Spondylolisthesis is defined as the disorder that causes the slip of one vertebral body over the one below. The name derives from the Greek terms «spondylos» meaning «vertebra» and «olisthesis» meaning «to slip».1,2 In 1963, Newman used for the first time the term «Degenerative Spondylolisthesis» to refer to the slipping of the anterior vertebral body in the lumbar region, relating it to the elderly female population and identifying it as an independent physiological entity.3
Historically, the biomechanics of degenerative spondylolisthesis was understood in 1978 by Kirkaldy-Willis considering it as a chronic identity described as a cascade of events that lead to degeneration and instability of the periarticular vertebral complex that includes the intervertebral disc and the facet joints.4
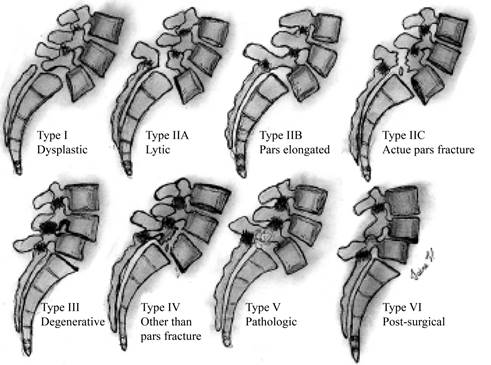
Because of the given knowledge of the different mechanisms that lead to the slipping of the anterior vertebral body, a classification based on the etiology or the degree of displacement of the spondylolisthesis was described.5 Two of the more used classification systems for spondylolisthesis were proposed by Wiltse et al.6 and Marchetti, and Bartolozzi.7 In 1962 Wiltse and Newman established a classification for spondylolisthesis based on the etiology.1 They include in their classification the pseudospondylolisthesis, described by Junghans; where the slipping of the vertebral body is observed because of the alteration of the articular cartilage that produces a sagittalization of the facet joints.1 In this way, they classify spondylolisthesis secondary to a defect in the pars interarticularis, due to the erosion of the articular processes, fractures-dislocations or secondary to destruction of the support elements, and describe that spondylolisthesis, although it can result from different causes, the most common is the separation of the pars interarticularis followed by degenerative diseases, fractures-dislocations, and diseases that cause bone destruction such as tuberculosis or cancer.8 They classified it into six types:
Type I: or dysplastic, includes congenital dysplasia of the sacrum or L5 neural arch that can subsequently result in elongation or lysis of the pars.
Type II: or isthmic, is a defect in the pars interarticularis with lysis of the pars (type IIA), elongation of the pars (type IIB), or an acute fracture (type IIIC).
Type III: or degenerative, it is the result of facet osteoarthritis that leads to vertebral slippage.
Type IV: or traumatic, it is secondary to an acute fracture of the posterior elements or other structures where the pars interarticularis is not involved.
Type V: or pathologic, it is associated with the incompetence of the posterior elements secondary to systemic diseases or bone pathological processes.
Type VI: or postsurgical, it is the result of the loss of posterior elements due to surgery (Figure 1).1
Degenerative spondylolisthesis is considered a disease of aging, the main reasons that lead to the development of a degenerative spinal slip are:
Disc degeneration.
Malfunction of the stabilizing component of the ligaments.
Osteoarthritis of the facet joints with loss of their normal structural support.
Ineffective muscle stabilization.3
After the degenerative changes end up destabilizing the intervertebral joints, spondylolisthesis occurs following a direction that depends mainly on two factors: the symmetry of the articular facets and the distribution of weight loads. When the facet subluxation is symmetric, the sliding is mainly sagittal, but with the asymmetric subluxation occurs a deformity with a rotational component.2
Since its description, degenerative spondylolisthesis has been the subject of multiple studies. While controversies continue regarding its pathogenesis, some aspects are notable: it is rarely found in people under 50 years, the female-to-male ratio of 5:1, black women are three times more affected by this pathology than Caucasian females.9,10,11 Vertebral sliding usually occurs in the L4-L5 segment and rarely exceeds 30% of the anteroposterior diameter of the vertebral body; it is in itself, usually asymptomatic, and there is no clear relationship between symptoms and the degree of listhesis, although the degree of degeneration does increase the risk of progressing to lumbar spinal stenosis and, thus causing clinical symptoms. Some authors have analyzed facet orientation to determine if it is the cause or consequence of segmental instability without reaching an obvious conclusion.12,13,14 Iliac crests height, ligament laxity, and degrees of pelvic tilt are others of the parameters studied to find their correlation.11
A comprehensive review was conducted in 2007 by Jacobsen et al. in the database of Copenhagen osteoarthritis study, where records have been made since 1976 involving 4,151 patients between 22 and 93 years of age to determine the age and sex distribution of degenerative spondylolisthesis in the general population, to know if there is a correlation between physical characteristics such as weight, height, body mass index, degree of lordosis and pelvic tilt, to identify the association between degenerative spondylolisthesis and low back pain and also to assess if there is a relationship between the number of children, occupational exposure weight-bearing and smoking. Patients with a previous history of lumbar surgery were excluded. In total, 4,001 patients were included in the study (1,495 men and 2,506 women). The results show that women have a higher risk of suffering from L3 and L4 spondylolisthesis compared to men, and there was no difference in the prevalence of L5 spondylolisthesis. Forty-one cases (2.7%) of spondylolisthesis were found in men and 213 in women (8.4%). At the L4 level, the female-male ratio was 6.4:1. No correlation was found between the age of presentation of menopause and the presence of degenerative spondylolisthesis, none association was found between null, and multiparity and the number of deliveries didn’t significantly increase the incidence of spondylolisthesis. The average age of men with spondylolisthesis was 68 years old and in women was 71 years old. In men, only L4 spondylolisthesis was correlated with age, and in women, L4 and L5 spondylolisthesis were associated with age. The average body mass index in men was 25.7 kg/m2 in 1976, increasing to 26.4 kg/m2 17 years later in 1993. The body mass index in women was 24.4 kg/m2 in 1976, increasing to 25.7 kg/m2 in 1993. In men, none association was found between body mass index and degenerative spondylolisthesis, and in women, a significant correlation was found between body mass index and the development of L4 listhesis. Increased lumbar lordosis and pelvic tilt were significantly associated with degenerative L4-L5 spondylolisthesis in women, and occupational exposure to repeat weight-bearing or smoking was not associated with their presence.15
Degenerative spondylolisthesis is the cause of low back pain in some patients, and the origin of pain in these patients comes mainly from the degenerated and subluxated facets joints, the segmental instability that causes tension on the facet joint capsules and ligaments and, the compensatory muscle spasm to the instability and central or foraminal stenosis that generates radicular pain.16,17 The main discomfort of patients is the recurrent low back pain,18 symptoms may be related to spinal stenosis or mechanical low back pain. In cases of extreme stenosis, bowel-bladder dysfunction can develop, as reported by Kostuik et al.19 Stenosis symptoms are the result of mechanical and vascular factors, neurogenic claudication occurs in 75% of patients; it is caused by blood hypoperfusion secondary to the compression of the nerve roots, manifesting as pain in the lower limbs with variable walking distances. As the listhesis progresses, facet hypertrophy, thickening of the yellow ligament,20 and disc bulging can lead to increase compression and sometimes trigger the symptoms of cauda equina syndrome, which, unlike its acute presentation in herniated discs, in spinal stenosis, it presents in an insidiously and subtly way.21 Symptom relief may occur after performing a trunk flexion widening the spinal canal, some patients with severe symptoms report the need to sleep in a fetal position to relieve their symptoms in the legs, and the vascular component may be so significant in some patients that it causes a restless leg syndrome.22
As part of diagnostic studies, radiography is the first line in suspected spondylolisthesis. The gold standard is the lumbar anteroposterior radiograph that allows us to evaluate the coexistence of scoliosis that may be secondary to the spasm of paravertebral muscles, degenerative changes, or alterations in symmetry in the hips and iliac crests. Lateral lumbar radiography is used to identify if there are defects in the pars interarticularis and to stage the degree of listhesis according to the Meyerding classification.23 The abnormal slip can increase in a standing position compared to the supine position, where it can even be reduced until it is negligible.24 Standing dynamic lateral radiographs are used to evaluate the degree of segmental instability in flexion and extension.25 Sometimes a trapezoidal shape of the 5th lumbar vertebra can be seen as a result of the listhesis and not as its cause.26 If the radiographic series are not sufficient to identify and stage of spondylolisthesis or there are previous surgical procedures performed on the posterior vertebral arch, computed tomography studies are requested as complementary auxiliary diagnostic and preoperative planning.27 Magnetic resonance imaging is indicated when neurological signs and symptoms are present and is an aid in the evaluation of the spinal cord and nerve roots, helps in the assessment of the degree of disc degeneration, the staging of the chronicity of the condition, and the assessment of added lesions or secondary spondylolisthesis to other causes.28
Various methods have been proposed to stage the degree of spondylolisthesis, the most universally used is the Meyerding method.23 This method is used in lateral lumbar spine radiography to measure the anteroposterior diameter of the upper platform of the lower vertebra and divide it into quarters, assigned from I to IV according to the degree of displacement of the upper vertebra (Figure 2). Some authors describe their preference for the Tailard method,29 referring to it as more accurate.30 This method is similar to Meyerding’s, measures the degree of displacement of the upper vertebra concerning to the lower vertebra in percentage. Other methods divide the percentage of anterior translation into < 50% as stable and > 50% as unstable. Some studies report up to 15% inter-observer error with these methods.31 Other studies used in the preoperative evaluation include panoramic radiographs in which the sagittal, coronal, and spinopelvic balance parameters are measured to evaluate the degree of correction necessary for an optimal result. Electrodiagnostic studies such as electromyography and motor-somatosensory evoked potentials that allow us to evaluate the functionality of the nerve pathways and the neuromuscular junction. Also, these studies have the purpose of evaluating other causes when it is suspected that the alterations are not caused by the listhesis.31
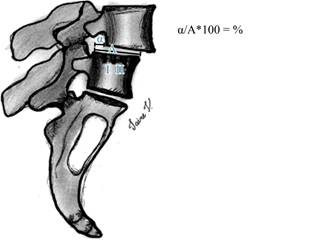
Figure 2: Artist’s illustration of the slippage of the vertebrae. Classification of spondylolisthesis is based on the degree of slippage in the lumbar spine. Grade 1 is less than 25%, grade 2 is 25 to 50%, grade 3 is 50 to 75%, grade 4 is 75 to 100%, and spondyloptosis is > 100%. Line A. The lower vertebral body is divided into four parts; α. distance between vertebrae. The percentage is obtained in the division between α/A.
The natural history of spondylolisthesis is favorable in its prognosis (Table 1). Only 10 to 15% of patients asking for medical attention go to surgery.32 In a long-term follow-up study of 145 patients with spondylolisthesis managed without surgery, listhesis progression was observed in 34%. No relationship was found between the progression of listhesis and changes in symptoms; it was observed that the development of osteophytes, the thickening of the yellow ligament, and the ossification of the intervertebral ligaments could generate a secondary stabilization that prevents sliding. 76% of the patients without neurological deficit remained symptom-free in a 10-year follow-up. 83% of patients with neurological deficit in the initial evaluation who refused surgery had a poor final prognosis.33 In another study, Johnson et al.34 followed 32 patients, which 9 had a diagnosis of spondylolisthesis with clinical symptoms and the rest with a diagnosis of lumbar spinal stenosis with an average follow-up of 49 months. 75% of the patients had neurogenic claudication, and in the follow-up, the same number of patients continued with the symptoms, although these were less, in general, 70% of the patients had no changes in the symptoms, 15% improved, and 15% got worse, there was no evidence of severe worsening of symptoms at a 4-year follow-up.
Table 1: General principles of degenerative spondylolisthesis.
| General principles |
|---|
| • Displacement of 1 vertebra over subjacent vertebra |
| • Associated with degenerative changes |
| • Most common in people older than 50 years old |
| • Female-to-male ratio of 5:1 |
| • The most affected segment is L4-L5 |
| • Symptoms: neurogenic claudication, lumbar pain, with or without radicular pain |
| • Conservative treatment is the first-line therapy |
| • Evaluation include panoramic radiographs, magnetic resonance imaging and electromyography |











 nueva página del texto (beta)
nueva página del texto (beta)