Introduction
The General Hospital Mexico has successfully implemented it's transplant program, performing in the year 2021: 20 renal transplants, 17 liver transplants, and 10 corneal transplants, completing until the day this manuscript was written a total of 25 renal transplants, 17 liver transplants, and 12 corneal transplants, in addition to having performed the first cardiac transplant on June 9th 2022, positioning our hospital as one of the centres with the most transplants performed at national level.
Case report
Recipient
Male, 31 years old with a previous history of ductus arteriosus closure surgery when he was 2 months old and mechanical valve replacement surgery in mitral position at 25, secondary to severe mitral insufficiency due to congenital heart valve disease. During the previous 3 months to his admission, he presented with ascending edema located on his lower limbs, dyspnea with softer activities than usual, nocturnal orthopnea, and paroxysmal dyspnea which is what lead him to the emergency room at our hospital, an electrocardiogram was performed (Fig. 1A) and thoracic radiography (Fig. 1B), and posterior admission to the Cardiology service. A transthoracic echocardiogram was performed (Fig. 1C and D), which showed a severely dilated left ventricle with a 642 mL end-diastolic volume, 557 ml end-systolic volume, left ventricular ejection fraction (LVEF) of 16% with generalized hypokinesia, global longitudinal strain −3%, dilated right ventricle with depressed systolic function, mechanical valve in ring prosthetics with moderate stenosis and severe paravalvular leak data, severe functional tricuspid insufficiency, and pulmonary artery systolic pressure (PSAP) of 58 mmHg, due to which a right cardiac catheterization was performed, this showed data from mild arterial hypertension. The case was presented to the transplant committee at General Hospital of Mexico "Dr. Eduardo Liceaga" where it was accepted for an orthotopic transplant. From a clinical perspective, he was considered within functional condition NYHA IV despite having optimal medical treatment; considering this, he was admitted to the coronary care unit where he even found himself in need of management with vasopressors, the cardiac transplant was performed on June 9th 2022.
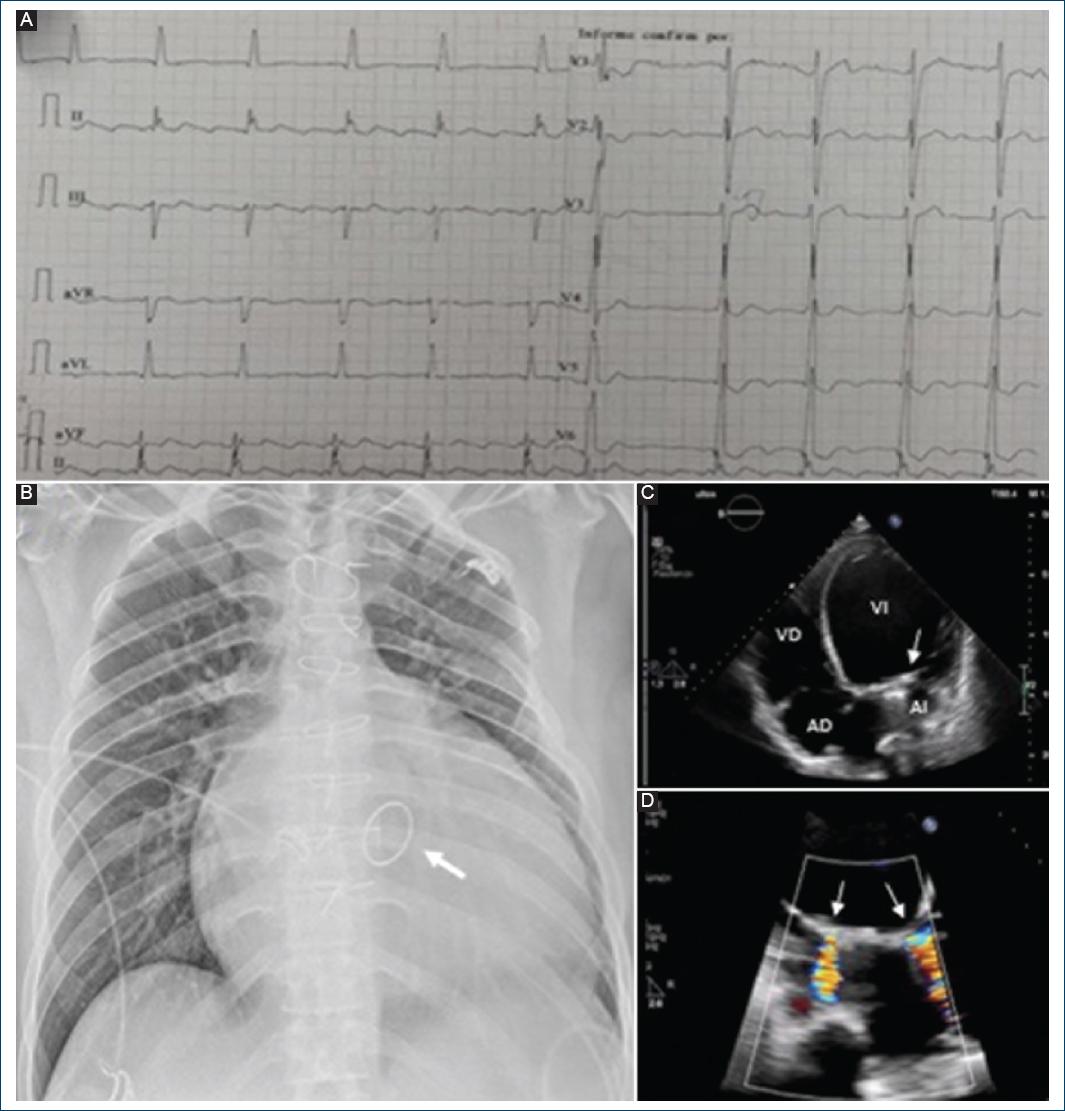
Figure 1 A: electrocardiogram. 12 leads, irregular rhythm, heart rate 60 beats/min, with the presence of F waves compatible with typical flutter, variable conduction hours, QRS axis +0°, QRS 120 ms, without ischemia, injury or necrosis. B: PA chest X-ray. Cardiomegaly and pulmonary venocapillary hypertension are observed, in addition to a mechanical mitral valve (arrow). C and D: transthoracic echocardiogram. Dilation of the left cavities and 2 leaks in the mechanical mitral prosthesis (arrow) are observed.
Donor
Male, 26 years old with a brain death diagnosis secondary to severe head trauma, he was admitted to a public hospital in Queretaro city, the organ harvest was performed 48 h after the brain death diagnosis. During the assessment; hypernatremia and polyuria were documented as well as hemoglobin descent, which required minimal dosage of norepinephrine and hormonal resuscitation with vasopressin, methylprednisolon e and levothyroxine, and the transfusion of 1 erythrocyte concentrate was indicated. A transthoracic echocardiogram was performed and it reported no alterations in the ventricular contractility, LVEF of 60%, right cavities without alterations, no valvular heart disease or short circuits. It did not present hemodynamic instability or important variations within the medium arterial pressure during the peri-operative period (Fig. 2A).
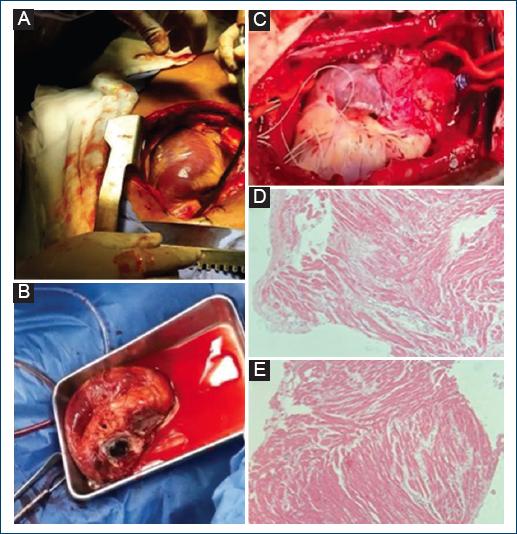
Figure 2 A: heart from a donor patient before extraction. B: heart of recipient patient after extraction. Cardiomegaly and mechanical mitral prosthesis are observed. C: heart transplanted to a recipient patient after aortic unclamping. D: first endomyocardial biopsy with moderate rejection (2R ISHLT) observing multifocal infiltrate and necrosis. E: control endomyocardial biopsy with mild rejection (1R ISHLT) observing focal infiltrate without necrosis.
Surgical procedure
The donor's management was based on maintaining hemodynamic stability based on the use of crystalloids and minimal dosage of norepinephrine, with adequate oxygen saturation and acid base equilibrium. The receptor's anesthetical maintenance management was done with fentanyl, rocuronium, and diazepam, with careful monitorization of vital signs. Methylprednisolone was administered posterior to the aortic unclamping. Cardiopulmonary bypass time was 108 min, aortic clamping time was 85 min, and cold ischemia time was 213 min. To proceed with the cardiectomy cardiopulmonary bypass was started in the conventional form, through canvas and aortic distal cannulation. A grafting surgery was performed, remodeling the anastomosis edges and both pulmonary arteries were communicated. The aortopulmonary graft fold was dissected to be implanted into the receptor into whom a cardiectomy was performed over the auriculoventricular furrow, this was performed respecting the venae cavae's arrival to the right side and respecting a posterior impeller in the left auricle that includes the arrival of the pulmonary veins. The next step was to dissect the aorta and pulmonary arteries as close to the heart as possible to leave enough range to remodel both vessels's anastomosis edges, with the posterior extraction of the surgical piece (Fig. 2B). It was proceeded to perform the first anastomosis to the left auricle, and after the anastomosis to the inferior vena cava, continuing with the superior vena cava, following the pulmonary artery and finally the aorta. The aortic root was vented, a pointy sein was placed in the left auricle for a posterior window, and it was closed with a tourniquet, unclamping the aorta, going into asystole and subsequently sinus bradycardia, placing epicardial pacemaker electrodes in the right ventricle and right auricle, which were exteriorized (Fig. 2C). The procedure was finished, admitting the patient to the intensive coronary care unit of our hospital.
Postoperative
The patient was admitted to the coronary intensive care unit under sedation, mechanical ventilation, and norepinephrine-based vasopressor with a dose of 0.05 mcg/kg/min. Resuscitation was started based on a combination between crystalloids and blood products guided by a floating pulmonary catheter (Swan Ganz) with thermodilution and arterial line, achieving the suspension of the vasopressor. Approximately 60 min he presented with right ventricular dysfunction and subsequently biventricular dysfunction. A transthoracic echocardiogram was performed, it found systolic dysfunction of the right ventricle with tricuspid annular plane systolic excursion (TAPSE) and decreased fractional shortening, LVEF of 40% and pericardial effusion with a layer separation of 30 mm, without cavity collapse, due to this a dobutamine-based inotropic was started with a dose of 3 mcg/kg/min that led to a hemodynamic improvement, with an expected postoperative bleeding. The resuscitation goals were met within 5 h of the immediate postoperative due to which it was decided to fast track the withdrawal of the mechanical ventilation, this was achieved 6 hours after his admission to the coronary unit. Again, this was performed a transthoracic echocardiogram that showed an improved LVEF of 50%, with a persisting right ventricular depression and mild pericardial effusion.
The patient progressed in a favorable manner over the next 12 h subsequently presenting with severe hypotension that did not respond to the administration of crystalloids or blood products, with a low cardiac output hemodynamic profile, normal left ventricle end-diastolic pressure, and low resistance. An urgent transthoracic echocardiogram was performed; it found a LVEF of 60%, right ventricular depression, a continuous mild pericardial effusion, no data of cardiac tamponade. A norepinephrine effusion was started with a poor response which is the reason why vasopressin was administered along with liquid resuscitation improving the arterial tension and cardiac index to 30 min, proceeding to diminish the dose of vasopressors until their suspension. It was decided to get the patient to pericardial effusion drainage 18 h into postoperative care which was performed uneventfully. He progressed to mediate postoperative and late postoperative with acute renal lesion, which improved until his full recovery, with suspension of the inotropes a week after the transplant, without further complications. The echocardiographic assessments at 72 h showed a LVEF of 60% and recovery of the systolic function in the right ventricle. Cardiac rehabilitation was indicated early in the recovery cubicle, 72 h after the surgery by means of telemedicine method, since the cardiac rehabilitator was at that time in Merida Yucatan, Mexico, along with the physical therapists of the General Hospital of Mexico "Dr. Eduardo Liceaga," achieving and completing phase I of the rehabilitation process.
Immunosuppressive therapy
It was decided to utilize as induction therapy for the recipient, Basiliximab, schema of 20 mg on the day of the transplant and 20 mg on the 4th day post-transplant, along with 1g of methylprednisolone after the aortic unclamping. The maintenance schema was discontinued once the patient was extubated with tacrolimus, a dose of 0.1 mg/weight kg divided into two doses and mofetil mycophenolate a dose of 1,440 mg divided into two doses and methylprednisolone 125 mg every 8 h the first day of the transplant, 125 mg every 12 h and 125 mg the second day and 125 mg every 24 h the third day, switching for prednisone a dose of 1 mg/weight kg on the 4th day with a reduction of 10 mg every fourth day with the aim of taking him to a maintenance dose, which is 15 mg a day. The levels of tacrolimus were tested every 48 h until the optimum levels of 18 ng/mL were reached within the first month. The level of mofetil mycophenolate was monitored through the final neutrophil count which were always kept over 1,400 × 10e3/uL. A prophylaxis with valganciclovir and trimethoprim/sulfamethoxazole was also added.
Endomyocardial biopsy
It was performed 10 days post-transplant, 4 samples were sent to be analyzed, this reported moderate rejection (2R) according to the ISHLT (Fig. 2D), due to which, it was decided to start methylprednisolone a dose of 1 g every 24 h for 3 days, the tacrolimus was left to a minimal dose because it was already found in optimum levels and the dose of mycophenolate was augmented up to 2,880 mg for 4 days which caused diarrhea as a side effect, due to this the dose was reduced to 1,440 mg. The endomyocardial biopsy was repeated a week later and it reported mild rejection (1R) according to the ISHLT; consequently, the mycophenolate was adjusted to 1,800 mg without any side effects.
Patient follow-up
A transthoracic echocardiogram was performed in August 2022 that reported a dilated left ventricle, with a LVEF of 54%, Grade III diastolic dysfunction, right ventricle dilated at the medium diameter, preserved systolic function, moderate mitral insufficiency, mild tricuspid insufficiency, and PSAP 47 mmHg.
Patient's progress until now has been positive, maintaining a functional class I of NYHA. Comprehensive treatment for cardiac insufficiency was started since he is considered a class II patient in the AHA/ACC with an adequate tolerance to it, acetylsalicylic acid was added and atorvastatin to prevent the vasculopathy of the graft, cardiac rehabilitation was continued, follow-up with the psychology service, and his inclusion to a support group for cardiac post-transplant patients, gradually rejoining his usual activities. The endomyocardial biopsy checks has been performed monthly with the last rejection report being mild (1R) based on the ISHLT of 2004 (Fig. 2E) and having an adequate adherence to medical treatment.
Discussion
The first successful cardiac transplant in the world was performed on December 3rd 1967 by Dr. Christian Neethling Barnard, at Hospital Grote Schurr in Cape Town South Africa, after extracting the ill heart of the patient Louis WashKansky. However, even though every measure of sterilization was taken, WashKansky died 18 days later, on December 21st 1967, subsequent to pseudomonas pneumonia. From that moment forward the era of heart transplants began worldwide and has been reported in several medical centres1,2.
In Mexico, the first cardiac transplant was performed by Dr. Dr. Rubén Argüero Sánchez as the surgeon responsible and Dr. Rodolfo de Jesús Castaño Guerra as the medic responsible in Centro Médico Nacional "La Raza" belonging to Instituto Mexicano del Seguro Social in 1989. From this first case, a transplant program was successfully implemented in Mexico, placing IMSS as the medical center with the most experience3. Considering a patient with end-stage cardiac insufficiency, cardiac transplant, and circulatory assistance are the only therapeutic option available nowadays that has proven to make a positive and great impact when it comes to the survival rate4. It is indicated for young patients and middle-aged patients with irreversible cardiac pathologies, with no other possibilities of medical treatment or alternative surgical treatment and with a limited life expectancy. The survival rate for a transplant patient is of 75% after the first year and 60% after 5 years. The average length of the graft is 8 years and 6 months5. Patients with a diagnosis of end-stage cardiopathy and potential transplant candidates must follow a very rigorous selection process and their addition to the wait list must be made by a committee in a verified transplant center or a hospital credited for this function, considering the clinical condition of the patient, the appropriate tests, and the results of the social analysis and psychiatric evaluation.
The committee could also define another surgical technique or therapeutical technique for cardiac insufficiency, such as cardiac resynchronization device and implantable defibrillators. If a decision is made that the patient has no other possible therapeutic options and meets all the requirements, it can be incorporated to the national cardiac transplant waitlist6. This reward is not easily obtained and is only possible if you can avoid one of the most efficient mechanisms of survival that human beings possess which is the reconning and subsequent defense against anything strange. Dodging this defense mechanism is one of the most difficult goals to guarantee a successful transplant, but it takes a tall, fundamentally infectious in nature7,8. Immunosuppression regimens utilized within the transplant are used in the induction, as a part of the maintenance or as a way of rescue. As a result of the immunosuppression, opportunistic microorganisms appear as an endogenous reactivation of dormant infections or from an exogenous origin. Its prevention, by means of the proper knowledge of risk factors, its quick diagnosis, and its correct management are fundamentals to guarantee the patient's survival9.
The day June 9th 2022 is a date that will be kept for posterity in the General Hospital of Mexico "Dr. Eduardo Liceaga." Finally, we would like to emphasize the success that was obtained which was due to the organization, human, and medical resources such as nursery, paramedics, and materials, it is also due to our adherence to treatment guidelines and internal hospital norms, to the transplant committee and the coronary care unit.











 nueva página del texto (beta)
nueva página del texto (beta)


