Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Salud Pública de México
versión impresa ISSN 0036-3634
Salud pública Méx vol.57 no.2 Cuernavaca mar./abr. 2015
Artículo original
Energy contribution from non-breastmilk items in low-income Guatemalan infants in their sixth month of life
Contribución de energía de fuentes diferentes a la leche materna en infantes de seis meses de edad de bajos recursos en Guatemala
Marieke Vossenaar, PhD,(1) Jeniece Alvey, MPH,(1) Ilse van Beusekom, MSc,(1) Colleen M Doak, PhD,(2) Noel W Solomons, MD.(1)
(1) Center for Studies of Sensory Impairment, Aging and Metabolism (CeSSIAM). Guatemala City.
(2) Health Sciences, Faculteit der aard-en levenswetenschappen (sectie infectieziekten), Vrije Universiteit. Amsterdam, the Netherlands
Abstract
Objective. To examine the nature and energy contribution of complementary feeding in breastfed infants in their sixth month of life, and the prevalence of the use of bottles as a delivery method.
Materials and methods. We recruited 156 breastfeeding infants at a health clinic in metropolitan Quetzaltenango, Guatemala. A previous-day recall was performed.
Results. Sixty nine mothers (44%) reported offering items other than breastmilk. The median contribution of energy from complementary foods among infants with mixed feeding (n=66) was 197 kcal/day (interquartile range [IQR] 49-353). The median energy contribution of formula or cow's milk among consumers (n=39) was 212 kcal/day (IQR 84-394). Bottles were used on the previous day by 55 (80%) of the 69 mothers not offering exclusive breastfeeding.
Conclusions. Premature introduction of non-breastmilk items is commonly practiced in feeding Guatemalan infants. Adherence to the internationally recognized guidelines for early infant feeding should be an intervention priority for this population.
Key words: infant nutrition; breastfeeding; bottlefeeding; infant formula; Guatemala.
Resumen
Objetivos. Examinar la naturaleza y contribución energética de la alimentación complementaria en infantes lactantes en el sexto mes de vida y la prevalencia del uso de biberones como método de alimentación.
Material y métodos. Se seleccionaron 156 infantes lactantes en un centro de salud en la ciudad de Quetzaltenango, Guatemala. Se solicitó una rememoración de la alimentación del día anterior.
Resultados. Sesenta y nueve madres (44%) reportaron dar alimentos adicionales a la leche materna. La mediana de contribución energética de alimentos complementarios en infantes con alimentación mixta (n=66) fue 197 kcal/día (rango intercuartil [RIC] 43-353). La mediana de contribución energética de leche de vaca entre consumidores (n=39) fue 212 kcal/día (RIC 84-394). De 69 madres que ofrecían alimentación mixta, 55 (80%) proporcionaron biberones.
Conclusiones. Las madres guatemaltecas practican comúnmente la introducción prematura de la alimentación complementaria. La adhesión a las guías internacionalmente reconocidas para alimentación de infantes debe ser una prioridad de intervención en esta población.
Palabras claves: nutrición de infantes; lactancia materna; alimentación artificial con biberón; sucedáneos de leche materna; Guatemala.
The most critical period of life for determining survival to adulthood, optimal growth and development, and health during the entire life span is infancy.1-4 This is particularly true in low-income countries, in which nutritional, social and environmental challenges confront the child from the moment of birth.5,6 The World Health Organization (WHO) recommends that exclusive breastfeeding (EBF) be the sole source of nourishment for infants throughout the first six months of life.2 Upon completing the sixth month -and only then- the pattern should be changed so that the infants "receive nutritionally adequate and safe complementary foods while breastfeeding continues for up to two years of age or beyond".2
EBF is defined by the WHO as the consumption of breastmilk only (including expressed milk or milk from a wet nurse). This feeding pattern does not allow the consumption of any other foods or drinks, not even water, but allows the infant to receive oral rehydration solutions (ORS), drops and syrups (vitamins, minerals and medicines). The WHO considers EBF the ideal feeding pattern in the first semester of life; however, it recognizes a series of other feeding formats with explicit definitions. Predominant breastfeeding (PBF) tolerates the use of certain liquids (water and water-based drinks, fruit juice), ritual fluids and ORS, drops or syrups (vitamins, minerals and medicines), but breastmilk remains the predominant source of nourishment.7,8 Mixed feeding (MF) is the term assigned to the combination of breastfeeding plus the addition of non-breastmilk foods and beverages; in such a way that breastmilk may no longer be the main source of energy. When MF commences at six months of age it sets the basis for potentially appropriate complementary feeding, depending on the quantity, nutritional quality and microbiological safety of the offering. Before this six months cut-off, however, MF is both inappropriate and a hazard to the infant's health.9
According to WHO data, there is a greater than 50% prevalence of EBF at six months of age across Guatemala.10 A pair of parallel protocol studies carried out by our team examining feeding practices from 6-11 months in the central highlands of Guatemala, one rural11 and one urban,12 first alerted us to a potentially higher prevalence of early MF. Furthermore, previously published data on the estimation of feeding patterns among the 156 infants examined in this manuscript revealed differences in the estimated rate of EBF based on the methodology used.13 Using WHO methodology based on the previous day dietary recall method, EBF was reported by 56% of the mothers. EBF rates were 20% estimated by current feeding practices questions and 9% when based on recall of feeding practices since birth. In this study, the introduction of infant formula or ritual fluids in a bottle were the practices that most commonly ended EBF.
The use of bottle feeding at any age is not recommended because unhygienic conditions and improper preparation can put the infant at greater risk of infection and illness.14 When items other than breastmilk are offered to young infants, even when prepared hygienically, the infant can be put at nutritional disadvantage if displacement of breastmilk occurs.5 The Guatemalan National Survey of Maternal and Child Health15 reports that 31.2% of 4 to 6 months old, breastfeed infants are fed with a bottle and 6.1% receive milk substitutes.
As part of the comprehensive study "Xela-Babies",13,16-19 a prospective study of feeding practices, morbidity and growth attainment in the metropolitan area of Quetzaltenango city, we conducted interviews among mother-infant dyads of infants in their sixth month of life. The aim of the current study was to examine the nature and energy contribution of foods and beverages, other than breastmilk, introduced prematurely at the age when infants should still be exclusively breastfed, as well as the prevalence of the use of bottles as a delivery method. We present here the results of this inquiry.
Materials and methods
Setting
This cross-sectional study was conducted in Quetzaltenango, a large metropolitan city in the western highland region of the Republic of Guatemala. The population is composed of Ladino and Indigenous peoples.
Subject population
A convenience sample of 156 participants was selected from mothers who brought infants in their sixth month of life to a public health clinic in metropolitan Quetzaltenango. The public health clinic is generally visited by the lower socioeconomic groups, mainly by those that live at a reasonable distance from the center and have the opportunity to visit. This particular clinic is the only public clinic located in the center of Quetzaltenango. Mothers who visited the clinic for various reasons, such as routine checkups, vaccinations, or illness, were invited to participate in the study. Inclusion criteria were: 1) the infant was in the sixth month of life (five months old); 2) the infant received breastmilk in the previous 24 hours, and 3) the infant and the biological mother were both present at the interview. Exclusion criteria were: 1) the infant was born more than four weeks before the expected birth date; 2) the infant had a sibling participating in the study, and 3) the infant had a diagnosis of a chronic illness or congenital anomalies. Participants were recruited from February to September, 2011.
Data collection
Face-to-face interviews were conducted at the public health clinic by two local Spanish-speaking nutritionists. They were trained and standardized. Sociodemographic data were collected by means of a structured questionnaire including gender, date-of-birth and place of birth of the infant and date-of-birth, age, marital status, parity, level of schooling, and occupation of the mother. The ethnicity of the mother was observed by the mother's use of clothing on the day of the interview. Indigenous Maya women typically wear the traditional clothing of a huipil and corte (colorful woven blouse and skirt).
Mothers were asked whether they had breastfed their infant during the previous 24 hours. A previous day dietary recall of all foods and beverages consumed by the infant as reported by the mother was recorded for infants that were not exclusively breastfed the day prior to the interview. Recipes and preparation methods, as well as brand names, were asked in detail. Portion sizes were estimated with commonly used household measures. When infant formula milk was reported, the brand, number of measures used, volume of water added and delivery method was queried in detail. Breastmilk intake was not quantified.
Ethical approval for this study was obtained from the Human Subjects Committee of the Center for Studies of Sensory Impairment, Aging, and Metabolism (CeSSIAM) and conforms to the provisions of the Declaration of Helsinki in 1995 (as revised in Edinburgh 2000). All mothers of the infants participating in the study were informed about the purpose, procedures, and privacy of the study and signed an informed consent form. The study was registered at the Nederlands Trial Register (TC=3273).
Data analysis
Demographic characteristics
Age of the infant and mother were calculated based on date-of-birth and date-of-interview. Three mothers were unable to report their own date-of-birth, therefore reported age was used. Mothers were grouped according to age: teenagers and adults, the cut-off point being 19 years. Parity was defined as having 1 child or >1 child. The mother's level of schooling was defined as "lower" for primary school or none, and "higher" for secondary or higher schooling. Occupations of the mothers were categorized into two groups: 1) working outside home or 2) housewife or working at home. If the mother was wearing a huipil and corte, the traditional Mayan clothing, she was classified as indigenous, and if wearing modern clothes she was classified as ladina.
Prevalence of consumers of foods and beverages other than breastmilk
The prevalence of consumers of all foods and beverages other than breastmilk was calculated based on the infant's dietary previous-day recall as reported by the mother when any food or beverage other than breastmilk was consumed. When the infant consumed only breastmilk the infant was classified as EBF; when the infant consumed only water-based drinks in addition to breastmilk the infant was classified as PBF, and when foods or beverages other than breastmilk were consumed the infant was classified as MF.20 The number of mentions of all food and beverages other than breastmilk were determined at group level.
Energy analysis of foods and beverages other than breastmilk
Each food or beverage reported in the previous day recall was disaggregated to the most elemental level and entered into an Excel worksheet (Microsoft Corporation®, Redmond, WA, USA). All recipes and individual items portion sizes were converted from household measures into individual intake in grams. Standard portion sizes for infants were previously determined by our local team. The energy contribution from formula milk was calculated based on the reported number of brand specific measures used and the volume of water added. Energy values were primarily derived from USDA National Nutrient Database for Standard Reference version 26.21 Energy values for foods not listed in the USDA database, such as lime-treated maize tortillas and refried black beans, were taken from a food composition compiled specifically for Latin American foods.22 Furthermore, country-specific data was compiled from product labels or from information supplied by the manufacturer for local foods and formula and powdered cow's milk.
The estimated one-day intakes and energy contributions were calculated separately for any items other than breastmilk or water-based drinks, formula and cow's milk, and beverages offered in a bottle or otherwise.
One-day energy intake and energy contribution from breastmilk and other sources
A quantitative assessment of breastmilk consumption was not made. Therefore, estimated intakes were modeled based on the assumption that the energy from breastmilk intake is equal to the energy requirement of the infant minus the energy consumed from complementary foods. This methodology has been used by our team and described in more detail elsewhere.11,12,23,24 In short, total daily energy requirements were computed using the formula: -95.4 + 88.3 * body weight (kg) for both breastfed and formula-fed infants25 using the actual measured weight of the infants.18 When the estimated energy from other food and beverages consumed was higher than the energy requirement, the energy contribution from breastmilk was arbitrarily set at zero.
The one-day estimated energy contribution of breastmilk, all other food and beverage items, and milk were calculated as a percentage of the daily energy intake. In addition, the net sum of energy from various classes of non-breastmilk food and beverage items was related to the total estimated one-day intake of the entire studied sample using the same requirement-based estimate.
Prevalence of bottle users
Infants that used a baby bottle as the method of delivery for any beverage were calculated based on mother's reported previous day-dietary recall for the infant. When mother reported the food item as pacha (bottle) or reported household measures for liquid drinks in relation to bottles (i.e. ounces), the delivery method was considered to be a bottle.
Energy density (dilution) of formula milk
The frequency of use of different brands and types of formula milk was computed. The energy density of formula milk, based on the reported preparation methods, was classified according to the Codex Alimentarius Committee International Expert Group's recommendations as over-diluted (<60 kcal/100ml), normal range (60-70 kcal/100ml) and over-concentrated (>70 kcal/100ml).26
Statistical data analysis
Data were analyzed using SPSS version 17.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics of sociodemographic characteristics of mother-infant dyads are presented by feeding pattern (EBF, MF or bottle users). Difference in sociodemographic characteristics between infants with EBF and MF were examined using chi-square tests. P-values <0.05 were considered statistically significant. Descriptive statistics of estimated one-day intakes (in grams and kcals) of all items other than breastmilk or water-based drinks, formula milk or cow's milk, and beverages offered in a baby bottle are presented. Median one-day energy intakes and energy contribution from breastmilk, all other items and non-breastmilk items are presented.
Results
Response rate
A total of 180 mother-infant dyads were invited to participate in the study. Of these, 24 were excluded for the following reasons: two infants were premature, five infants were severely ill at the time of the interview, 10 infants had not been breastfed the day before the interview, three infants were not of the correct age and four mothers were not able to participate due to schedule restraints. Finally, 156 (87% of those approached) were interviewed. All mothers provided realistic and complete data.
Sociodemographic characteristics
The general sociodemographic characteristics of the infants and mothers are presented by feeding pattern based on a single previous day dietary recall in table I. An equal number of boys (n=78) and girls (n=78) were selected into the study. The mean (±SD) age of the infants was 158±8 days, ranging between 150 and 183 days. Most infants were born in the national hospital (n=88, 56%) or in a private clinic or hospital (n=52, 33%). The mean age of the mothers was 26±6 years, ranging from 16 to 42 years, and 23 (15%) were teenage mothers. The vast majority of mothers were married or united (n=132, 85%). More than one-third of the mothers (n=61, 39%) were primiparous. Among infants with MF the proportion of them with at least one sibling was lower than among those with EBF (46% versus 72%, p<0.001). 77 mothers (49%) had a lower level of schooling (with at most primary school) and 107 (69%) were housewives or worked at home. Among infants with MF the proportion of mothers working outside home was greater than among those with EBF (51% versus 16%, p<0.001).Typical clothing was worn by 37 (24%) of the mothers and were thus classified as indigenous.
Consumption of anything other than breastmilk
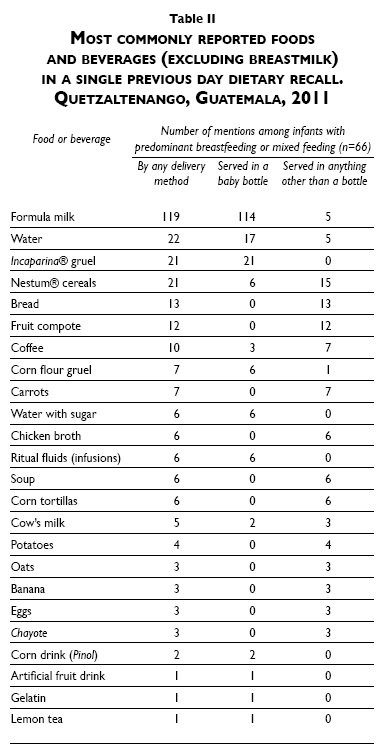
Of the total 156 breastfeeding infants examined, 87 (56%) received only breastmilk on the previous day and were thus classified as EBF, three received a water-based drink (2%) and were thus classified as PBF, and 66 (42%) consumed other foods or beverages and were thus classified as MF. Among the 66 infants with MF at five months of age, 26 foods and beverages, excluding breastmilk, were mentioned in a single previous day recall. All reported items are listed in table II in descending order of frequency of mentions. The most commonly consumed items were formula milk (119 mentions), followed by water (22 mentions), Incaparina® gruel (21 mentions), Nestum® cereals (21 mentions) and bread (13 mentions).
The mean body weight of the 156 infants measured was 6742±783 g, which corresponds to an estimated daily energy requirement of 500±69 kcal. For the 66 infants with MF, the median daily energy contribution from complementary feeding was 197 kcal, with an interquartile range (IQR) between 49 and 353 kcal (table III). The median energy contribution from non-breastmilk food and beverage items was 40% of the total diet (table IV). Finally, when referenced across the estimated intake of the 156 infants in the sample, the cumulative caloric contribution of the 26 reported items in table II constituted 20% of the total one-day energy in the survey (data not shown). For 10 infants, the energy contribution from food and beverage items other than breastmilk was higher than their estimated weight-specific energy requirement; the median difference was 100 kcal.
Consumers of milk other than breastmilk (formula or cow's milk) by any delivery method
A total of 39 infants (25% of the total sample or 59% of those with MF) were offered milk other than breastmilk according to a single previous day recall. This includes both formula milk and cow's milk, delivered in a bottle or otherwise. The median consumption of all milks other than breastmilk among consumers was 284 g and ranged between as little as 5 g to more than 1000 g per day with an IQR between 142 and 570 g (table III). The median daily energy contribution from this milk was 212 kcal, with an IQR between 84 and 394 kcal. The median energy contribution from all non-breastmilk food and beverage items was 52% of the total diet, and the contribution of formula and cow's milk was 39% (table IV). Leaving out the infants whose milk was exclusively cow's milk, the corresponding findings for the remaining 36 infants (55% of infants with MF or 23% of the entire sample) who consumed infant formula milk was an identical median consumption volume, 284 g/day of formula, with an IQR between 142 and 618 g (table III). The energy contribution from just formula milk ranged from 21 to 749 kcal (IQR 92-402 kcal), with a median of 218 kcal/day. Among formula milk consumers, the median energy contribution from all non-breastmilk food and beverage items was 54% of the total diet, and the contribution of formula and cow's milk was 44% (table IV). Finally, when referenced across the estimated intake of the 156 infants in the sample, the energy contribution of the cumulative sum of all the formula feedings presented in figure 1 constituted 12% of total one-day energy in the survey (data not shown).

For more than one-third (36%) of infants who consumed milk other than breastmilk, formula and cow's milk contributed less than one-fourth of the daily energy requirement. For four infants, the energy contribution from formula and cow's milk exceeded the energy requirement on this one given day (data not shown).
Prevalence of consumption of formula milk
As shown in figure 1, there was no overwhelmingly preferred brand of formula milk used by participating mothers, though Enfamil®, Nan 1®, and Similac Advance® were the three brands most frequently consumed. The median energy density of formula milk offered in bottles (114 bottles) was 65.8 kcal/100ml, with an IQR between 63.8 and 67.6 kcal/100 ml. The vast majority of formula preparations (n=80, 69%) were reconstituted within the normal range of energy density, 18 (17%) of the prepared bottles were overdiluted and 16 (14%) were under-diluted. Though a majority of servings were prepared within recommended standards, just over one-third (31%) of all bottles were prepared incorrectly.
Consumption of anything in a baby bottle
None of the mothers reported offering breastmilk in a bottle. Of the 69 infants who consumed anything other than breastmilk, 55 (80%) were offered some form of beverage in a baby bottle. This corresponds to 35% of the entire study sample. All items that were offered in a bottle are listed in table II. The most common beverages served in bottles were formula milk (114 mentions), followed by Incaparina® gruel (21 mentions), water (17 mentions), corn flour gruel (6 mentions), and water with sugar (6 mentions). A total of 10 mothers offered beverages commonly given in bottles using an alternative delivery method; these included formula milk (5 of 119 mentions), water (5 of 22 mentions), coffee (7 of 10 mentions), cow's milk (3 of 5 mentions) and corn flour gruel (1 of 7 mentions).
The estimated amount of beverage offered from a bottle ranged between 28 to 1361g (IQR 142-553 kcal), providing 0 to 749 kcal/day (IQR 38-315 kcal) (table III). A total of 38 infants (24% of bottle users and 69% of the study sample) were offered milk in a bottle, 30 infants (19% of bottle users and 55% of the study sample) were offered another beverage and 13 infants (8% of bottle users and 24% of the study sample) were offered both.
Discussion
The recommendations for early feeding are dually based on the benefits that derive from EBF and the hazard that ensue from other forms of feeding an infant in the first semester of life. These behaviors are highly relevant for Guatemalan children who are at risk for nutritional problems and live in unhygienic environments with high transmission of infectious diseases,27 as reflected by the highest stunting rate in the Americas.28 Our present findings show that, on any given day in the sixth month of life, 44% of mothers provide food or beverage items other than human milk; this is the rate of premature introduction of food and beverages within the sample studied. Among these infants, 40% of dietary energy comes from non-breastmilk energy sources. This is a clear non-adherence to WHO recommendation to defer complementary food introduction until completing six months of age.2
The deviation from adequate early infant feeding practices, as recommended by scientific and policy experts, is a concern for the wellbeing of the child. On the one hand, failure to EBF has consequences for the health and safety of young infants. Gordon et al.29 describe a phenomenon of recurrent diarrhea ("weanling diarrhea") associated with the period in time in which complementary foods are introduced. Victora et al.30 documented that the protective immune properties of human milk could be overcome by exposure to other foods, which probably conveyed food-borne pathogens to the infant.
On the other hand, long-term health benefits of EBF include lower risk of gastrointestinal infection, acute otitis media, and severe lower respiratory disease, and beneficial effects on cardiovascular health, including lower blood cholesterol concentrations and lower blood pressure later in life.4,7,31-35 Conversely, proteins and other constituents of cow's milk represent another risk factor. Among the adverse effects of cow's milk formula are gastrointestinal bleeding,36 milk-protein allergies,37 iron deficiency38 and risk of obesity later in life.39 With respect to the latter, a recent paper out of Egypt40 reports that those infants who were PBF until six months of age or received cow's milk had higher frequencies of anemia and iron deficiency anemia than those infants who received formula milk, which is commonly iron-fortified. Data regarding the relation of iron deficiency anemia and breastmilk are controversial and inconsistent. EBF is the best and recommended practice for infants under six months; furthermore, in low-income countries where anemia is a public health problem, cow's milk is not recommended before 12 months.40 A further factor to consider is that the combination of breastmilk and other items is implicated in higher rates of mother to child transmission of HIV than EBF.41,42
We found a wide variety of non-breast-milk items (n=26) being reported across the sample. The most common item in this group, in terms of times mentioned, volume of consumption and energy consumption was the milk group: infant formula and cow's milk. A wide variety of brands and formulations, available in the local marketplace of the western highlands of Guatemala, were reported as offered to the babies before completion of the sixth month. The energy contribution from formula milk was 9% of the total energy intake among infants with mixed feeding and 44% among formula milk consumers. Older textbooks cite concerns that economic constraints for mothers would induce them to use less milk powder than the recommended amounts for a given volume of prepared formula, producing a hypocaloric dietary regimen for the baby.43 In our population from the lower socioeconomic strata, similar rates of under- and overdilution of formula milk were observed (14 versus 17% of all preparations, respectively). The range of energy density in formulas as reported was narrow, and virtually centered around the actual energy content of human milk of 67 kcal/100 mL.
The hazard to the infant does not stop at the content of the baby bottle, but there are issues with the vessel itself. A 6% minority of the women in the sample used a spoon or cup to feed their infants the non-milk item. As the swallowing control of infants requires maturation, nourishment up to four months can only be obtained by sucking,44,45 whether it be from the nipple of the breast or the bottle. It was established decades ago that, under conditions of inadequate resources for their cleansing and sterilization and improper schooling and orientation to appropriate hygienic practices, bottle feeding can lead to excess morbidity and mortality; these were the bases for the 1981 "Code of Marketing Breast Milk Substitutes".46-49 Lack of refrigeration is an additional factor as bacterial proliferation is accelerated at the ambient temperatures of tropical latitudes. Its role in predisposition to dental caries is widely heralded.50 A final, often unrecognized, hazard of bottle feeding is that of the injuries that can be sustained. In the United States, for instance, it is estimated that over 29 000 infants and toddlers receive injuries associated with baby bottles, most commonly from falls while bottle-feeding.51
Our study has acknowledged strengths and limitations. It emanates from a prospective protocol, using standardized interviewers and detailed questioning about intake, combined with accessing the reported brands and reviewing their ingredient labels. Our convenience sample of mothers visiting the public health clinic in metropolitan Quetzaltenango is unlikely to be representative of the population as a whole, bringing into question the universality of the findings. Access to the public health system is consistently lower among the indigenous population and mothers with no formal schooling are less likely to visit. Nevertheless, observed feeding patterns and stunting rates in young children recruited in this clinic are comparable to representative data.13,18 With any recall assessment of diet, issues of inexactness of memory for items consumed and portions offered on the part of the informants are latent. Beyond this, however, the survey covered only a single day in the life of the infants, such that findings are valid only on the group level. Day to day variation among the mothers in offering non-breastmilk items or bottles but reporting EBF on the day of interview means that our values are likely a major underestimation of exposures when considered over the whole sixth month of life for the subjects of this sample. Moreover, there may be a potential inhibition on the part of informants in admitting practices deemed as being inappropriate in the eyes of the researchers. Finally, we had no direct measurement of breastmilk consumption as a denominator for our contribution-to-energy estimations; although the procedure used has a series of assumptions, it has been accepted by all the reviewers of a series of early papers from our group.11,12,23,24 Due to day-to-day variation in dietary intake, the energy contribution from complementary feeding was higher than their daily energy requirement (by a median of 100 kcal) for 10 infants. At the group level this difference was insignificant.
Conclusions
The early feeding of infants by low-income mothers of the metropolitan areas of Quetzaltenango city can be considered inappropriate and at variance with the WHO recommendations in a large minority of instances. This is driven by a penchant to introduce infant formula and other items, most often in baby bottles. Contrary to a popularized view, the energy delivery in the reconstitution of formula in this population is generally that prescribed by the manufacturer's label. However, bottle feeding is a recognized danger at anytime in an infant's or toddler's life and it should be of no consolation that more than half of the infants had not been fed from a bottle on the day prior to the interview and measures. The policy goal should be zero exposure to this unfortunate and risky practice and efforts should be made to discourage its use, both before and after six months of age.
It is heartening that 10 mothers, at least, have found that feeding a five months old infant with cup or spoon can work for them. Although much more tedious for the caregiver, a cultural inroad for non-bottle administration of liquids seems to have been created, perhaps as an expression of positive deviance.52-54 Focusing on how such women adopted this program should allow, at least, for the safer early administration of ritual fluids and the other liquids that constitute the practice of PBF.
Acknowledgments
We thank the nutritionists who interviewed the mothers (Elena María Díaz Ruiz, Claudia Alejandra Maldonado and Deborah Fuentes), the students who helped recruit participants and enter data (Leonie Peters, Linda Oyesiku, Lydia Kim, Marieke Reurings, Natasha Irving, Óscar Padilla and Robine van der Starre) and the staff of the Quetzaltenango health clinic. Mostly we thank the participants of the study for their collaboration.
Source of funding: Financial support was obtained from Sight and Life, Basel, Switzerland.
References
1. 1 000 Days. 1 000 Days: Change a Life, Change the Future. 2011 [updated 2011; accessed 10 May 2011]; Available from: http://www.thousanddays.org/about/. [ Links ]
2. WHO. Global strategy for infant and young child feeding. Geneva: World Health Organization, 2003. [ Links ]
3. Victora CG, de Onis M, Hallal PC, Blossner M, Shrimpton R. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics 2010;125:e473-80. [ Links ]
4. Fewtrell MS, Morgan JB, Duggan C, Gunnlaugsson G, Hibberd PL, Lucas A, et al. Optimal duration of exclusive breastfeeding: what is the evidence to support current recommendations? Am J Clin Nutr 2007;85:635S-8S. [ Links ]
5. Brown KH, Dewey KG, Allen LH. Complementary feeding of young children in developing countries: A review of current scientific knowledge. Geneva: WHO, 1998. [ Links ]
6. Arabi M, Frongillo EA, Avula R, Mangasaryan N. Infant and young child feeding in developing countries. Child Dev 2012;83:32-45. [ Links ]
7. Bahl R, Frost C, Kirkwood BR, Edmond K, Martines J, Bhandari N, et al. Infant feeding patterns and risks of death and hospitalization in the first half of infancy: multicentre cohort study. Bull World Health Organ 2005;83:418-426. [ Links ]
8. Mihrshahi S, Oddy WH, Peat JK, Kabir I. Association between infant feeding patterns and diarrhoeal and respiratory illness: a cohort study in Chittagong, Bangladesh. Int Breastfeed J 2008;3:28. [ Links ]
9. WHO. Implementing the global strategy for infant and young child feeding. Geneva: World Health Organization, 2003. [ Links ]
10. WHO. World Health Statistics 2010. 2010. [ Links ]
11. Campos R, Hernandez L, Soto-Mendez MJ, Vossenaar M, Solomons NW. Contribution of complementary food nutrients to estimated total nutrient intakes for rural Guatemalan infants in the second semester of life. Asia Pac J Clin Nutr 2010;19:481-490. [ Links ]
12. Hernandez L, Campos R, Enneman A, Soto-Mendez MJ, Vossenaar M, Solomons NW. Contribution of complementary food nutrients to estimated total nutrient intakes for urban Guatemalan infants in the second semester of life. Asia Pac J Clin Nutr 2011;20:572-583. [ Links ]
13. van Beusekom I, Vossenaar M, Montenegro-Bethancourt G, Doak C, Solomons NW. Estimation of exclusive breastfeeding rates among mother-infant dyads in Quetzaltenango, Guatemala varies by interview methods and timeframe. Food Nutr Bull 2013;34:106-108. [ Links ]
14. Mukuria AG, Kothari MT, Abderrahim N. Infant and Young Child Feeding Updates. Calverton, Maryland, USA: ORC Macro, 2006. [ Links ]
15. Ministerio de Salud Pública y Asistencia Social (MSPAS), Instituto Nacional de Estadística (INE), Centros de Control y Prevención de Enfermedades (CDC). National Survey of Maternal and Child Health 2008 [Encuesta Nacional de Salud Materno Infantil 2008 (ENSMI-2008/09)]. MSPAS, 2010. [ Links ]
16. Oyesiku L, Solomons NW, Doak CM, Vossenaar M. Highland Guatemalan women are extremely short of stature, and no lactation duration effects on body composition are observed in a cross-sectional survey. Nutr Rev 2013;33:87-94. [ Links ]
17. Doak CM, van der Starre RE, van Beusekom I, Campos-Ponce M, Vossenaar M, Solomons NW. Earlier introduction of 'agüitas' is associated with higher risk for stunting among infants and toddlers in the Western Highlands of Guatemala. Am J Clin Nutr 2013;97:631-636. [ Links ]
18. Reurings M, Vossenaar M, Doak CM, Solomons NW. Stunting rates in infants and toddlers born in metropolitan Quetzaltenango, Guatemala. Nutrition 2013;29:655-660. [ Links ]
19. Solomons NW, Vossenaar M. Nutrient density in complementary feeding of infants and toddlers. Eur J Clin Nutr 2013;Feb 27. doi: 10.1038/ejcn.2013.46. [Epub ahead of print] [ Links ].
20. WHO, UNICEF, USAID, AED, UCDAVIS, IFPRI. Indicators for assessing infant and young child feeding practices - Part I: Definitions; 2008. Geneva: who, 2008. [ Links ]
21. USDA. National Nutrient Database for Standard Reference. 2012 [updated 2012; accessed September 2012]; Available from: http://www.ars.usda.gov/Services/docs.htm?docid=18879. [ Links ]
22. Bermudez OI, Hernandez L, Mazariegos M, Solomons NW. Secular trends in food patterns of Guatemalan consumers: new foods for old. Food Nutr Bull 2008;29:278-287. [ Links ]
23. Enneman A, Campos R, Hernandez L, Palma AV, Vossenaar M, Solomons NW. Contribution of complementary foods to the total daily water needs of urban Guatemalan infants. J Hum Nutr Diet 2010;23:520-528. [ Links ]
24. Vossenaar M, Hernández L, Campos R, Solomons NW. Several "problem nutrients" are identified in the diet of Guatemalan infants with continued breastfeeding using the concept of 'critical nutrient density' in complementary feeding. Eur J Clin Nutr 2013;67:108-114. [ Links ]
25. UNU, WHO, FAO. Human energy requirements. Report of a Joint FAO/WHO/UNU Expert Consultation, 17-24 October 2001, Rome, Italy. Rome: UNU, WHO, FAO, 2004. [ Links ]
26. Koletzko B, Baker S, Cleghorn G, Neto UF, Gopalan S, Hernell O, et al. Global standard for the composition of infant formula: recommendations of an ESPGHAN coordinated international expert group. J Pediatr Gastroenterol Nutr 2005;41:584-599. [ Links ]
27. Heuveline P, Goldman N. A description of child illness and treatment behavior in Guatemala. Soc Sci Med 2000;50:345-364. [ Links ]
28. World Bank. Nutrition at a Glance: Guatemala 2010 [updated 2010; accessed March 2012]; Available from: http://siteresources.worldbank.org/INTLACREGTOPNUT/Resources/Guatemala4-20-10.pdf. [ Links ]
29. Gordon JE, Chitkara ID, Wyon JB. Weanling diarrhea. Am J Med Sci 1963;245:345-377. [ Links ]
30. Victora CG, Smith PG, Vaughan JP, Nobre LC, Lombardi C, Teixeira AM, et al. Evidence for protection by breast-feeding against infant deaths from infectious diseases in Brazil. Lancet 1987;2:319-322. [ Links ]
31. Arifeen S, Black RE, Antelman G, Baqui A, Caulfield L, Becker S. Exclusive breastfeeding reduces acute respiratory infection and diarrhea deaths among infants in Dhaka slums. Pediatrics 2001;108:E67. [ Links ]
32. Kramer MS, Kakuma R. Optimal duration of exclusive breastfeeding (review). The Cochrane Collaboration 2009. [ Links ]
33. Lamberti LM, Fischer-Walker CL, Noiman A, Victora C, Black RE. Breastfeeding and the risk for diarrhea morbidity and mortality. BMC Public Health 2011;11 Suppl 3:S15. [ Links ]
34. Oddy WH. Long-term health outcomes and mechanisms associated with breastfeeding. Expert Rev Pharmacoecon Outcomes Res 2002;2:161-177. [ Links ]
35. Nutrition ECo, Agostoni C, Braegger C, Decsi T, Kolacek S, Koletzko B, et al. Breast-feeding: A commentary by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr 2009;49:112-125. [ Links ]
36. Fernandes SM, de Morais MB, Amancio OM. Intestinal blood loss as an aggravating factor of iron deficiency in infants aged 9 to 12 months fed whole cow's milk. J Clin Gastroenterol 2008;42:152-156. [ Links ]
37. Friedman NJ, Zeiger RS. The role of breast-feeding in the development of allergies and asthma. J Allergy Clin Immunol 2005;115:1238-1248. [ Links ]
38. Hopkins D, Emmett P, Steer C, Rogers I, Noble S, Emond A. Infant feeding in the second 6 months of life related to iron status: an observational study. Arch Dis Child 2007;92:850-854. [ Links ]
39. Agostoni C, Baselli L, Mazzoni MB. Early nutrition patterns and diseases of adulthood: a plausible link? Eur J Intern Med 2013;24:5-10. [ Links ]
40. Elalfy MS, Hamdy AM, Maksoud SS, Megeed RI. Pattern of milk feeding and family size as risk factors for iron deficiency anemia among poor Egyptian infants 6 to 24 months old. Nutr Res 2012;32:93-99. [ Links ]
41. Tess BH, Rodrigues LC, Newell ML, Dunn DT, Lago TD. Infant feeding and risk of mother-to-child transmission of HIV-1 in Sao Paulo State, Brazil. Sao Paulo Collaborative Study for Vertical Transmission of HIV-1. J Acquir Immune Defic Syndr Hum Retrovirol 1998;19:189-194. [ Links ]
42. Coutsoudis A, Coovadia HM, Wilfert CM. HIV, infant feeding and more perils for poor people: new WHO guidelines encourage review of formula milk policies. Bull World Health Organ 2008;86:210-214. [ Links ]
43. Torun B, Viteri FE. Protein energy malnutrition. In: Shils M, Young V, eds. Modern nutrition in health and disease. 7th ed. Philadelphia: Lea & Febiger, 1988:746-773. [ Links ]
44. Udall JN, Jr. Infant feeding: initiation, problems, approaches. Curr Probl Pediatr Adolesc Health Care 2007;37:374-399. [ Links ]
45. Delaney AL, Arvedson JC. Development of swallowing and feeding: prenatal through first year of life. Dev Disabil Res Rev 2008;14:105-117. [ Links ]
46. Jelliffe DB. Commerciogenic malnutrition? Nutr Rev 1972;30:199-205. [ Links ]
47. Jelliffe DB, Jelliffe EF. Feeding young infants in developing countries: comments on the current situation and future needs. Stud Fam Plann 1978;9:227-229. [ Links ]
48. Baer E, Margulies L. Infant and young child feeding: an analysis of the WHO/UNICEF meeting. Stud Fam Plann 1980;11:72-75. [ Links ]
49. Brady JP. Marketing breast milk substitutes: problems and perils throughout the world. Arch Dis Child 2012;97:529-532. [ Links ]
50. Gaffney KE, Farrar-Simpson MA, Claure D, Davilla G. Prolonged baby bottle feeding: a health risk factor. Pediatr Nurs 2004;30:242-245. [ Links ]
51. Keim SA, Fletcher EN, TePoel MR, McKenzie LB. Injuries associated with bottles, pacifiers, and sippy cups in the United States, 1991-2010. Pediatrics 2012;129:1104-1110. [ Links ]
52. Mattosinho SG, Lovel H, Ebrahim GJ. Positive deviance. J Trop Pediatr 1996;42:247-248. [ Links ]
53. Shekar M, Habicht JP, Latham MC. Use of positive-negative deviant analyses to improve programme targeting and services: example from the TamilNadu Integrated Nutrition Project. Int J Epidemiol 1992;21:707-713. [ Links ]
54. Zeitlin M, Ghassemi H, Mansour M. Positive deviance in child nutrition - with emphasis on pscyococial and behavioural aspects and implications for development. Tokyo: United Nations University Press, 1990. [ Links ]
Received on: July 21, 2014
Accepted on: March 2, 2015
 Corresponding author:
Corresponding author:
Dr. Marieke Vossenaar.
Center for Studies of Sensory Impairment,
Aging and Metabolism. 17 Avenida 16-89 (interior),
Zona 11 (Anillo Periférico). 01011, Guatemala City
E-mail: mvossenaar@hotmail.com, cessiam@guate.net.gt
Declaration of conflict of interests. The authors declare that they have no conflict of interests.













