Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista odontológica mexicana
versão impressa ISSN 1870-199X
Rev. Odont. Mex vol.17 no.1 Ciudad de México Jan./Mar. 2013
Original research
Pre-condylar stop: surgical alternative for the treatment of mandibular chronic luxation. Modification of Norman Technique. Experience with 12 patients
Jesús Quiroz Navarro,* Ma. Iliana Picco Díaz,§ Jorge Ramírez Melgoza,II Sonia Cruz Paz¶
* Physician attached to the Maxillofacial Surgery Service. Regional Hospital 1 o de Octubre, ISSSTE, HGZ 57, IMSS and UNAM Professor.
§ Professor, Maxillofacial Surgery Course, Regional Hospital 1 o de Octubre, ISSSTE.
II Physician attached to the Maxillofacial Surgery Service, Regional Hospital 1 o de Octubre, ISSSTE.
¶ Private Practice Orthodontist, University Graduate, National School of Dentistry, National University of Mexico (UNAM).
ABSTRACT
Aim: The aim of the present article was to describe use of chin bone graft to increase articular eminence as preferred treatment for mandibular chronic luxation. Patients and methods: The present study was undertaken with 12 patients, average age 44 years. Patients had been diagnosed as suffering from chronic mandibular luxation (dislocation), with pain symptomatology rating 8 or more in the Analogous Visual Scale (AVS). Patients had experienced an average 1.5 year evolution and 55 mm or more oral opening. Patients had been conservatively treated for at least three months, with no visible improvement. Patients were then treated following a modified Norman technique, in which an articular eminence augmentation is performed with a chin bone graft placed through pre-auricular approach. Results: None of the patients presented new dislocation events during the 18 month follow up period after surgery. Conclusions: The present study showed the fact that mandibular chronic dislocation correction with placement of pre-condylar stop with chin bone graft is an effective and safe technique.
Key words: Chronic jaw dislocation, augmentation of articular eminence.
INTRODUCTION
Mandibular luxation is a complete dislocation of condylar and temporal articular surfaces.1 It can be due to a spasm of the external pterygoid muscle or to the over-rotation of the condyle.2 Ligaments do not actively participate in TMJ (temporomandibular joint) functions; they restrict articulation movements, mechanically as well as through neuromuscular reflex activity. Ligaments do not stretch, but when subjected to traction they can elongate, thus increasing their length, and giving rise to the possibility of compromising the articulation's normal functioning. TMJ articular surfaces must be kept in constant contact. This is achieved by muscles which bring the articulation from one side to the other (elevator muscles: temporal, masseter and internal pterigoyd muscles).3
A normal oral opening should be within a 40 to 55 mm range.4 TMJ dislocation is not very common when compared with dislocations of other articulations. Incidence of TMJ dislocations is about 3%, and is present more in females than in males.5 There is confusion with respect to terminology pertaining mandibular dislocations. The term hyper-mobility, literally means ''excessive mobility''.
HYPER-MOBILITY CAN BE DIVIDED INTO THREE INTER-RELATED CLINICAL ENTITIES
Hyper-translation refers to movements of the condyle in front and above the articular eminence during the opening of the mouth. This is probably a normal state for many individuals.6,7
Subluxation represents an incomplete dislocation of the condyle, where articular surfaces preserve partial contact. At maximum opening, the condyle moves anteriorly towards the articular eminence, and is able to re-take the fossa either through manipulation or spontaneous reduction.8
Spontaneous dislocation (blocked opening) seems to be the final stage of TMJ hyper-mobility development. This takes place when the condyle moves towards an anterior position with respect to the articular eminence. This position cannot be voluntarily reduced.9-11
Dislocations repeatedly occurring at long or short intervals are referred to as recurrent dislocations. A dislocation which remains locked for days or even years is considered a long-standing dislocation.
TMJ dislocations, occurring as result of protrusive muscles tone increase have recently been referred to as TMJ neurogenic dislocations.8
MOBILITY PREDISPOSING FACTORS
• Lax ligaments (constitutional hypermobility): This is a physiological variety which, under given circumstances, can generate pathogenic consequences. Hypermobility is frequently associated to weakness, muscle discoordination, or incapacity to create healthy movement stereotypes. An increase in estrogen levels takes place. This fact probably explains why lax ligaments are more common in women.12
• Condyle and eminence morphological circumstances: Patients afflicted with TMJ hypermobility with flat articular eminence area are able to easily retake the dislocated condyle. In the case of a very steep dislocation, re-positioning becomes very difficult, increasing thus the risk of bi-laminar area over-extension.13
• Degenerative diseases of the articulation: these produce morphological changes in ligaments, condyles and fovea.
• Un-synchronized muscle function: This is the result of an alteration of the normal contraction sequence of pro-tractor and elevator muscles of the lower jaw. Condylar protrusive muscles bring about a more inferior-anterior position with respect to the articular eminence in opening position; In a similar fashion, elevator muscles contract, thus dislocating the mandible inside the temporal fossa.8,5
Approximately 8,000 appointments are made at the out-patient service of the Maxillofacial Surgery Department, Regional Hospital 1o de Octubre. 50% of these are assigned to patients afflicted with TMJ (temporomandibular joint) alterations of varied nature and severity. 3% of our population present chronic mandibular dislocation; they require effective alternatives identified by a suitable diagnosis to solve the specific problems. Therefore, the present study proposes the following: the articular eminence increase technique through the placement of a graft with pre-auricular approach is a safe technique providing optimal results in the correction of mandibular chronic dislocation in patients who previously had unsuccessfully been subjected to conservative treatment.
PATIENTS AND METHODS
The present study was undertaken at the 1o de Octubre ISSSTE Regional Hospital. In 2006, 12 patients underwent surgery, one male and 11 female. Age rank was from 35 to 52 years, average age was 44 years. After clinical and radiographic examination, emitted diagnosis on patients (linear tomography) was the following: mandibular chronic dislocations (at least three previous events) with pain symptomatology equal to or above 8 in the Analogous Visual Scale (AVS). Evolution was in average 1.5 years.1-3 Oral opening was 55 mm or more. Patients had been conventionally treated, for at least three months previously, with muscle re-programming exercises, physical therapy, placement of class III elastics, application of botulinum toxin in external pterygoid muscle. All the aforementioned methods proved to be unsuccessful (Table I).

SURGICAL TECHNIQUE
Patients were previously assessed by the anesthesiology service in order to preclude any type of contraindication pertaining to the anesthetic procedure. Patients were admitted in the hospital on surgery day.
Endotracheal intubation was established. A graft from the symphysis menti was first harvested conducting intra-oral approach in the anterior section of the mandible. Incision was placed at 5 mm underneath the muco-gingival insertion, from canine to canine, exposing thus the bony tissue of the symphysis. With a bur, an approximately 10 mm per side square was traced, reaching, in depth, cancellous bone (Figure 1). A 45° inclination was given to the osteotomy border, on all sides. With a fine, curved chisel, the graft was harvested. The graft was then immersed in saline solution. Hemostatic measures were undertaken with wax on the surgical bed. Oral mucosa was sutured with Vycril 3-0 (Figure 2).


Once asepsis and antisepsis of pre-auricular area were achieved (Figure 3), pre-auricular approach was undertaken, incising skin and subcutaneous cellular tissue, until reaching the temporalis superficial fascia. Palpation was performed on the zygomatic arch, an incision was then executed at 45° with respect to the arch, to free the temporal-frontal ramus from the facial nerve (Figure 4). Careful dissection of the superficial fascia and capsule was undertaken, until uncovering the glenoid cavity, articular eminence and one third of the zygomatic arch (Figure 5).



At a later point in time, the oblique osteotomy was traced from the zygomatic arch crossing the articular eminence. With a fine chisel a jagged fracture was performed on the ramus and the descent of the lower part of the eminence (Figure 6). The graft was given a wedge shape and was interposed between both osteotomized fragments. (Figure 7). The graft was later secured with a three orifice plate and 2 x 5 mm screws. One screw was placed on the lower section of the eminence, another screw was placed in the graft, and the last one in the upper section of the eminence (Figure 8). Once the graft was fixated, suture by planes was undertaken, and the surgery was deemed completed.



The patient was recalled for follow up visits once a week for a month, then he was recalled every month for six months, then 12 months later and finally, 18 months after that. With the help of linear tomography oral opening (Figure 9) and condyle translation within the glenoid fossa were assessed (Figure 10). Abnormal articular noise and pain symptoms were also assessed to later analyze this data along with pre-surgical data.


STATISTICS
Statistical frequency measurements with central tendency and association measurements.
RESULTS
Initial oral opening (average 55.2 mm) was compared with openings at 6, 12, and 18 months, which were in average 33.1, 37.5 and 40.3 mm respectively (Table II). Significant and gradual improvement could be observed with the passing of time.

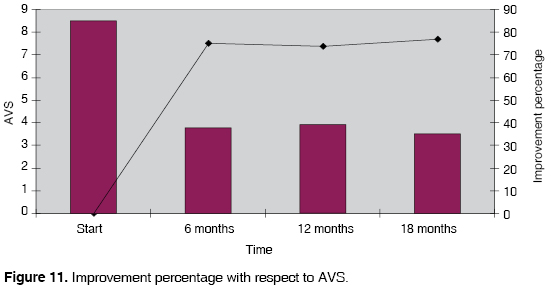
Pain symptoms were assessed on a 1 to 10 scale (Analogous Visual Scale). Where 10 would be the highest degree of pain and 1 absence of pain. Initially, patients exhibited an 8.5 AVS average rating. 18 months after procedure a significant improvement could be observed; patients then exhibited a 3.5 rank in the AVS scale (Table III).

With respect to symptomatology frequency in post-surgical period, 9 patients (75%) informed experiencing symptoms occasionally, whereas only 3 patients (25%) informed experiencing constant symptoms. Out of the 9 patients reporting occasional symptomatology, 5 (55%) referred it was mainly associated to the process of chewing.
In order to assess symptom improvement based on AVS when compared to symptoms exhibited before the surgery, the following was defined: excellent result was achieved when AVS ranked between 1 and 3, good results were achieved when AVS ranked between 4 and 6, same results were achieved when AVS ranked between 7 and 9, and worse results were obtained when AVS rated 10. 7 patients (59%) rated excellent results; 4 patients (33%) rated good results, and only 1 patient (8%) did not experience changes. None of the patients rated a higher AVS rank after surgery when compared to their initial rank (Table IV).

Before surgery, all patients exhibited articular noises; after surgery only 50% of all patients exhibited some articular noise.
Based on obtained results, and based on Analogous Visual Scale, we could reach the conclusion that there was improvement in 77% of cases after 18 months, when compared to pain symptoms referred before surgery (Figure 11).
DISCUSSION
There are different techniques used to correct chronic dislocation of the mandible. These include surgical and non-surgical procedures. Sclerosing solutions14,15 have been used to produce fibrosis within the articulation and thus limit condylar movements. Muscle re-education exercises, physical therapy as well as TMJ ultrasound have equally been used.16 Traction with class III elastics for a two week period is a useful procedure to achieve total reduction. Simple maxillary-mandibular fixation (MMF) for a few days is insufficient to be considered appropriate treatment, since significant reduction of the internal pterigoyd muscle fibers is established after 72 hours of immobilization.17 The aforementioned techniques have short term effects; for this reason they have been discarded.
Within the scope of surgical techniques, procedures on capsule, mandibular condyle, articular eminence, meniscus, myotomy , myectomy and cygomatic arch have been performed.14,15,18-20
The most commonly used surgical procedures are cygomatic arch split fracture and articular eminence bone graft. Norman's surgical technique described in 1984 on 350 patients is one of the most accepted techniques. In the aforementioned technique, the glenoid-temporal osteotomy is conducted through a temporal- facial incision. Dissection is performed through the length of the cygomatic arch at a sub-periosteal level. Separation of the temporal muscle with electric scalpel allows wide exposition of the temporal muscle squama and a relaxed anterior dissection lacking facial nerve traction. The temporomandibular lateral ligament and the articular capsule are separated from the lateral margin of the mandibular fossa and the articular eminence, in such a way that an oblique osteotomy from the zygoma root and the eminence is performed. The osteotomy on the fossa is placed close to the petrotympanic fissure, and its medial extension is determined by a vertical cut (eminotomy) which starts through the temporalis fossa and is completed through the mandibular fossa. Upon completion of osteotomy, the bone is raggedly fractured, with a gently cleaving motion. The resultant dehiscence is filled with a plug-shaped wedge-shaped graft previously harvested from the iliac crest of the mastoid region.
The surgeon must strive to achieve 8 to 10 mm height above the 50% of the eminence width. The graft is fixated with the help of wire osteo-synthesis. If proper graft width is not achieved, the mandibular condye could escape medially and new dislocation episodes might take place. At a later point articular capsule reconstruction is undertaken and the wound is sutured by planes.21-24
In the present study, a pre-auricular approach, in the shape of seagull wings, was undertaken. This technique avoids damaging the auricular-temporal branch of the facial nerve. Upon arriving to the fascia of the temporal muscle, it is imperative to perform a 45° incision above it, so as to be able to reflect temporal and frontal branches of the facial nerve and avoid inflicting lesions on them, which would later cause paresthesia. When following this approach, proper vision of bone structures where osteotomy is to be performed is achieved, as well as the ragged fracture , where, at a later point, the graft is going to be lodged. This technique also offers a more aesthetic and less invasive approach.
The graft is harvested intra-orally, from the symphysis menti. This allows for lesser surgical time and patient morbidity, since it doesn't affect the iliac crest, thus avoiding possible complications such as temporary disability. Post-operative disability period is also decreased allowing the patient to resume normal daily activities. Scarring and incisions in the patient are also avoided, circumventing thus aesthetic discomfort. The graft harvested from the symphysis menti must be immersed in saline solution to produce a basic pH change. Bacteria found in the intraoral area are thus eliminated and post-surgical infection is avoided.
Graft fixation with titanium miniplates and screws permits a rigid graft unable to extrude or move. This avoids possible surgical failure precluding condylar exit through medial section of the osteotomy.
During surgical procedure, instruments used within the mouth to harvest the symphysis menti graft, must be clearly separated from instruments used on the TMJ, to avoid contamination and possible post-surgical infection.
MAIN MODIFICATIONS TO NORMAN TECHNIQUE
1. Pre-atrial (pre-auricular) approach. The suitable point of the ear is located, it slides downward very close to the auricular cartilage until reaching the lowest point of the earlobe, giving the appearance of a seagull wing.
2. The graft is harvested from within the mouth from the symphysis menti.
3. Fixation of the graft is achieved with titanium mini-plates and screws.
CONCLUSIONS
We have found that correction of mandiular chronic dislocation with the placement of pre-condylar stop with chin graft is an efficient and safe technique, in which we achieved an improvement of 75 to 77% in 90% of all patients.
REFERENCES
1. Buenecha-Imaz R, Gay EC. Cirugía funcional de la articulación temporomandibular. Odontología 1995; 3: 27-45. [ Links ]
2. Bell WE. Temporomandibular disorders . 3rd ed. Chicago: Year Book Medical Publishers, 1990. [ Links ]
3. Burch I. Activity of was accessory ligaments of the temporomandibular joint. L Prosthet Dent 1970; 24 (6): 621-628. [ Links ]
4. McCarthy WL. Internal derangements of the temporomandibular joint. Surgery of the temporomandibular joint. Blackwell Scientific Publications 1988; s. 271-289. [ Links ]
5. Merrill RG. Mandibular dislocation. Surgery of the temporomandibular joint. Blackwell Scientific Publications 1988; s. 271-289. [ Links ]
6. Boering C, Citován V, Kieth DA. Surgery of the temporomandibular joint. Boston: Blackwell Scientific Press 1988; s.137. [ Links ]
7. Undt G, Kermer C, Piehslinger E, Rasse M. Treatment of recurrent mandibular dislocation. Part I Leclerc blocking procedure. Int Oral Surg 1997; 26: 92-97. [ Links ]
8. Okeson lP. Management of temporomandibu1ar disorders and occlusion. 3ra. Ed. Sto Louis (MI): Mosby Year; 1993. [ Links ]
9. Oatis G, Baker D. The bilateral erninectomy as definitive treatment. J Oral Surg 1984: 294-298. [ Links ]
10. Myrhaug H. A new method of operation for habitual dislocation of the mandible: review of former method of treatment. Acta Odontol Scand 1951; 9: 247-261. [ Links ]
11. Dingman RO, Moorman W. Meniscectomy in the treatment of lesions of the temporomandibular joint. J Oral Surg 1951; 9: 214-224. [ Links ]
12. Bates R, Stewart C, Atkinson W. The relationship between internal derangements of the temporomandibular joint and systemic joint laxity. J Am Dent Assoc 1984; 109 (3): 446-447. [ Links ]
13. Dijkstra PU. Temporomandibular joint: Osteoarthrosis and joint mobility. Rijksuniversiteit Groningen, dissertation thesis, Groningen 1993. [ Links ]
14. Georgiade N. The surgical correction of chronic luxation of the mandibular condyle. Plast Reconstruct Surg 1965; 36: 339-342. [ Links ]
15. Gosserez M, Dautrey J. Osteoplastic bearing for the treatment of temporomandibular joint luxatios. Oral Surg IV Trans Congr Int Assoc Oral Surg Copenhagen 1967: 261-264. [ Links ]
16. Westling L. Craniomandibular disorders and general joint mobility. Acta Odontol Scand 1989; 47 (5): 293-299. [ Links ]
17. Israel HA. Current concepts in the surgical management of temporomandibular joint disorders. J Oral Surg 1995; 5: 202-207. [ Links ]
18. Köle H. Dermis flap transportation as a treatment for fixed dislocation of the temporomandibular joint. J Maxillofac Surg 1981; 9: 129-131. [ Links ]
19. Laskin DM. Myotomy for the management of recurrent and protracted mandibular dislocations. Trans Cong Int Assoc Oral Surg 1973; 4: 264-268. [ Links ]
20. Mac. Farlane WI. Recurrent dislocation of the mandible: treatment of 7 cases by simple surgical method. Br J Oral Surg 1977; 14: 227-229. [ Links ]
21. Norman JE de B. Postraumatic disorders of the temporomandibular joint. An Royal Coll Surg Engl 1982; 64: 29-36. [ Links ]
22. Norman JE de B. Recurrent dislocation of temporomandibular joint. Gleno-temporal osteotomy and a modified dowel grafo. European Assoc. For Maxillofac. Surg. 7th. Congreso 1984, Abstracts, 97. [ Links ]
23. Norman JE de B. Technique of Surgery of the mandibular joint. Aus Dent J 1975; 20: 174-175. [ Links ]
24. Norman J, Bramley P. Libro de texto y atlas de la articulación temporomandibular: Enfermedades alteraciones cirugía . 1993: 136-150. [ Links ]
LECTURAS RECOMENDADAS
• Okeson JP. Tratamiento de la oclusión y las afecciones temporomandibulares . 4th ed. Madrid: Harcourt, 1999. [ Links ]
• Gay-Escoda C. Eminectomy associated with redirectioning of the temporal muscle for treatment of recurrent TMJ dislocation. J Cranio Maxillofac Surg 1987; 15: 355-358. [ Links ]
• Wolford DMD, Pitta DDS. Mitek anchors for treatment of chronic mandibular dislocation. Oral Med Oral Pathol Oral Radio Endo 2001; 92: 495-498. [ Links ]
Note This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam Mailing address:
Mailing address:
Jesús Quiroz Navarro
E-mail: jesuscmf@hotmail.com











 texto em
texto em 


