History of presentation
A 53-year-old-male was admitted for rescue percutaenous coronary intervention (PCI) after a failed thrombolysis of an anterior STEMI. During the intervention, a Vieussens’ arterial ring (VAR) to main pulmonary artery (PA) fistula was documented. Months after successful PCI with a drug eluting stent to the mid left anterior descending artery (LAD), he began with progressive shortness of breath.
Medical history
Former smoker, overweight, and ischemic heart disease (the above-mentioned anterior STEMI).
Investigations
Coronary computed tomography angiography (CCTA) showed a conus artery with independent ostium at the right sinus of valsalva with a tortuous pre-pulmonary path which was anastomosed to with a left branch (from the left main stem) forming a vascular ring with pre and retroconal path, the VAR. The VAR had a fistula at preconal side that communicated with the PA with a niche of 8 × 14 × 8 mm and a 2 mm branch that was anastomosed to a bronchial branch. In the left coronary artery, the LAD showed the 3.5 × 21 mm stent. The other coronary arteries were normal (Figure 1, panel A).
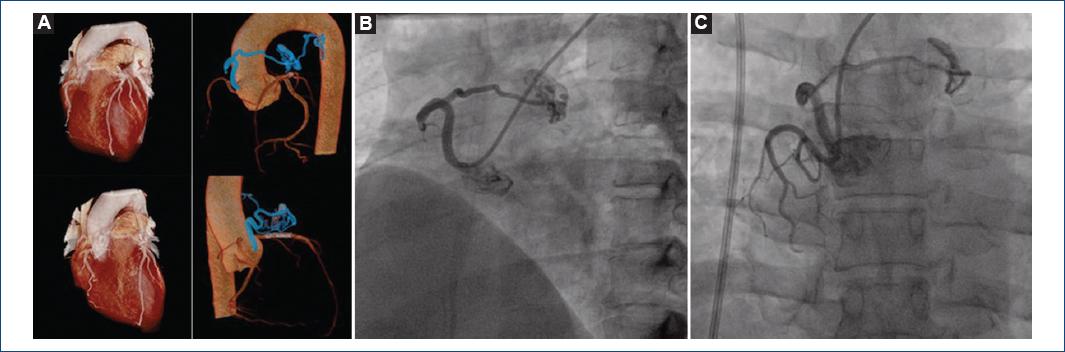
Figure 1 A: coronary computed tomography angiography 3D reconstruction. Vieussens’ arterial ring with an additional small bronchial branch surrounding the main pulmonary artery with a large niche that communicates with the pulmonary artery and its relationship with surrounding structures (blue). B and C: initial angiography. Small right coronary artery and an independent right conus artery (B) with pre and retroconal path (Vieussens’ arterial ring) with a large niche that communicates with the main pulmonary artery (contrast media delimitating the PA trunk) (C).
Management
We performed a transradial coronary fistula coil embolization. Using the transradial approach, we gain arterial access through the left radial artery with a 6 Fr hydrophilic introducer sheath. The initial coronary angiogram was performed using a 5 Fr JR 4. The CCTA findings were confirmed. Independent right conus artery and a VAR with pre and retroconal path. The large niche was arising from the preconal branch and it showed a large fistula by means of a large amount of contrast media passing to the main PA. Aiming to achieve the highest available support, a grandmother-mother-child (GMC) technique was performed. For this patient, we used a JR 4 guide catheter (the grandmother), a 6 Fr guide extension catheter (the mother) and a microcatheter (the child) over a 0.014’’ coronary wire. We took this assembly through the independent right conus artery to the preconal branch of the VAR just before the large niche. Being there, the coils deployment began: first a 2 mm x 4 cm, followed by a 5 mm x 8 cm and finished with a 5 mm × 15 cm coil. It was not until the last (third) coil that angiographic control showed a complete embolization without any evidence of complications (Figure 2).

Figure 2 A and B: grandmother-mother-child technique. The setup was a 6 Fr JR 4 guide catheter (the grandmother), a guide extension catheter (the mother) and a microcatheter (the child) over a 0.014’’ coronary wire. C-D: fistula coil embolization. Delivery (C) and deployment (D) of the three sequential coils until complete embolization. E-F: final results. Final angiographic control showing the independent right conus artery with absence of contrast media in its distal segments and no evidence of flow to the pulmonary artery.
Discussion
The VAR was first described in 1706 by Raymond de Vieussens as a collateral artery between the conus branches of the right coronary artery and the left anterior descending coronary artery, found in almost half of the population1, such as this case with a vascular ring surrounding the pulmonary artery trunk although with the particular difference of an independent ostium for the right branch of the VAR. The primary pathologies associated to VAR are extremely rare and in the context of a coronary artery fistula, a fistula from a VAR to the pulmonary artery is even infrequent2: it has been reported that incidental diagnostic rate in adults is < 0.1% in patients undergoing invasive cardiovascular imaging3. Usually, coronary to pulmonary artery fistula embolization can be achieved by coils or vascular plugs and this kind of procedures are indicated in cases of symptoms associated with the large shunt caused by the fistula or in cases of asymptomatic patients but a Qp: Qs >1.53. The first report of percutaneous embolization of a VAR to pulmonary artery was in 2010 by Hirzalla et al. They successfully used coils and an Amplatzer duct occluder through a transfemoral approach4. With the evolution to a minimally invasive PCI and the advent of transradial approach, a continuous number of procedures previously thought to be only doable through a femoral access can now be performed through a radial access. Still there are some limitations like the lack of support such as in complex anatomies, but there are several advanced transradial techniques to improved it. One of these techniques is the so-called GMC technique, in which the operator puts a microcatheter (child) inside a guide extensor catheter (mother) and both go inside the guide catheter (grandmother), achieving the highest active support available for transradial intervention, method that also has been used to safely perform a coronary fistula coil embolization without the classic and more invasive femoral approach5. The use of this safe and minimally invasive technique for coil embolization of an extremely rare coronary artery fistula (VAR to main PA fistula) was able to be carried out with success thanks to the proper support achieved with this technique.











 nova página do texto(beta)
nova página do texto(beta)


