Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Salud Pública de México
versión impresa ISSN 0036-3634
Salud pública Méx vol.56 no.1 Cuernavaca ene./feb. 2014
Artículos originales
Incidence of type 2 diabetes in Mexico. Results of The Mexico City Diabetes Study after 18 years of follow-up
Incidencia de diabetes tipo 2 en México. Resultados del Estudio de la Diabetes en la Ciudad de México después de 18 años de seguimiento
Clicerio González-Villalpando, MD,(1,2) Claudio Alberto Dávila-Cervantes, PhD,(3) Mireya Zamora-Macorra, PhD,(1,2) Belem Trejo-Valdivia, PhD,(4) María Elena González-Villalpando, MD.(2)
(1) Unidad de Investigación en Diabetes y Riesgo Cardiovascular, Instituto Nacional de Salud Pública. México, DF.
(2) Centro de Estudios en Diabetes. México, DF.
(3) Facultad Latinoamericana de Ciencias Sociales (FLACSO). México, DF.
(4) Dirección de Estadística, Centro de Investigación en Evaluación y Encuestas, Instituto Nacional de Salud Pública. Cuernavaca, Morelos, México.
Abstract
Objective. To estimate the incidence of type 2 diabetes (T2D) in Mexican population.
Materials and methods. Population based prospective study. At baseline (1990), the population at risk (1939 non-diabetic adults 35-64 years) was evaluated with oral glucose tolerance test. Subsequent similar evaluations were done (1994, 1998, 2008). American Diabetes Association diagnostic criteria were applied.
Results. The period of observation was 27842 person-years, the cumulative incidence of T2D was 14.4 and 13.7 per 1000 person-years for men and women, respectively. Incidence was 15.8, 15.7 and 12.7 per 1 000 person-years for the second (1994), third (1998) and fourth (2008) follow-up phases, respectively. The mean age at diagnosis was 44 years for prevalent cases and 56 years for incident cases.
Conclusions. This is the first estimate of long-term incidence of T2D in Mexican population. The incidence is among the highest reported worldwide. It remained with few changes throughout the study period.
Keywords: diabetes mellitus; incidence; urban population.
Resumen
Objetivo. Estimar la incidencia de diabetes mellitus tipo 2 (T2D) en México.
Material y métodos. Estudio prospectivo, de base poblacional. En el examen basal (1990) se evaluó a 1939 participantes normoglucémicos, con curva de tolerancia a la glucosa. Se realizó examen similar en tres evaluaciones subsecuentes (1994, 1998, 2008). Se aplicaron criterios recomendados por la American Diabetes Association.
Resultados. En el tiempo de observación (27842 años persona), la incidencia acumulada de T2D fue de 14.4 y 13.7 por 1000 años persona en hombres y mujeres, respectivamente. En evaluaciones intermedias de (1994, 1998 y 2008) fue de 15.8, 15.7 y 12.7 por 1 000 años persona, respectivamente. Los casos prevalentes tuvieron edad promedio al diagnóstico de 44 años; los incidentes de 56 años.
Conclusiones. Esta es la primera estimación a largo plazo de la incidencia de T2D en población mexicana. Los resultados se encuentran entre los más altos informados en el mundo.
Palabras clave: diabetes mellitus; incidencia; población urbana.
There is national consensus that type 2 diabetes (T2D) is a public health problem of the highest priority for Mexico. This is due to its high prevalence (14% of total adults), its morbidity and mortality. These facts are reflected in significant human and economic costs. In addition, there is an ominous future since the proportion of the elderly in Mexico is growing significantly and T2D in this age group occurs in 25-30% of cases.1-5
National health surveys suggest increments in the prevalence of T2D throughout the past three decades. If this is true, it could be the result of several factors, one of which might be that the increase in prevalence is the result of an increment in the incidence of T2D. Hence, to characterize appropriately the nature of the epidemic it is important to have estimates of the incidence of this pathologic condition. In the United States the estimated costs attributable to T2D were 245 billions in 2012, 41% higher than the previous calculation. In Mexico costs associated to T2D care are alarmingly (high and will increase). There is a need for evidence based scientific information that will be useful in the elaboration of an appropriate strategy in the construction of public policy. This is another area in which the estimation of the incidence of T2D will be of value.6,7
There is published information demonstrating that the prevention of T2D is possible.8-10 A baseline estimate of the incidence of T2D will aid in the evaluation of the potential effects of preventive strategies.
Incidence of T2D will be an important information to estimate the efficacy of interventions designed to diminish the prevalence of overweight and obesity. This is another area where information of the incidence of T2D might be of use.11,12 This prospective clinical investigation reports, for the first time in Mexican population, the cumulative incidence of T2D over 18 years of follow-up, in a low income adult urban population.
Materials and methods
The Mexico City Diabetes Study (MCDS) is a population based, prospective investigation that was designed to estimate the prevalence, incidence and natural history of T2D and cardiovascular risk factors, in low income urban adults residing in Mexico City. The study began in 1989 with the identification of a homogeneous low income site. This was located in the delegación (borough) Álvaro Obregón. It encompasses six census tracts (áreas geoestadísticas básicas) defined by the Instituto Nacional de Geografía y Estadística. The following neighborhoods were included: Francisco Villa, Molino de Santo Domingo, Unidad Habitacional Molino de Santo Domingo, Liberales de 1857, Lomas de Santo Domingo and Real del Monte. After a complete household enumeration and comprehensive census of the entire population permanently living in the area (15532 inhabitants), we established that the eligibility criteria would be all men and non pregnant women, 35-64 years of age.
Community centers, worship places, schools, meeting sites and opinion leaders were visited in order to achieve the best response rates to the invitation to participate in the study. Efforts were made to maintain a high level of community trust in the trained personnel at the field and in the staff that conducted the interviews and examinations.
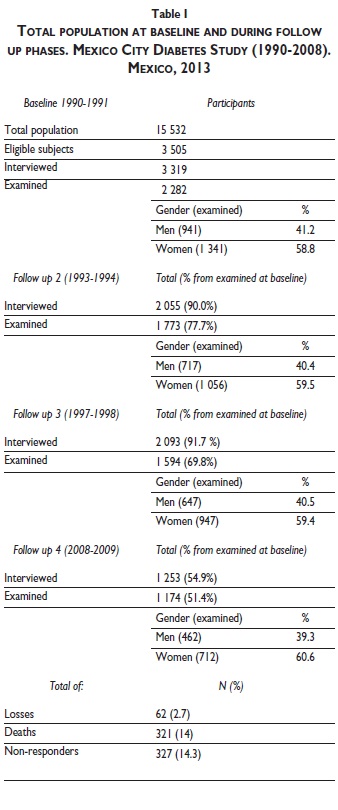
At baseline (1989-1990), a total of 3319 subjects were interviewed and 2282 examined (from a total of 3505 eligible individuals). The final cohort was composed of 941 men and 1 341 women. We identified a total of 343 (15%) subjects with prevalent diagnosis of T2D, of which 179 (52%) were individuals that self reported they had T2D. We established that in order to consider them truly as patients with T2D, they must have been diagnosed by a physician and be under pharmacological therapy for diabetes (oral agents and/or insulin therapy), regardless of their glycemic values. In 164 (48% of prevalent cases) we diagnosed T2D as a result of the survey. These subjects were unaware of their diabetic condition. Therefore the population at risk was 1 939 non-diabetic participants. In the second follow-up, approximately four years later, 2055 from the original cohort were interviewed and 1773 participants were examined (717 men, 1056 women). A third follow-up, performed also approximately four years latter, included 2093 interviewed and 1594 examined individuals (647 men, 947 women). The fourth follow-up, performed during 2008, included 1253 participants that were interviewed and 1174 examined (462 men, 712 women).
Home interviews were attempted in all eligible subjects. The questionnaire contained items to determine the presence of previously diagnosed T2D, and of cardiovascular risk factors, such as: overweight, obesity, hyperlipidemia, hypertension, tobacco use, physical activity, diet and self-care.
After the home interview, participants were invited to a clinical and laboratory examination. All subjects were asked to arrive to the clinic with 12 hours of fasting prior to the exam. Informed consent was obtained from all participants in accordance with the ethical principles for medical research involving human subjects. The institutional review boards of the Centro de Estudios en Diabetes and the Instituto Nacional de Salud Pública approved the protocol.
Each evaluation was performed in a standardized manner; participants were examined in a disposable gown and no shoes. Anthropometry included: height, weight, waist and hip circumferences, tricipital and sub-scapular skin folds. Blood pressure (BP) was measured three times, using a calibrated random zero sphygmomanometer, in the sitting position after 5 min of rest, the mean of the last two readings was used.13 In all phases of the study, an oral glucose tolerance test, using 75 gr of glucose load was performed, fasting and 2 hours insulin, and lipids profile were obtained.
The laboratory used standardized protocols to measure metabolic variables. The results of the clinical and laboratory evaluation with medical interpretation and recommendations were delivered to every participant. International diagnostic criteria were applied. T2D was defined as the American Diabetes Association recommends:14 Fasting glucose ≥126 mg/dl, and/or 2 hours glucose ≥ 200 mg/dl or when a participant self reported having been diagnosed by a physician and was on medication for type 2 diabetes, regardless of the blood glucose found in the laboratory result.
When a participant was found to be deceased and the death certificate stated that he or she was diagnosed as T2D and we had not previously diagnosed him or her we accepted the diagnosis.
Hypertension was diagnosed using the Joint National Commission on Detection and Evaluation of Hypertension (JNC VII) diagnostic criteria.15 Participants who self-reported having been diagnosed by a physician as hypertensive and were taking antihypertensive medications were considered hypertensive, regardless of the blood pressure value obtained. Every effort was made to obtain an interview with questionnaires, physical examination and laboratory tests.
Subjects were classified as home interview non-responders, when the individual declined to give the home interview despite several attempts in which our trained personnel approached him or her because eligibility status. As clinic examination non-responders when, having accepted the home interview the participant refused to accept the examination in the initial evaluation, or sometime in the follow-up phases.
During every phase of the study, efforts were made to determine the vital status of all study subjects, (even non responders). In all the deceased subjects, we tried to obtain a death certificate. When this was not possible we attempted a formal "verbal autopsy", as a surrogate of the death certificate.
The estimation of person-years was made by the contribution of time in the study of all participants, even those who refused at some point to continue in the investigation. We consider that the amount of time contributed by each person that refused to continue ended at the time they expressed that decision. Participants who died contributed with time until the date of death, stated in the death certificate, or informed by family members.
Age at diagnosis was estimated as follows: If the participant accurately defined date of diagnosis (day, month and year) we took this as such, day 30 was considered when they knew month and year but not the exact day, June 30 was considered if they only remembered the year. If the participant was diagnosed at the exam, this date was considered as date of diagnosis.
Statistical analysis was performed using STATA 11.0 package.* It consisted on descriptive statistics, estimation of every numeric variable, considering mean and standard deviation by gender and age group. Variables were analyzed with parametric and non-parametric tests depending on their distribution.
Results
Table I shows the results of the response rates observed throughout the study period by gender. The participation rate decreased progressively due to losses (n=62, 2.7%), deaths (n=321, 14%) or clinic non-responders (n=327, 14.3%).
A total of 732 cases of T2D were identified (32% of the entire study population). Of the 343 participants with T2D (15%) found at baseline, 179 were self reported subjects and were significantly older (53.6 vs 50.1, p<.05), less obese (BMI 28 vs 30, p<.05) and had shorter waist circumference (98 vs 103, p=.06) compared to the individuals that were also prevalent cases, but were identified as T2D as a result of the survey.
Table II shows, by gender, the estimated cumulative incidence of T2D for the total study period. The incidence for the intermediate stages of our investigation is shown. The number of incident cases was 389 (17% of the total study population), 164 men and 225 women. The study period (1990-2008), encompassed 27842 person-years. Cumulative incidence was 14.4 and 13.7 by 1000 person-years for men and women, respectively. The incidence per follow-up phase was 15.8 (1990-1994), 15.7 (1994-1998) and 12.7 (1998-2008), by 1000 person-years respectively.

All incident cases were diagnosed by oral glucose tolerance test except for 12 individuals in which T2D was diagnosed by death certificate (3.08% of the incident cases). Verbal autopsy was performed but we did not identified cases of T2D with this instrument.
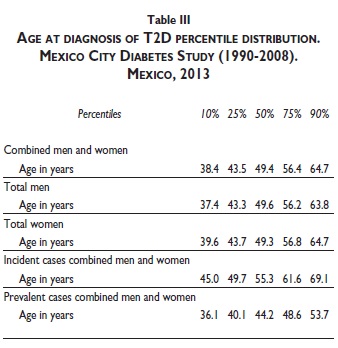
The age at diagnosis frequency histogram for the entire population is shown in figure 1(A). It suggests two modes, figure 1 (B, C) shows the frequency distribution of age at diagnosis, by diagnostic status (prevalent or incident, respectively). The mean age at diagnosis of subjects classified as prevalent is less than those classified as incident (44.4 vs. 55.9 years, respectively).
At baseline, when subjects entered the study, prevalent cases were significantly older than incident ones (52.3 vs 46.2 years, p<.05) and also had lower BMI (28.8 vs 30.0, p<.05), waist (100.1 vs 101.1, p>.05) and hip circumference (100.1 vs 102.7, p <.05).
Table III represents, in percentiles, the distribution of age at diagnosis of our studied subjects. It shows that 25% of the T2D cases were diagnosed either at or before 43.5 years old. We present a comparison by percentile between incident and prevalent cases. The entire age distribution tends to be younger in prevalent cases. Fifty per cent of incident diabetic subjects received their diagnosis being 10 years older than subjects classified as prevalent at baseline.
In figure 2 we present selected publications in which incidence of T2D is informed, expressed in person-years, and representing several populations and ethnic groups. It is shown from the highest to the lowest reported incidence. We include these publications based on comparable methods. It can be noted that our results occupy the seventh position among the studies selected.16-21
Discussion
This is the first investigation in Mexican population designed to obtain an estimate of the long term incidence of T2D. The data presented demonstrates that a significant proportion of individuals (25% of subjects with T2D) have a clinical presentation at younger ages. This "early onset" T2D has been identified previously and coincides with an estimate of 25% of the entire T2D population.22 The experimental design of the study has to be taken into account in order to interpret the interactions of the concepts of age at diagnosis and age of entry to the study. This is the reason why prevalent cases are older at the entry phase and younger at the age of diagnosis when compared to incident cases.
The fact that we found relatively stable incidence throughout the study, should be taken with caution, because by design, our investigation initiates in a group of subjects in which, though were relatively young, we could have missed an increment in the incidence within the younger of them (less than 35 years of age). The fact that we found a decrement from 15.7 to 12.7 per 1 000 person-years in the last phase of our investigation suggests that the survival of the healthiest, with lesser risk to T2D, might be expressed with lower incidence rates in this age group.
The comparison with the incidences reported in other populations, sheds light in the study of the phenomenon. The highest reported incidence, by person-years, corresponds to Pima indians. These comparisons demonstrate that the Mexican population is situated among the high incidence levels of T2D worldwide16-21 (figure 2).
The group that studies the Pima indian population reported no increment in the incidence of T2D through three follow-up periods. They found the following incidences: 25.3 (1965-1977), 22.9 (1978-1990) and 23.5 (1991-2003) cases per 1 000 person-years respectively.16 Although these incidence rates are considerably higher than those obtained in our study, both investigations coincide in the fact that incidence rates have remained relatively stable throughout the long period of observation. It should be noted that the incidence obtained in our investigation is higher than the reported in non Hispanics whites.23
These findings are even more significant if we consider the results of a study done in a cohort of men followed for 23 years in England. In that investigation the incidence of T2D increased from 2-4 cases to 9-11 cases per 1 000 person-years in the last period of observation. Authors conclude that this increment was due to the increase in weight of the population.24 This should be an alert signal, if we considered the rapid pace at which the obesity epidemic is occurring in Mexico.12,25 Other researchers found that the incidence of T2D was higher in low income subjects compared to high income individuals (20.4 vs 9.2 cases per 1 000 person-years).26 Whereas weight gain and poverty have a promoting effect, inducing higher incidence of T2D, as evidenced by these studies, the Mexican population is at risk of reaching even higher incidence rates.
The limitations of the metric used to estimate the incidence of T2D in any given population (person-years) should be recognized. It assumes a uniform risk throughout the follow-up period. Also, a population-based study with a long follow-up period is susceptible to selection bias. Despite these limitations, this approach is useful and valid for international comparisons and the assessment of the dynamics of the phenomenon.
The evidence from this research provides data of potential use in the development of new strategies of interventions directed to the earliest phases of T2D with focus in the younger age group.
Acknowledgements
The Mexico City Diabetes Study is supported by the grants: RO1HL 24799 from the National Heart, Lung and Blood Institute, USA; Consejo Nacional de Ciencia y Tecnología (2092, M9303, F677-M9407, 251M & 2005-C01- 14502, SALUD 2010-2-151165).
References
1. González-Villalpando C, Stern MP, Villalpando E, Hazuda H, Haffner S, Lisci E. Prevalencia de diabetes mellitus e intolerancia a la glucosa en una población urbana de nivel económico bajo. Rev Invest Clin 1992; 44:321-328. [ Links ]
2. Secretaría de Salud. Encuesta Nacional de Enfermedades Crónicas 1993. México: Secretaría de Salud, 1993. [ Links ]
3. Olaiz-Fernández G, Rojas R, Aguilar Salinas C, Rauda J, Villalpando S. Diabetes mellitus in Mexican adults: Results from the 2000 National Health Survey. Salud Publica Mex 2007; 49:331-337. [ Links ]
4. Villalpando S, Shama-Levy T, Rojas R, Aguilar-Salinas CA. Trends for type 2 diabetes and other cardiovascular risk factors in Mexico from 1993-2006. Salud Publica Mex 2010;52 (suppl 1): S72-S79. [ Links ]
5. Secretaría de Salud. Encuesta Nacional de Salud y Nutrición 2012. [Accessed May 3, 2013] Available at: http://ensanut.insp.mx/informes/ENSANUT2012ResultadosNacionales.pdf [ Links ]
6. González-Villalpando C, Stern MP, Arredondo PB, Martínez DS. The level of control in low income Mexico City diabetics. The Mexico City Diabetes Study. Arch Med Res1994; 25:387-392. [ Links ]
7. González-Villalpando C, López-Ridaura R, Campuzano JC, González-Villalpando ME. The status of diabetes care in Mexican population: Are we making a difference? Results of the National Health and Nutrition Survey 2006. Salud Publica Mex 2010: 52 (suppl 1); S36-S43. [ Links ]
8. Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, et al. Finnish Diabetes Prevention Study Group. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001; 344:1343-1350. [ Links ]
9. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346:393-403. [ Links ]
10. Schulze MB, Manson JE, Ludwig DS, Colditz GA, Stampfer MJ, Willett WC, et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA 2004; 292:927-934. [ Links ]
11. González-Villalpando C, Rivera- Martínez D, Cisneros-Castólo M, González-Villalpando ME, Simón J, Williams K, et al. Seven-year incidence and progression of obesity. Characterization of body fat pattern evolution in low- income Mexico City urban population. Arch Med Res 2003; 34: 348-353. [ Links ]
12. Barquera S, Campos-Nonato I, Hernández-Barrera L, Flores M, Durazo-Arvizu R, Kanter R, et al. Obesity and central adiposity in Mexican adults: results from the Mexican National Health and Nutrition Survey 2006. Salud Publica Mex 2009; 51(suppl 4): S595-S603. [ Links ]
13. González-Villalpando C, Stern MP, Haffner S, González-Villalpando ME, Gaskill S, Rivera MD. Prevalence of hypertension in Mexican population according to the sixth report of the Joint National Committee on Prevention Detection Evaluation and Treatment of High Blood Pressure. J Cardiovasc Risk 1999; 6:177-181. [ Links ]
14. American Diabetes Association. Clinical Practice Recommendations. Diabetes Care 2013; 36: S4-S5. [ Links ]
15. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. JAMA 2003; 289:2560-2571. [ Links ]
16. Pavkov ME, Hanson RL, Knowler WC, Bennet PH, Krakoff J, Nelson RG. Changing patterns of type 2 diabetes incidence among Pima Indians. Diabetes Care 2007; 30: 1758-1763. [ Links ]
17. Karter AJ, Schillinger D, Adams AS, Moffet HH, Liu J, Adler NE, et al. Elevated rates of diabetes in Pacific Islanders and Asian subgroups. Diabetes Care 2013; 36: 574-579. [ Links ]
18. Andersen ZJ, Raaschou-Nielsen O, Ketzel M, Jensen SS, Hvidberg M, Loft S, et al. Diabetes incidence and long-term exposure to air pollution. Diabetes Care 2012; 35: 92-98. [ Links ]
19. Valdés S, Botas P, Delgado E, Alvarez F, Diaz-Cadórniga F. Population-based incidence of type 2 diabetes in Northern Spain. Diabetes Care 2007; 30: 2258-2263. [ Links ]
20. Laclé-Murray A, Valero-Juan LF. Incidencia de diabetes tipo 2 en un área urbano marginal de Costa Rica. AMC 2008; 50: 29-34. [ Links ]
21. Bonora E, Kiechl S, Willeit J, Oberhollenzer F, Egger G, Meigs JB, et al. Population-based incidence rates and risk factors for type 2 diabetes in White individuals The Bruneck Study. Diabetes 2004; 52: 1782-1789. [ Links ]
22. Jiménez-Corona A, Rojas R, Gómez-Pérez FJ, Aguilar-Salinas CA. Early-onset type 2 diabetes in a Mexican survey: Results from the National Health and Nutrition Survey 2006. Salud Publica Mex 2010; 52 (suppl 1):S27-S35. [ Links ]
23. Burke JP, Williams K, Haffner SM, Gonzalez-Villalpando C, Stern MP. Elevated incidence of type 2 Diabetes in San Antonio, Texas, compared with that of Mexico City, Mexico. Diabetes Care 2001; 24: 1573-1578. [ Links ]
24. Hardoon SL, Morris RW, Thomas MC, Wannamethee SG, Lennon LT, Whincup PH. Is the recent rise in type 2 diabetes incidence from 1984 to 2007 explained by the trend in increasing BMI? Diabetes Care 2010; 33: 1494-1496. [ Links ]
25. González-Villalpando C, Stern MP. La obesidad como factor de riesgo cardiovascular en México. Estudio en población abierta. Rev Inv Clin 1993; 45: 13-21. [ Links ]
26. Hsu CC, Lee CH, Wahlqvist ML, Huang HL, Chang HY, Chen L, et al. Poverty increases type 2 diabetes incidences and inequality of care despite universal health coverage. Diabetes Care 2012; 35: 2286-2292. [ Links ]
* StataCorp. Stata Statistical Software: Release 11. Texas: StataCorp LP, College Station; 2009.
Received on: July 17, 2013
Accepted on: October 29, 2013
 Corresponding author:
Corresponding author:
Clicerio González-Villalpando.
Unidad de Investigación en Diabetes y Riesgo Cardiovascular,
Instituto Nacional de Salud Pública. Sur 136 # 116-309, 01120,
México DF. E-mail: cliceriogonzalez@hotmail.com













