Introduction
Transoral laser microsurgery (TLM) is a worldwide, time-honored technique for early laryngeal carcinoma treatment, in the past 35 years, it has been developed and refined. Based on the excellent results for early larynx cancer, it is also being used for cancer treatment of the whole superior aerodigestive tract1.
In the early 70’s, laser microsurgery was first used by Strong and Jako in the United States2; however, several reports from European countries described technical improvements and resection classification types3 and began to publish the first series of patients treated with laser microsurgery4. In America, it was not until 2000 when interesting reports were published from different authors in the United States5-8. In this context, the expansion of TLM took longer to influence Latin America9 where very scant information can be found about its progress and applicability in the region. In 2004, we published in the Mexican medical literature the technique and principles of transoral laser surgery based on the teachings of Dr. Wolfgang Steiner at Georg-August-University in Goettingen, Germany10.
In the present manuscript, we describe the experience in early glottic carcinoma laser microsurgery treatment at a Tertiary Care Hospital in Mexico City.
Materials and methods
Diagnosis and patients selection
The study cohort consisted of a retrospective analysis of patients treated for laryngeal carcinoma with CO2 laser microsurgery between November 2003 and December 2013. Fifty-three consecutive patients with confirmed glottic laryngeal cancer Stage I-II (Tis-T2, N0, M0) according to the 2002 AJCC Cancer Staging Manual11 were selected, only patients without previous treatment (radiotherapy and/or chemotherapy) and with at least 3-year follow-up were included in the study. Information was collected from each of the patients’ hospital records. As a result, 40 patients were included and are the subject of this study.
Laryngeal biopsy for diagnosis was made either by direct laryngoscopy under general anesthesia (in our hospital or elsewhere) or by flexible endoscopy in an office-based setting at our hospital. A few Tis-T1 cases were operated on the basis of an intraoperative diagnosis considering that resection would be a diagnostic and therapeutic procedure. Patients diagnosed with squamous cell carcinoma of glottic localization were considered for this study.
At our hospital, the therapeutic modality for laryngeal carcinoma treatment was discussed with the patient. An explanation was given about different therapeutic modalities: radiotherapy or laser surgery. Second look surgery was not routinely done; only cases of suspicious lesions detected during the follow-up were reoperated. Informed consent was provided by all patients before treatment.
Surgical technique
CO2 laser equipment varied from Sharplan 11000 (Laser Industries Ltd., Tel-Aviv, Israel), Sharplan 10415 (Lumenis, Tel-Aviv, Israel), Surgilase SL 60 Gold (Patlex Corp., Rhode Island, USA), and Sharplan 30C (Lumenis, Yokneam, Israel). Laser power settings used were 3-5 watt in super pulse mode for precise cutting with minimal tissue carbonization, up to 10 w for tumor debulking, and 15 w for cartilage resection. It was coupled to the microscope either with MicroSlad 719 or AcuSpot 712 micromanipulator (Lumenis Inc., California, USA). Instrumentation consisted of Steiner Laser Set (Karl Storz, Tuttlingen, Germany). The technique used for resection was based on Steiner’s state of the art laser manual1. Special laser endotracheal tubes were used whenever possible, but they frequently had to be changed during surgery due to its restricted internal lumen and the obstructive external diameter of the surgical field. In these cases, conventional polyvinyl chloride tubes were used with 5.5-6.5 mm inner diameter protected with moist gauze nasal packing material and with the safety measures described by Ossoff12; Steiner and Ambrosch have used since over 25 years the Mallinckrodt Nellcor (MLT) endotracheal tube (inner diameter 5 mm) with inspiratory O2 under 25%, protected with moist cottonoid, without complications1.
Data analysis
Variables and data collection
Data collected were introduced into a database (Microsoft Office Excel 2010). The studied variables were age, sex, TNM staging, surgery date, post-operative complications, hospital stay days, histology report, distant metastasis, local recurrence, regional recurrence, and years of follow-up. Data were shown as mean±standard deviation (minimum-maximum) for continuous variables, where appropriate. Survival curves (overall survival, disease-specific survival (DSS), local control, and ultimate local control [ULC]) were calculated from the date of the diagnosis by the Kaplan–Meier method. Overall survival was assessed from the date of surgery to the date of death (regardless of the cause) or the date of the last follow-up for censored observations. For the analysis of DSS, patients who died of unrelated causes were considered as censored at the date of death. The endpoint for local control by laser only treatment was the date of recurrence or post-operative decision for additional therapy other than laser surgery. The endpoint for the organ preservation (OP) rate was the date of total laryngectomy.
Results
Forty patients were included in the analysis: 4 pTis (10%), 19 pT1a (47%), 8 pT1b (20%), and 9 pT2 (23%). There were 36 male and 4 female patients, the mean patient’s age was 67 years (range 39-82). Mean patient follow-up time was 7.4 years (range 3-12.9 years). The average post-operative hospital stay was 2.75 days (0-15 days). Only 1 patient (2.5%) presented bleeding as a post-operative major complication, in his 2nd post-operative day, that required urgent revision surgery with prophylactic tracheotomy and had the longest hospital stay (15 days) (Table 1).
Table 1 Patient characteristics
| Variable | Tis (n = 4) | T1a (n = 19) | T1b (n = 8) | T2 (n = 9) | Total (n = 40) |
|---|---|---|---|---|---|
| Male/Female | 4 | 15/4 | 8 | 9 | 36/4 |
| Mean age | 67 | 68 | 65 | 67 | 67years |
| Recurrence | 0 | 2 | 1 | 1 | 4 |
| Post-operative bleeding | 0 | 0 | 0 | 1 | 1 |
| Hospital stay (mean days) | 1 | 1.8 | 2.5 | 5.8 | 2.7days |
Recurrence occurred in 4 patients (10%), one of them did not receive additional treatment because it had no implication in his quality of life, he died of non-related cancer cause. Another patient had revision TLM with adequate local control; however, he developed a second primary in the lung during his 5th year of laryngeal carcinoma follow-up for which he received chemotherapy, he is alive without disease. The third patient had a local recurrence at his 5th follow-up year, he received radiotherapy and is alive without disease. Finally, the fourth patient with recurrence was treated with total laryngectomy and chemoradiotherapy; unfortunately, he died with locoregional disease.
Twenty-nine patients (72.5%) are alive without disease, nine patients (22.5%) died disease-free of non-cancer-related causes, 1 patient (2.5%) died with disease of non-cancer-related cause, and another one (2.5%) died of the disease (Fig. 1).

Figure 1 Survival status. AWOD: alive without disease; DWOD: dead without disease; DWDCR: dead with disease cancer-related cause; DWDCNR: dead with disease cancer not related cause.
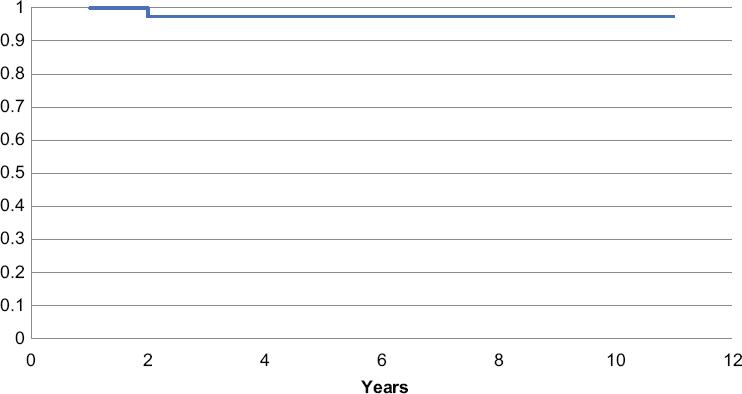
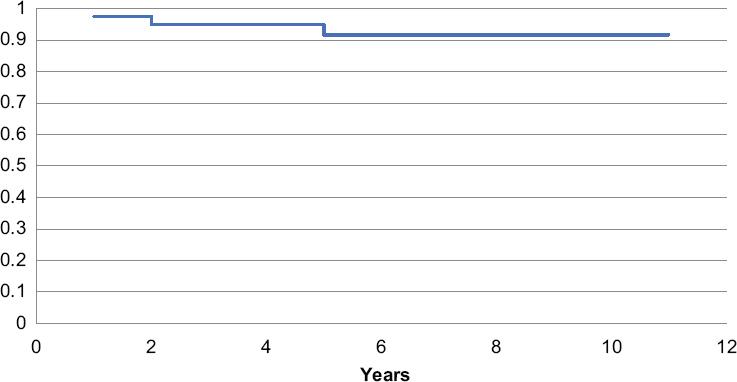
In our cohort, the Kaplan–Meier results at 3 and 5-year estimates were as follows: overall survival (OAS) was 92.5% and 87%, respectively; laser only local control (LLC) was 94.9 and 91.6%, respectively; and DSS and ULC rate were 97.5% for both time periods (Figs. 2-5). We found a 97.5% (39/40) OP rate.
Discussion
Medical technologic advances take some time to be established as “standard” therapeutic modalities. They must prove their efficacy at the site of conception to convince colleagues of its applications. Sometimes the technique also defies the so-called “unbreakable” principles of medicine and skepticism keeps it on the shelf for more time than expected, as in oncological endoscopic laser microsurgery. This type of surgery requires Hi-Tec equipment and costs may also seem a limitation to the low-income countries. All the latter have delayed laser microsurgery as being considered a reasonable treatment option for laryngeal carcinoma in Mexico.
Our institution is a public, general, and teaching hospital in Mexico City which offers laser microsurgery as a standard modality for laryngeal carcinoma treatment. Through all these years, we have learned that to perform successfully this procedure, training, equipment, technique, and close patient follow-up are very important and need to be taken seriously by surgeons who are willing to perform this technique.
The special parameters of laser beam manipulation (continuous wave, pulsed, super pulsed/continuous, single pulse, and repeated pulse) will interact differently with tissue to acquire the desired results. One principle of laser microsurgery is the ability to recognize tumor limits and invasion according to the degree of carbonization during laser cutting1, so excessive carbonization is not desired using high laser output.
Since laser microsurgery conception, surgeons have made efforts to implement classifications to compare results of laryngeal laser resections3-5,13-15, as with its external approach counterpart. However, we found them difficult to apply to our patients, as laser microsurgery is a self-tailored technique, in which there are as many variations as patients treated. We followed the principles of resection described by Steiner and Ambrosch1.
Even though bleeding is the most common complication reported by other authors16, it has a very low presentation rate. In the present study, 1 patient (2.5%) presented this complication on the 2nd post-operative day, Ellies and Steiner17 report a 1.4% and Vilaseca-González18 a 2.9% bleeding rate for glottic resections; they consider that the extension of resection and the surgeon experience are important factors leading to this complication16,18. Our patient was one of our first transoral laser surgery cases, we performed a revision surgery for hemostatic control and a temporary prophylactic tracheotomy. We consider that our learning curve and better instrumentation (hemostatic laryngeal surgery alligator forceps) helped to prevent further bleeding events in our patients and we would not consider making prophylactic tracheotomy now in the same clinical situation.
In our study, the 5-year overall survival rate was 87%, which is similar to that reported by Pradhan19 (84.1%) and Huang20 (89.4%). The 5-year DSS rate in our series was 97.5%, similar to reports from other authors such as Eckel21 and Moreau13 (97%).
OP rate has been reported by Eckel21, Ledda22, Schrijvers23, Grant24, Ambrosh25, and Ellies and Steiner17 from 89% to 100%, whereas we achieved an OP rate of 97.5%.
The 5-year laser alone local control of our cohort was 91.6% while it has been reported in 93% in different series14,20,21, our 5-year ULC was 97.5%, where as we found a 98.7%14,20,21,25,26 reported in the literature. Fortunately, we gladly found that our results are similar as other experienced authors have reported24,27,28 (Table 2).
Table 2 Comparative results
| Author | OAS % | DSS % | LLC % | OP % |
|---|---|---|---|---|
| Present study | 87 | 97.5 | 91.6 | 97.5 |
| Lee27 | 92.2 | 99 | 94.2 | 96.2 |
| Pearson28 | 93 | 91 | 91 | 95 |
| Canis29 | 88 | 98 | 86.6 | - |
| Stoeckli29 | 85 | 96 | 86 | 96 |
| Spector29 | 84 | 95 | 77 | 90 |
| Mahler29 | 78 | 98 | 92 | 99 |
DSS: disease-specific survival; LLC: laser local control; OAS: overall survival; OP: organ preservation.
It is important to mention that multiple efforts have been made to compare oncologic and functional results between endoscopic laser microsurgery and radiotherapy, but this has been difficult because randomized controlled multicenter studies are not yet available29. Taken these in mind, the oncologic results for TLM tend to be better than with radiotherapy (RT) at 5-year estimates30,31; TLM versus RT: LC 85% versus 82%, OAS 84% versus 75%, DSS 94% versus 87%, and OP 89% versus 79%. Regarding open partial laryngectomy (OPL), this technique has higher morbidity and longer recovery time than TLM. However, as it is a more “radical” procedure, the oncologic results have been reported better than it is endoscopic counterpart30; OPL versus TLM: LC 96% versus 85% and OS 89% versus 84%.
Conclusion
Endoscopic laser microsurgery for the treatment of early glottic carcinoma has proved adequate oncological results since its conception and has gathered more than 35 years of experience around the world. Fortunately, we were also able to reproduce the technique and results reported by diverse authors in Europe and in the United States of America following the step-by-step principles described and developed by Dr. Wolfgang Steiner. It is important to say that proper training with adequate surgical equipment and instrumentation is mandatory to achieve this goal.
Due to our results, we consider that laser microsurgery could be performed in other institutions in our country.











 nova página do texto(beta)
nova página do texto(beta)