Introduction
Cardiovascular disease (CVD), particularly ischemic heart disease (IHD), continues to be one of the leading causes of mortality in America1. In the past two decades, it has been reported that the prevalence, incidence, and mortality rates attributable to CVD have decreased in the United States and Canada2,3. Nevertheless, in developing countries like Mexico, CVD and IHD have increased in prevalence and mortality within the same time period4. A potential explanation for the increase in these epidemiological trends has been associated with a rise in the burden of well-identified traditional risk factors, particularly diabetes, arterial hypertension, and obesity5. According to the 2016 National Health and Nutrition Survey, a growth in the prevalence of these three traditional risk factors was reported in Mexico's growing urban cities6. Moreover, the impact has been translated at an individual care level, where the high prevalence of chronic health comorbidities is also combined with a diverse clinical cardiac-related symptoms at the moment of medical evaluation7. Both traditional risk factors and cardiac symptoms are related to cardiovascular impairments that had been previously described8,9.
Imaging methods are essential to stratify, identify, and give an appropriate treatment for the underlying myocardial impairments10. An optimal approach for the clinical practices is the positron emission tomography/computed tomography (PET/CT) techniques that had been demonstrated to be an excellent method for stratifying patients with IHD. Its implementation could be useful for measuring mechanical capacity, microvascular circulation, and coronary flow reserve (CFR)11. The association between comorbidities, cardiac symptoms, and their relationship to myocardial function as evaluated by PET/CT has not been fully explored. The detection of this association could be useful for clinicians with insufficient resources to implement PET/CT imaging in at-risk populations, allowing for an early referral based on comorbidities and symptoms to a specialized cardiologic center.
Approach to the problem
There is an association between comorbidities and cardiac symptoms that alter myocardial function that could help clinicians to correctly identify at-risk population.
Objective
In this study, we intend to assess the joint impact of traditional risk factors with cardiac symptoms associated with ventricular mechanical impairments, ischemia, decreased CFR, and coronary artery obstruction in patients evaluated with PET/CT in a reference medical center in Mexico City. In addition to demonstrate, the relationship between comorbidities and the symptoms related to myocardial ischemia assessed with PET/CT.
Materials and methods
Study setting
The PET/CT unit in the Faculty of Medicine at the National Autonomous University of Mexico is a reference center for evaluating patients with CVD. We designed a cross-sectional study, all the data was collected from January 1, to December 31, 2019. Our inclusion criteria included patients who were ≥ 18 years and were referred to our PET/CT unit by a certified cardiologist due to typical or atypical symptoms related to angina and no history of medication that could modify their cardiovascular risk profile. For all our analyses, we excluded subjects who had previous history of myocardial infarction, arrhythmias, congenital heart disease, acute infections, or cancer at the time of PET/CT assessment. Medical records of subjects who had incomplete or inconclusive clinical information or whose PET/CT scan image were illegible, were excluded from the analysis. Data collectors were trained and supervised by a certified cardiologist during the study period. The Human Research Ethics Committee of the National Institute of Cardiology Ignacio Chávez approved the study, and all patients signed informed consent before the myocardial perfusion study (MPS).
Clinical and anthropometrical measurements
A professional physician performed a medical history interrogating for traditional risk factors which were defined as previous history of systemic arterial hypertension, type 2 diabetes mellitus, dyslipidemia, smoking, alcoholism, and overweight or obesity. We asked for specific cardiac symptoms such as chest pain, typical and atypical angina, palpitations, and dyspnea; history of previous myocardial infarction; and the imaging method used for diagnosis. Blood pressure was measured using a calibrated manual sphygmomanometer, after 5 min of rest of the patient, with an indication to stop smoking, alcohol, or caffeinated beverages before the appointment. Blood pressure was recorded directly before the myocardial perfusion study.
PET/CT perfusion procedure
The image acquisition procedure was performed according to the ASNC guidelines12, using a Siemens Biograph Vision 600 PET/CT (Erlangen, Germany). In our study, we used nitrogen-13 ammonium ([13N] – NH3) – radiotracer whose half-life is 9.9 min and is produced by a cyclotron, to evaluate myocardial perfusion, ventricular function, coronary flow, and CFR. Patients were placed within the PET/CT camera where 10 mCi of [13N]-NH3 were injected to obtain images in a linear mode acquisition for 10 min. The stress phase was performed 20 min after the rest phase ended, in which we administer intravenous adenosine at a dose of 140 mg/kg/min for 4 min. Afterward, 10 mCi of [13N]-NH3 were additionally administered, and the last stress images were retaken for 10 min. Once the image acquisition was completed, the intravenous catheters were removed. During the entire test, blood pressure and electrocardiographic data were recorded to monitor the patient.
Myocardial perfusion image technique and classification
MPS images were obtained in three main axes: short, vertical, and long horizontal axes. The images were processed by two certified nuclear cardiologists which ruled out the presence of perfusion defects. We performed a semiquantitative visual interpretation of tomographic perfusion images, both at rest and in stress, using a model that divides the left ventricle (LV) into 17 segments. Each segment was assigned with a score of 5 points: 0 (normal), 1 (slight reduction), 2 (moderate reduction), 3 (severe reduction), and 4 (absence of radioactive tracer uptake). The summed stress score (SSS) was considered the sum of the points assigned to each of the segments of LV during the stress phase, representing the perfusion at the peak of the exercise. Meanwhile, summed rest score (SRS) was the summed scores of all the segments in the images taken at the rest phase, which depicts perfusion at basal condition. The summed difference score (SDS) is the difference between the SSS and the SRS and represents the degree of reversibility of myocardial ischemia. SDS under 1 point was considered normal perfusion; mildly abnormal from 2 to 4; moderately abnormal from 5 to 7; and severely impaired perfusion > 8. Ischemia was defined as a SDS ≥ S13.
PET/CT coronary flow measurements
Coronary flow was obtained automatically using the Cedars Sinai Polar Flow program (QT PET software). For this purpose, three measurements were obtained at rest and in pharmacological stress. The total coronary flow and the flow of each artery (anterior descending, circumflex artery, and right coronary artery) were obtained automatically and independently during the two phases of the study in mL/min/g. The CFR was calculated by dividing the total coronary flow value obtained during the pharmacological stimulus by the flow value obtained at rest. A decreased CFR was defined as < 2 mL/min/g12,14,15.
Ventricular function using gated-PET
The use of [13N]-NH3 by synchronizing the PET camera with the patient's heart rhythm (Gated-PET) allowed automatic assessment of ventricular volumes in end-diastole and end-systole, as well as left ventricular ejection fraction (LVEF), both at rest and during pharmacological stress with adenosine. We defined an impaired ventricular mechanical function as a reduction of ≥ 5% in LVEF between the phase of stress and rest phase in the MPS. In subjects submitted to CT scan, we defined a significant arterial obstruction as a reduction ≥ 50%. Multivessel disease was defined as two or more obstructed coronary arteries.
Descriptive statistics
The frequency distribution of categorical variables was reported as frequencies and percentages. Continuous variables are presented as mean (standard deviation) or median (interquartile range) based on their normal distribution and homogeneity of variances assessed with the Shapiro–Wilk test and Levene test, respectively. Mann–Whitney U-tests were conducted to evaluate differences of continuous variables between subjects with and without ischemia. When relevant, χ2 and Fisher's exact test were carried out for categorical variables.
Comorbid conditions and cardiac symptomatology associated with myocardial impairments
We performed logistic regression models to assess the impact of traditional risk factors and cardiac symptoms in the impairments of mechanical function, ischemia, decreased coronary circulation, and coronary artery obstruction within our two groups of study. The goodness of fit of the logistic regression model was assessed using the Hosmer and Lemeshow test. The diagnosis and selection for our logistic regression models were conducted by assessing the lowest Bayesian information criterion, along with the highest R2.
EVALUATION OF MYOCARDIAL FUNCTION WITH TRADITIONAL RISK FACTORS AND SYMPTOMS
To evaluate whether an increased number of comorbid conditions and associated cardiac symptoms is associated with a decreased LVEF, ischemia, and CFR, we performed trend analyses categorizing the number of comorbidities and symptoms. Interaction analysis was evaluated to test whether the presence of any cardiac symptoms alters the relationship of comorbid conditions in myocardial function using the LVEF, ischemia, and CFR as our tested outcomes. All statistical analyses were performed using the R software (version 3.5.1). p < 0.05 was considered statistically significant.
Results
Study population
We recruited 1587 patients assessed with PET during our study period. After application of selection criteria, 1,273 (80.2%) subjects remained with complete clinical information and legible PET/CT scan image. Complete anthropometrical and clinical characteristics of our study population are presented in table 1. We observed a male predominance (66.1%) with an average age of 62.4 (± 12.7) years. Notably, patients with ischemia were older and more likely to be referred with angina than non-ischemic patients.
Table 1 Characteristics, comorbidities, types of studies conducted, and reasons for referral of subjects tested in the PET/CT unit in the faculty of medicine at the national autonomous university of Mexico
| Parameter | Total (n = 1273) | With ischemia (n = 360) | Without ischemia (n = 913) | p-value |
|---|---|---|---|---|
| Male (%) | 841 (66.1%) | 245 (68.1%) | 596 (65.3%) | 0.484 |
| Age (years) | 62.4 (± 12.7) | 64.1 (± 11.3) | 61.6 (± 13.2) | 0.008 |
| Weight (kg) | 76.4 (± 14.6) | 76.5 (± 14.6) | 76.3 (± 14.6) | 0.858 |
| Height (mts) | 1.75 (± 2.88) | 1.66 (± 0.1) | 1.81 (± 3.6) | 0.921 |
| BMI (kg/m2) | 27.7 (± 4.48) | 27.77 (± 4.25) | 27.65 (± 4.61) | 0.258 |
| Comorbidities and risk factors | ||||
| Hypertension (%) | 598 (47) | 204 (56.7) | 394 (43.2) | < 0.001 |
| Diabetes mellitus (%) | 265 (20.8) | 91 (25.3) | 174 (19.1) | 0.02 |
| Smoking (%) | 460 (36.1) | 155 (43.1) | 305 (33.4) | 0.001 |
| Pack-years | 3.28 (± 12.97) | 7.23 (± 20.37) | 1.72 (± 7.92) | < 0.001 |
| Alcoholism (%) | 206 (16.2) | 96 (26.7) | 110 (12) | < 0.001 |
| Family History of IHD (%) | 317 (24.9) | 169 (46.9) | 148 (16.2) | < 0.001 |
| Exercise (%) | 161 (12.6) | 88 (24.4) | 73 (8) | < 0.001 |
| Type of study | ||||
| PET (%) | 860 (67.6) | 147 (40.8) | 713 (78.1) | < 0.001 |
| CT (%) | 36 (2.8) | 0 (0) | 36 (3.9) | 0.001 |
| PET/CT (%) | 337 (26.5) | 193 (53.6) | 144 (15.8) | < 0.001 |
| Unknown (%) | 32 (2.5) | 19 (5.3) | 13 (1.4) | < 0.001 |
| Viability (%) | 8 (0.6) | 1 (0.3) | 7 (0.8) | 0.52 |
| Reason for referral | ||||
| Not specified (%) | 6 (0.5) | 4 (1.1) | 2 (0.2) | 0.2 |
| Rule out IHD (%) | 440 (34.6) | 149 (41.4) | 291 (31.9) | 0.868 |
| Angina (%) | 50 (3.9) | 35 (9.7) | 15 (1.6) | < 0.001 |
| Previous MI (%) | 191 (15) | 57 (15.8) | 134 (14.7) | 0.294 |
| Arrhythmia (%) | 7 (1.9) | 31 (2.4) | 24 (2.6) | 0.171 |
| Other (%) | 75 (5.9) | 19 (5.3) | 56 (6.1) | 0.072 |
BMI: body mass index; IHD: ischemic heart disease; MI: myocardial infarction.
Comorbidities and associated cardiac symptoms
Regarding associated comorbidities, 72.7% of patients reported to had at least one comorbidity. Grouping for comorbid categories, we observed that 36.4% had between one and two associated comorbidities, 31.6% three and four, and 4.7% more than five; only 27.3% reported no-associated comorbidities. We observed a high prevalence of arterial hypertension within our study population, followed by any type of dyslipidemia, smoking status, type 2 diabetes, and alcoholism. Patients classified with ischemia had a higher proportion of comorbidities and a higher proportion of familiar history of IHD than patients without ischemia.
Regarding associated symptoms, 45.8% arrived at our PET/CT unit with at least one associated symptom. The cumulative number of associated cardiac symptoms included 26.7% with one up to two associated symptoms, 11.6% with three up to four, and 7.5% more than five; 54.1% reported no-associated symptoms. The most frequently reported cardiac symptoms included chest pain, palpitations, and dyspnea.
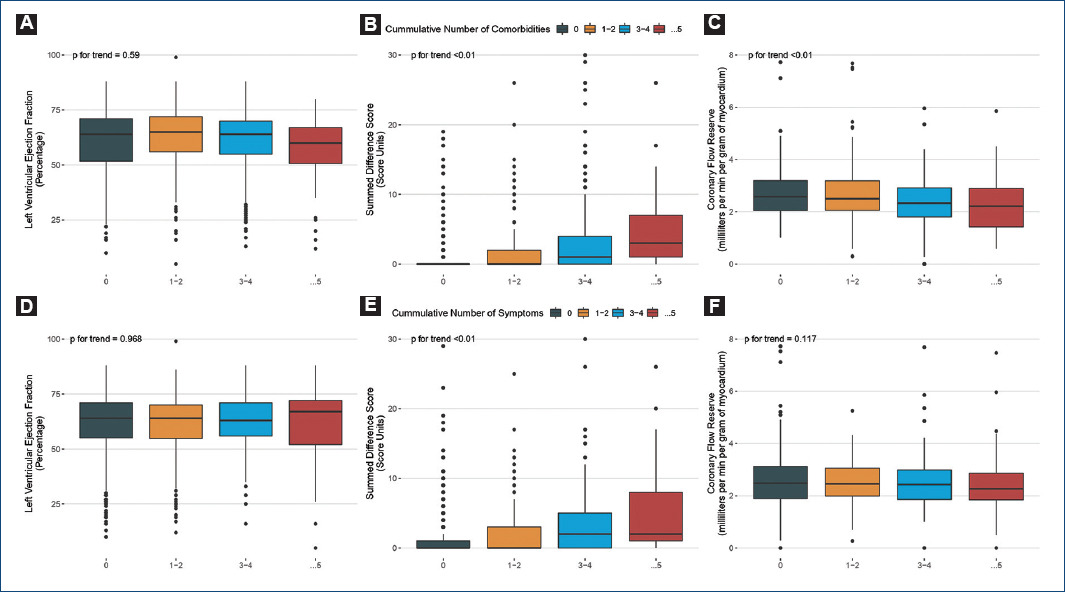
Traditional risk factors and associated symptoms related to myocardial impairments
In subjects classified with ischemia, we observed that men with increased body mass index, history of arterial hypertension, and that referred radiation of chest pain to any arm at the time of assessment were associated with impaired ventricular mechanical function. Moreover, male patients tend to have an increased likelihood of ischemia. We observed that patients with age over 65, with type 2 diabetes and a previous history of myocardial infarction were more likely to have a reduced CFR. In patients assessed with CT scan, we observed that type 2 diabetes and smoking status were associated with obstruction of any coronary artery and multivessel disease (Fig. 1A).
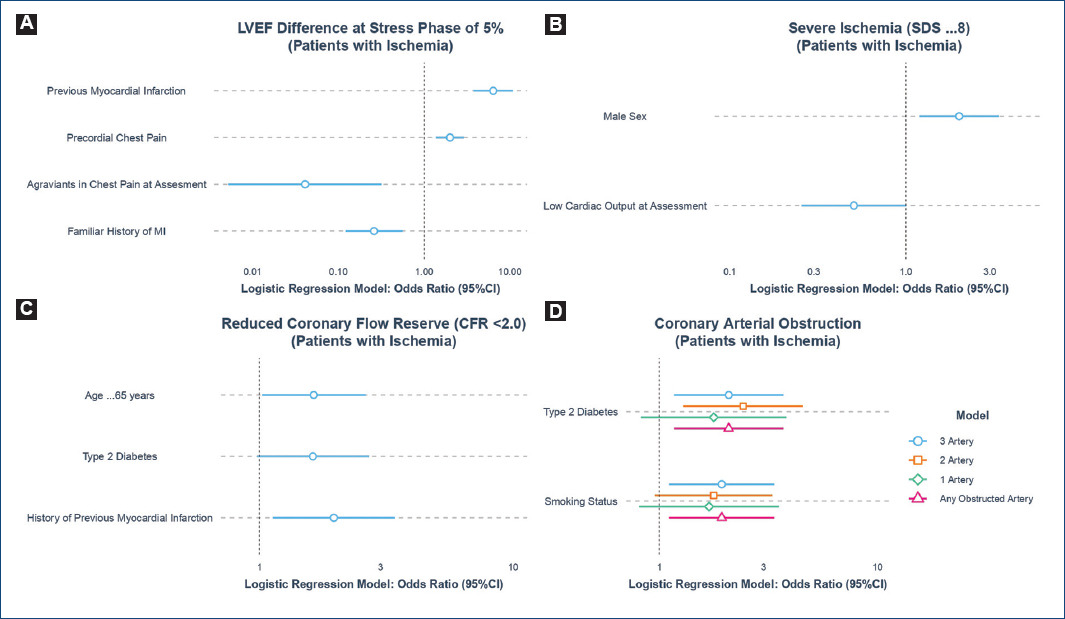
Figure 1A A: comorbidities and symptoms associated with left ventricular ejection fraction difference at stress phase of 5%, B: ischemia, C: reduced coronary flow reserve, and D: coronary arterial obstruction in patients with ischemia assessed with PET/CT.
We identified that patients without ischemia, a previous history of myocardial infarction and chest pain were associated with a difference in LVEF at the stress phase of 5%. In contrast, patients with ameliorators in chest pain and family history of myocardial infarction had decreased likelihood for this outcome. Notably, we observed that patients without ischemia living with arterial hypertension, type 2 diabetes, and dyspnea at evaluation increased the probability of having a reduced CFR. Finally, elderly male patients living with arterial hypertension had an increased probability of having multivessel disease without ischemia (Fig. 1B).
Increased risk factors and cardiac symptoms impact myocardial impairments
We hypothesized that the presence of cardiac symptoms modified the relationship between a higher burden of comorbidities and myocardial function. We observed a trend with a cumulative number of comorbidities and cardiac symptoms and an increased SDS and a decreased CFR, but not for LVEF parameters (Fig. 1C). Nevertheless, we noted an interaction effect with an increased number of comorbidities and any cardiac symptoms, associated with a lower LVEF compared to patients without cardiac symptoms (Fig. 1D).
Discussion
In this study, we report the frequency and prevalence of traditional risk factors and associated symptoms of IHD in a group of patients referred to a PET/CT unit in Mexico City. We observed a high prevalence of cardiovascular risk factors and adverse cardiac symptoms regardless of the presence of myocardial ischemia, suggesting that a high proportion of our population has a high burden of comorbidities and cardiac symptoms at clinical assessment.
The prognostic value of perfusion studies to predict cardiovascular events has been well studied, especially the PET stress modality that is associated with an augment in the frequency of known or suspected coronary artery disease adverse events.
Interestingly, clinical history of arterial hypertension, diabetes, and obesity significantly alters the myocardial function and CFR in patients classified without ischemia, which is translated into a growing atherosclerotic state before the onset of an acute ischemic syndrome. Finally, we observed that comorbidities alter ventricular function in addition to any cardiac symptoms, suggesting that the clinical presentation varies across the Mexican population's metabolic risk profiles.
It is important to mention that in patients with a greater the number of comorbidities, the greater the deterioration of cardiac function, while in those without comorbidities their cardiac function was significantly preserved.
All patients' comorbidities such as hypertension and diabetes were strictly under therapeutic goals during our study.
Identification of traditional risk factors related to the development of atherosclerotic events has been widely reported16,17.
It has been demonstrated that the factors related to the accumulation of lipid residues that damage the subendothelial layer are exacerbated when the number of comorbidities increases18. Recent reports have shown that the prevalence of traditional risk factors has increased in the Mexican population, displaying a high burden of chronic-health comorbidities that predispose to CVD5. Moreover, these factors are present in a population without myocardial ischemia, suggesting that chronic comorbidities are linked to a metabolic phenomenon that favors the development of subclinical atherosclerosis, decreasing myocardial function and CFR before an episode of myocardial infarction19.
Although several international organizations have created various recommendations to diminish the effect of chronic health conditions in global health, recent evidence suggests that Mexico continues to have increased trends in CVD-related mortality20. However, at an individual level, this phenomenon could be directly attributed to the high burden of comorbidities in the general population, adverse clinical presentation at the time of evaluation in a cardiology service, and the lack of referral centers to stage the size of myocardial abnormalities.
We found that in patients without ischemia, type 2 diabetes, arterial hypertension, and adverse cardiac symptomatology were associated with adverse function, perfusion, and coronary flow parameters.
PET is considered a non-invasive gold standard for the measurement of the coronary flow capacity, myocardial blood flow, and CFR, that offers an excellent methodology for selecting patients with ventricular dysfunction who would benefit from a revascularization. Assessment of functional abnormalities of the coronary vessels with PET may have an advantage over structural alterations of the arterial wall, as it may identify the earliest functional stage of development of the coronary atherosclerotic process21.
Our work has several strengths: first, patients were assessed by PET/CT, which is very accurate in detecting myocardial ischemia, coronary artery disease, and myocardial blood flow22. Furthermore, the large number of patients enrolled in our cross-sectional study allowed us to make detailed estimations of the prevalence of comorbidities and cardiac symptoms and make associations of these variables between parameters measured by PET/CT. The high burden of chronic comorbidities in Mexico makes it an ideal population to conduct this analytical cross-sectional study.
It exists a clear advantage of the acquisition of PET/CT, for the correct assignation of ischemia in every ventricular segment with a significant impact on the clinical treatment of coronary disease.
Chest pain in patients without obstructive coronary artery disease has been a frequent problem in clinical practice. Investigations have suggested that up to two-thirds of patients with non-obstructive coronary atherosclerosis may have microvascular dysfunction23. In particular, patients with type 2 diabetes mellitus exhibit accelerated progression of CAD, which may account for the increased morbidity and mortality in these patients. Assessment of functional abnormalities of the coronary vessels with PET may have an advantage over structural alterations of the arterial wall, as it may identify the earliest functional stage of the initiation and development of the coronary atherosclerotic24.
Conclusion
The patients studied with a PET/CT center of reference in Mexico City had a high burden of chronic comorbidities and traditional cardiovascular risk factors. The proportion of these comorbid conditions is enhanced in patients with ischemia. The high burden of comorbidities and symptoms in our population alters myocardial functionality regardless of the level of ischemia, which ultimately diminishes LVEF after the presence of any cardiac symptoms.
Patients with a greater number of comorbidities present consistently alterations in the PET/CT parameters, which are related to the onset of clinical manifestations such as angina, myocardial infarction, and the number of occluded vessels, highlighting the importance of PET/CT as a predictor of an accurate revascularization.
Limitations
Among our study's limitations, there is sampling bias since the PET/CT unit is a reference center for myocardial perfusion imaging in Mexico City, where only a selected number of patients are studied.
In our study, it was not included the basal heart rate and blood pressure after the max effect of the vasodilator, we also would like to have made a multimodal analysis to prove the hypothesis.











 nova página do texto(beta)
nova página do texto(beta)