]
24. Bergen S, Sheppard L, Sampson PD, Kim SY, Richards M, Vedal S, et al. A national prediction model for PM2.5 component exposures and measurement error-corrected health effect inference. Environ Health Perspect 2013;121(9):1017-1025. [ Links ]
25. Sheppard L, Burnett RT, Szpiro AA, Kim SY, Jerrett M, Pope CA, 3rd, et al. Confounding and exposure measurement error in air pollution epidemiology. Air Qual Atmos Health 2012;5(2):203-216. [ Links ]
26. Zeger SL, Dominici F, McDermott A, Samet JM. Mortality in the Medicare population and chronic exposure to fine particulate air pollution in urban centers (2000-2005). Environ Health Perspect 2008;116(12):1614-1619. [ Links ]
27. Samoli E, Peng R, Ramsay T, Pipikou M, Touloumi G, Dominici F, et al. Acute effects of ambient particulate matter on mortality in Europe and North America: results from the APHENA study. Environ Health Perspect 2008;116(11):1480-1486. [ Links ]
28. Dominici F, Peng RD, Bell ML, Pham L, McDermott A, Zeger SL, et al. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. JAMA 2006;295(10):1127-1134. [ Links ]
29. Samet JM, Zeger S, Dominici F, Curriero F, Coursac I, Dockery D, et al. The National Morbidity, Mortality, and Air Pollution Study (NMMAPS). Part II. Morbidity and mortality from air pollution in the United States. Cambridge, MA: Health Effects Institute, 2000. [ Links ]
30. US Environmental Protection Agency. Integrated Science Assessment for Particulate Matter (final report). Washington, DC: US Environmental Protection Agency, 2009. [ Links ]
31. National Research Council, Committee on Research Priorities for Airborne Particulate Matter. Research priorities for airborne particulate matter: I. Immediate priorities and a long-range research portfolio. Washington, DC: National Academies Press, 1998. [ Links ]
32. National Research Council, Committee on Research Priorities for Airborne Particulate Matter. Research priorities for airborne particulate matter: IV. Continuing research progress. Washington, DC: National Academies Press, 2004. [ Links ]
33. Bell ML, Dominici F, Ebisu K, Zeger SL, Samet JM. Spatial and temporal variation in PM(2.5) chemical composition in the United States for health effects studies. Environ Health Perspect 2007;115(7):989-995. [ Links ]
34. Bell ML, Ebisu K, Peng RD, Dominici F. Adverse health effects of particulate air pollution: modification by air conditioning. Epidemiology 2009;20(5):682-686. [ Links ]
35. Peng RD, Bell ML, Geyh AS, McDermott A, Zeger SL, Samet JM, et al. Emergency admissions for cardiovascular and respiratory diseases and the chemical composition of fine particle air pollution. Environ Health Perspect 2009;117(6):957-963. [ Links ]
36. Bell ML, Ebisu K, Leaderer BP, Gent JF, Lee HJ, Koutrakis P, et al. Associations of PM2.5 constituents and sources with hospital admissions: analysis of four counties in Connecticut and Massachusetts (USA) for persons >/= 65 years of age. Environ Health Perspect 2014;122(2):138-144. [ Links ]
37. Ostro B, Roth L, Malig B, Marty M. The effects of fine particle components on respiratory hospital admissions in children. Environ Health Perspect 2009;117(3):475-480. [ Links ]
38. Dominici F, Peng RD, Barr CD, Bell ML. Protecting human health from air pollution: shifting from a single-pollutant to a multipollutant approach. Epidemiology 2010;21(2):187-194. [ Links ]
39. Sarnat JA, Marmur A, Klein M, Kim E, Russell AG, Sarnat SE, et al. Fine particle sources and cardiorespiratory morbidity: an application of chemical mass balance and factor analytical source-apportionment methods. Environ Health Perspect 2008;116(4):459-466. [ Links ]
40. Wade KS, Mulholland JA, Marmur A, Russell AG, Hartsell B, Edgerton E, et al. Effects of instrument precision and spatial variability on the assessment of the temporal variation of ambient air pollution in Atlanta, Georgia. J Air Waste Manag Assoc 2006;56(6):876-888. [ Links ]
41. Strickland MJ, Darrow LA, Mulholland JA, Klein M, Flanders WD, Winquist A, et al. Implications of different approaches for characterizing ambient air pollutant concentrations within the urban airshed for time-series studies and health benefits analyses. Environ Health 2011;10:36. [ Links ]
42. Sarnat SE, Sarnat JA, Mulholland J, Isakov V, Ozkaynak H, Chang HH, et al. Application of alternative spatiotemporal metrics of ambient air pollution exposure in a time-series epidemiological study in Atlanta. J Expo Sci Environ Epidemiol 2013;23(6):593-605. [ Links ]
43. Mauderly JL, Samet JM. Is there evidence for synergy among air pollutants in causing health effects? Environ Health Perspect 2009;117(1):1-6. [ Links ]
44. Health Effects Institute. Traffic-Related Air Pollution: A Critical Review of the Literature on Emissions, Exposure, and Health Effects. Special Report 17. Boston, MA: Health Effects Institute, 2009. [ Links ]
45. White RH, Spengler JD, Dilwali KM, Barry BE, Samet JM. Report of workshop on traffic, health, and infrastructure planning. Arch Environ Occup Health 2005;60(2):70-76. [ Links ]
46. Zhu Y, Hinds WC, Kim S, Sioutas C. Concentration and size distribution of ultrafine particles near a major highway. J Air Waste Manag Assoc 2002;52(9):1032-1042. [ Links ]
47. Brauer M. How much, how long, what, and where: air pollution exposure assessment for epidemiologic studies of respiratory disease. Proc Am Thorac Soc 2010;7(2):111-115. [ Links ]
48. Gan WQ, McLean K, Brauer M, Chiarello SA, Davies HW. Modeling population exposure to community noise and air pollution in a large metropolitan area. Environ Res 2012;116:11-16. [ Links ]
49. Pope CA, III. Respiratory disease associated with community air pollution and a steel mill, Utah Valley. Am J Public Health 1989;79:623-628. [ Links ]
50. Pope CA, III. Respiratory hospital admissions associated with PM 10 Pollution in Utah, Salt Lake, and Cache Valleys. Arch Environ Health 1991;46:90-97. [ Links ]
51. Pope CA, III, Schwartz J, Ranson MR. Daily mortality and PM 10 pollution in Utah Valley. Arch Environ Health 1992;47(3):211-217. [ Links ]
52. Clancy L, Goodman P, Sinclair H, Dockery DW. Effect of air-pollution control on death rates in Dublin, Ireland: an intervention study. Lancet 2002;360(9341):1210-1214. [ Links ]
53. Health Effects Institute. Proceedings of an HEI Workshop on further research to assess the health impacts of actions taken to improve air quality. Communication 15. Boston, MA: Health Effects Institute, 2010. [ Links ]
54. van Erp A, Cohen A. HEI's Research Program on the Impact of Actions to Improve Air Quality: Interim Evaluation and Future Directions. HEI Communication 14. Boston, MA: Health Effects Institute, 2009. [ Links ]
55. US Environmental Protection Agency. Integrated Science Assessment of Ozone and Related Photochemical Oxidants (Final Report). Washing, DC: US Environmental Protection Agency, 2013. [ Links ]
56. O'Neill MS, Jerrett M, Kawachi I, Levy JI, Cohen AJ, Gouveia N, et al. Health, wealth, and air pollution: advancing theory and methods. Environ Health Perspect 2003;111(16):1861-1870. [ Links ]
57. American Lung Association. Urban air pollution and health inequities: a workshop report. Environ Health Perspect 2001;109 Suppl 3:357-374. [ Links ]
58. Holloway JW, Savarimuthu-Francis S, Fong KM, Yang IA. Genomics and the respiratory effects of air pollution exposure. Respirology 2012;17(4):590-600. [ Links ]
59. Zanobetti A, Baccarelli A, Schwartz J. Gene-air pollution interaction and cardiovascular disease: a review. Prog Cardiovasc Dis 2011;53(5):344-352. [ Links ]
60. Peters A, Greven S, Heid IM, Baldari F, Breitner S, Bellander T, et al. Fibrinogen genes modify the fibrinogen response to ambient particulate matter. Am J Respir Crit Care Med 2009;179(6):484-491. [ Links ]
61. Gilliland FD. Outdoor air pollution, genetic susceptibility, and asthma management: opportunities for intervention to reduce the burden of asthma. Pediatrics 2009;123 Suppl 3:S168-S173. [ Links ]
Received on: November 14, 2013
Accepted on: July 10, 2014
 Corresponding author:
Corresponding author:
Jonathan M. Samet.
2001 North Soto Street, Suite 330A
Los Angeles, California 90089-9239,
E-mail: jsamet@usc.edu
Declaration of conflict of interests. The author declares that he has no conflict of interests.













