Introduction
A persistent sciatic artery (PSA) is an embryologic remanent of the internal iliac artery, being present in 0.03-0.06% of the population1. The sciatic artery is a branch of the umbilical artery and the main arterial supply of the lower limbs during the embryonic phase until the 3rd month of development which is supply by the superficial femoral artery (SFA), and then, the umbilical artery develops into the internal iliac artery. The PSA may persist when the SFA develops incompletely, and when this happens, the internal iliac artery supplies blood to the lower leg through the PSA2. PSA can occur on the right leg, the left leg, or bilaterally, in 50%, 20%, and 30% of the cases, respectively. The PSA can be completed or incompleted, depending on whether the SFA is normal, hypoplastic, or absent3.
Physicians must acknowledge the existence of PSA since up to 50% of the patients with this anomaly will eventually develop aneurysmal formation, leading to an increased risk of acute lower ischemia and potential limb loss4.
The present study's objective is to describe a 56-year-old female patient with PSA who presented with acute limb ischemia. A review of the literature is also presented.
Case report
A 56-year-old female patient with a previous history of ovarian cancer was electively admitted for a ventral hernia repair. Laboratories were within normal parameters. During completion of the herniorrhaphy, under general anesthesia, the patient presented sudden hemodynamic instability, with tachycardia and hypotension, without an explained cause. She was transferred to the coronary unit, and cardiac studies were within normal parameters. On the 2nd post-operative day, she was extubated, and on the 3rd post-operative day, when she tried to walk, she referred acute right leg pain on a scale of 9/10. Physical examination showed absent right popliteal and tibial pulses, with a regular femoral right pulse. An arterial Doppler ultrasound was ordered, where thrombotic occlusion of the right popliteal and tibial arteries was seen. She was taken to the angiography suit, where an angiogram was performed with us-guided puncture to the left common femoral artery, after crossover, an angiogram showed adequate patency of the common and profound femoral arteries, with a hypoplastic SFA and a right occluded popliteal artery (Fig. 1A-C). The decision to perform the right popliteal conventional thrombectomy was made. A right popliteal incision was made at P1 level, popliteal arteriotomy was performed, and embolectomy was achieved with a 3-fr Fogarty catheter. The final angiogram showed adequate patency through the popliteal and tibial arteries, with adequate flow to the foot. The incision was closed, without incidents. After the procedure, a magnetic resonance angiogram was done where a right permeable sciatic artery was confirmed, with good outflow toward the infrapopliteal vessels (Fig. 2A-C). The patient recovered uneventfully and was discharged on POD 3 with aspirin 100 daily. On a 12-month follow-up, the patient is doing well, with adequate infrainguinal pulses, and without claudication or rest pain.
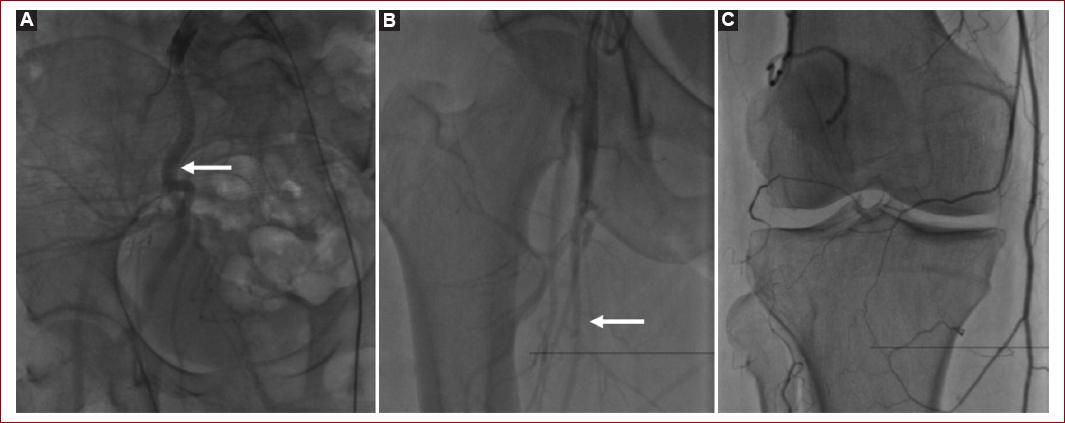
Figure 1 Angiogram. A: persistent sciatic artery (white arrow). B: hypoplastic superficial femoral artery (white arrow). C: popliteal artery occluded due to embolism.
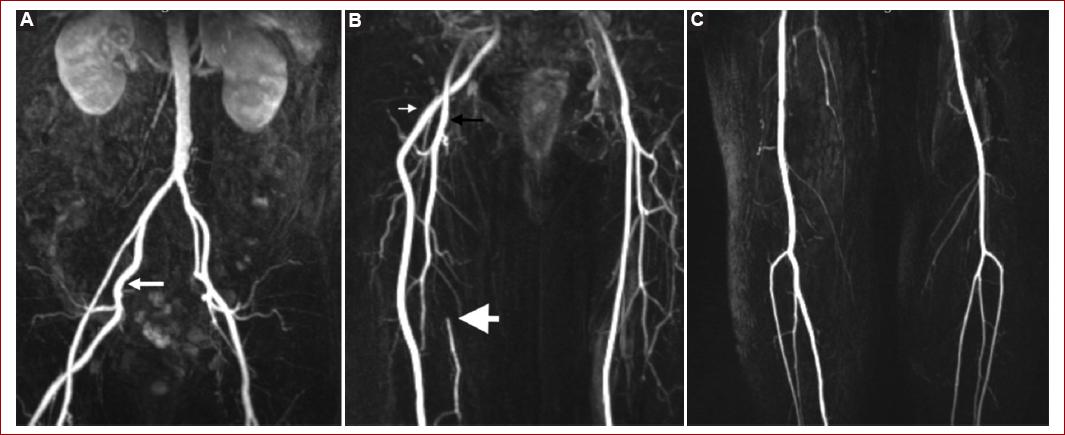
Figure 2 Magnetic resonance angiogram. A: aortic bifurcation. A hypoplastic external iliac right artery with a persistent sciatic artery (white arrow). B: right persistent sciatic artery ending in the popliteal artery (thin white arrow). Profunda femoris of good caliber (black arrow). Hypoplastic superficial femoral artery occluded in its middle third (thick white arrow). C: post-embolectomy right popliteal artery runoff with good outflow.
Discussion
PSA is an uncommon anomaly that develops when the SFA is involuted during gestation. Making the diagnosis is a challenge, and most people presenting this anomaly live asymptomatic. The most common symptoms are limb ischemia (claudication, rest pain, or necrosis) and mass formation, being less frequently encountered neurological disorders, such as radicular pain or foot drop4. In a systematic review of PSA by Van Hooft et al.4, 146 PSAs in the literature were studied. They found that 80% of the patients presented symptoms, with 26.3% having acute onset. The most common symptom was rest pain (29.6%), followed by claudication (27.4%).
In most cases, the diagnosis is made incidentally during physical examination for lower extremity symptoms such as claudication, rest pain, or acute thromboembolism5. Our patient presented with sudden acute leg pain due to acute embolism. A positive Cowie's sign might be seen when distal pulses are present in the absence of femoral pulses. This sign is pathognomonic for PSA6. In our patient, this sign was absent, and on the contrary, a femoral pulse was present, and popliteal and tibial pulses were absent.
Diagnostic tests might vary, and the most frequently used include computed tomography angiography (CTA), magnetic resonance imaging (MRI), and angiography. CTA and MRI are useful for showing possible aneurysmal formation of the artery and its relationship with adjacent structures such as the sciatic nerve. Furthermore, they can show a totally occluded PSA that might not be seen with angiography. Our patient's diagnosis as first was made with angiogram, and postoperatively confirmed with MRA, where the PSA was seen without aneurysmal degeneration. Arterial Doppler ultrasound can also help with diagnosis; nevertheless, a meticulous examination should be made as the absence of the SFA might lead to the assumption of a complete thrombosis of the vessel, confusing it with a hypoplastic vessel. Ultrasound scanning through a posterior approach can help to identify a PSA and its collateralization of the above-knee popliteal artery7.
Angiography is the most used study for detecting PSA since it gives information about the classification and outflow of the PSA. Pillet et al.8 in 1980 described four different types of PSA. Types I and II involve a complete PSA in combination with a complete femoral artery and an incomplete femoral artery, respectively. In subtype IIa, the SFA is present without reaching the popliteal artery; in subtype IIb, the SFA is absent. Type III has an incomplete proximal PSA with normal femoral arteries. Type IV has an incomplete distal PSA with normal femoral arteries. A V type was added 12 years later by Gauffre et al.9 where the PSA originated from the sacral artery, with developed and undeveloped SFA corresponding to types Va and Vb, respectively. Our patient presented with type IIa because he had a complete PSA with a hypoplastic SFA. Table 1 summarizes the types of PSA.
Table 1 Types of persistent sciatic artery
| Type | Persistent sciatic artery | Superficial femoral artery |
|---|---|---|
| Type I | Complete | Complete |
| Type II a | Complete | Incomplete (does not reach the popliteal artery) |
| Type II b | Complete | Absent |
| Type III | Incomplete (lower part is absent) | Complete |
| Type IV | Incomplete (upper part is absent) | Complete |
| Type V a | Originate from sacral artery | Complete |
| Type V b | Originate from sacral artery | Absent |
Patients can present with stenosis or aneurysm with and without distal thrombosis of the PSA4. The precise cause of why an aneurysm is recurrently seen in a PSA is undetermined. One theory is that the vessel is affected by recurrent trauma from compression against the sacrospinous ligament, piriformis muscle, and hip during flexion of the hip articulation, causing destruction of the adventitia and media, resulting in aneurysmal dilatation10.
Treatment depends on the type of PSA encountered and on the symptoms of the patients. If the PSA or the SFA is hypoplastic or incomplete, maintaining circulation to the lower extremities should be the primary objective. A femoral-popliteal bypass, ilio-popliteal-transobturator bypass, or interposition bypass can achieve revascularization4. If an aneurysm is encountered and the PSA is patent, ligation of the PSA can be safely performed. If the PSA is not patent, then end-to-end reconstruction after aneurysmectomy can be done using a venous or prosthetic graft7. Endovascular treatment with stent placement has also been reported with reasonable patency rates1. If the patient is asymptomatic, conservative treatment is recommended, with active image surveillance, due to the high incidence of aneurysmal formation, or thromboembolic events7,11. Our patient presented with a patent PSA, so the embolism acute event was resolved by embolectomy, and the PSA was left intact. Furthermore, the patient will be kept under active surveillance due to the known risk for PSA aneurysm formation in up to 50% of the cases11.











 nueva página del texto (beta)
nueva página del texto (beta)


