Introduction
Penile fracture (PF) is defined as a traumatic rupture of the tunica albuginea of the corpora cavernosa during penile erection. Although vaginal intercourse is the most common reason for PF, penile manipulation and masturbation have also been shown to be responsible in the etiology1. The recommended treatment of surgery has excellent long-term results1-3. Although complications such as penile curvature, penile deformity, fibrosis, and sexual dysfunction are less common following surgical treatment, overall morbidity rates remain high due to inflammatory and fibrotic processes2-4.
Dexpanthenol has been used in clinical practice for many years as it promotes wound healing5,6. Dexpanthenol is the molecule that is the alcohol form of pantothenic acid and accelerates anti-inflammatory effects by increasing mitotic activity. In the body, it transforms to pantothenic acid, which is a molecule that assists the coenzyme A structure, and by decreasing myeloperoxidase secretion from granulocytes, it halts the formation of free oxygen radicals, while also increasing mitotic activity which results in an anti-inflammatory effect5,7.
The aim of this study was to investigate the effect of dexpanthenol on wound healing at the histopathological level on cavernous tissue. To the best of our knowledge, this is the first study to have examined the use of dexpanthenol in penile cavernous tissue.
Materials and methods
The study was conducted in the Experimental Animals Laboratory of Ankara Training and Research Hospital. Approval for the study was granted by the Local Ethics Committee (approval number: 0055-17.09.19). The study sample was formed of a total of 44 Wistar albino rats, each weighing 220-250 g. Both pre- and postoperatively, all the rats were housed in separate cages at 22°C and 50% humidity with free access to food and water.
On the day of the study, all the rats were administered anesthesia of 50 mg/kg ketamine under sterile conditions. At 1 h before the procedure, a single prophylactic dose of 20 mg/kg ceftriaxone was injected intramuscularly. Then, the rats were positioned supine, the genital area was shaved, and the penis area was wiped with 10% povidone iodine. A 3 Fr urethral catheter was inserted from the external meatus up to the mid-urethral level at approximately 2 cm. The experimental model of PF was created with a number 15 lancet as previously described literature8,9 (Fig. 1). After the interventions, the rats were randomly separated into four study groups as Group B, Group S, Group LD, and Group SD, and a reference group of Group A.
Group A was the reference group with no PF applied. In Group B, the incision was made, then left for secondary healing with no repair. In Group S, the incision line was repaired with 5/0 polyglactin suture. In Group LD, the incision line was repaired with 5/0 polyglactin suture, then 0.25 mg/kg dexpanthenol was applied subcutaneously below the repaired wound region once a day for 14 days. In Group SD, the incision line was repaired with 5/0 polyglactin suture, then 500 mg dexpanthenol was applied intraperitoneally once a day for 14 days.
Six weeks later, all the rats were sacrificed using the cervical dislocation method. The penectomy was performed from proximal of the repaired region using a lancet. The penectomy material obtained from each group was placed in a 10% formaldehyde solution for pathological examination.
Histopathological evaluation using a light microscope was performed by a single independent pathologist blinded to the study groups. The penectomy material of each rat was fixed in 10% formaldehyde until macroscopic examination. Circles of tissue were cut at 4-mm intervals and then embedded in paraffin blocks, from which slices 4 micron in thickness were cut and stained with hematoxylin and eosin (HE) and with Masson trichrome for histopathological examination. Light microscopy examination was made of the preparates at ×20 and ×40 magnification. Fibrosis was evaluated as follows: 0: none, Mild: fibrosis in the focal area or ≤10% of the cavernous body, Moderate: fibrosis in >10%-≤30% of the included cavernosal tissues, and Severe: fibrosis in > 30% of the included cavernosal tissues. Inflammation was evaluated according to the presence of inflammatory cells such as neutrophils, lymphocytes, and monocytes. The groups were compared according to fibrosis and inflammation parameters.
Data obtained in the study were analyzed statistically using PASW 18 software (SPSS/IBM, Chicago, IL, USA). Categorical data were stated as number and percentage. Categorical variables were analyzed using the Pearson Chi-square test. A value of p < 0.05 was considered statistically significant.
Results
One rat in Group S died 12 h after anesthesia, possibly due to anesthesia complications. The most common complications of infection and urinary retention were not observed in any rat.
No severe fibrosis was observed in any rat in Group SD and was determined in one rat in Group B, in one rat in Group S, and in three rats in Group LD (p = 0.001). No fibrosis was observed in 8 (80%) rats in Group SD. The fibrosis rate was significantly lower in Group SD compared to Group B, Group S, and Group LD (p= 0.013, p = 0.005, and p = 0.003, respectively) (Table 1) (Fig. 2). In Group SD, total healing was observed in 8 (80%) rats.
Table 1 Fibrosis rates of the groups
| Fibrosis | Group B | Group S | Group LD | Group SD | p-value |
|---|---|---|---|---|---|
| None (n %) | 1 (10%) | 0 | 0 | 8 (80%) | 0.001* |
| Mild (n %) | 5 (50%) | 6 (66.7%) | 6 (60%) | 2 (20%) | |
| Moderate (n %) | 3 (30%) | 2 (22.2%) | 1 (10%) | 0 | |
| Severe (n %) | 1 (10%) | 1 (11.1%) | 3 (30%) | 0 |
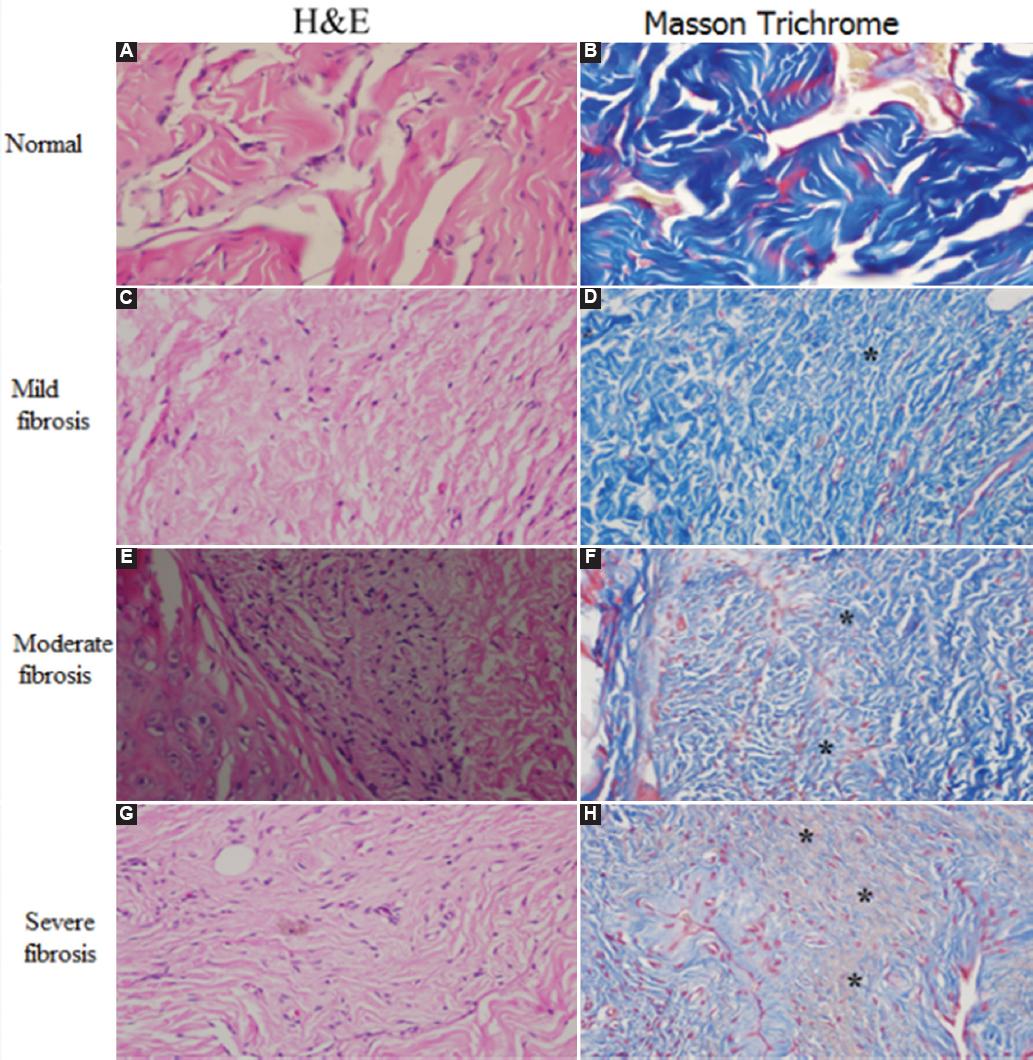
Figure 2 Sections of rat penis (×40). A: H&E image of a normal rat penis in Group A. B: Masson trichrome image of the same rat penis in Group A. C: H&E image of mild fibrosis in Group S. D: Masson trichrome image of mild fibrosis in the same rat penis in Group SD. E: H&E image of moderate fibrosis in Group S. F: Masson trichrome image of moderate fibrosis in the same rat penis in Group S. G: H&E image of severe fibrosis in Group LD. H: Masson trichrome image of severe fibrosis in the same rat penis in Group LD. (*: areas of fibrosis).
When the groups were evaluated in terms of inflammation, the lowest inflammation rate was observed in Group SD (2 rats, 20%), with no statistically significant difference determined between the groups (p = 0.13) (Table 2) (Fig. 3). In the control groups (Groups B and S), fibrosis and inflammation were predominant features of the healing. More extensive fibrosis was observed in these groups than in Group SD.
Discussion
With the occurrence of PF, there can be a sudden cracking or popping sound, pain, and immediate detumescence. There is rapid local swelling of the penile shaft due to a growing hematoma, because PF includes rupture of the tunica albuginea and the enclosed corpus cavernosum10. When PF is diagnosed, the recommended treatment is surgical repair with closure of the tunica albuginea. Negative long-term complications such as penile curvature and deformity are kept to a minimum with this repair and the psychological well-being of the patient is not negatively affected11. Other complications may also be observed such as painful coitus, penile nodule formation, priapism, wound infection, and penile abscess, but the incidence rates of these can be decreased with delicate surgery.
Dexpanthenol was investigated in this study due to its well-known anti-inflammatory, wound healing, and epithelization properties. It also has the advantages of low cost and few side-effects12,13. The role of inflammation in wound healing is a matter of debate since excessive inflammation affects this process negatively. In the present study, fibrosis was not observed in 8 (80%) rats in Group SD. Compared to other groups, these rates were statistically significant and only two rats had mild fibrosis. Similarly, inflammation was not detected in 8 (80%) rats in Group SD, but this was not statistically significant. Interestingly, the fibrosis rate was higher in Group LD. Although mostly mild (60%), fibrosis was observed in all rats in Group LD. This could be explained by different reasons, the first being possibly the microtrauma caused by the subcutaneous application of dexpanthenol for 2 weeks, and the second reason might be that a sufficient concentration of the subcutaneously administered dexpanthenol could not reach the tunica and cavernous tissue.
A previous study by the current author group investigated the effect of intraurethral dexpanthenol in hypospadias repair and intraurethral dexpanthenol administration was found to significantly decrease inflammation and fibrosis. Similarly, in another study by the same group, intraurethral dexpanthenol was used in post-traumatic urethral stricture and was shown to reduce both inflammation and fibrosis14,15. The promising results of those two studies encouraged the current research of the effect of dexpanthenol on wound healing in a PF model. Several studies have shown that dexpanthenol accelerates wound healing after surgery and can successfully prevent scar formation16,17. To the best of our knowledge, this is the first study to have investigated the effect of dexpanthenol on wound healing in an experimental animal model of PF. However, the fact that it was an experimental model is a limitation of the study and there is a need for further advanced clinical studies to confirm these findings.











 nueva página del texto (beta)
nueva página del texto (beta)




