A 53-year-old female presented with Type 2 diabetes, systemic arterial hypertension, and mixed dyslipidemia. She presented at youth intermittent episodes of lipothymia, and for 3 years ago history of angina and v dyspnea on exertion. Her physical examination was unremarkable. ECG showed sinus rhythm, with the left bundle branch block and left ventricular hypertrophy, QS complexes in V1-V2 with poor R-wave progression from V3 to V6. Transthoracic echocardiogram showed left ventricular ejection fraction 50%, dilated left chambers, and eccentric hypertrophy of the left ventricle. Coronary angiotomography showed an anomalous origin of the left coronary artery (LCA) from the pulmonary artery trunk, with diffuse ectasia of the coronary arteries and collaterals formation from the right coronary artery (RCA) to the left anterior descending (LAD) artery and circumflex; without atheroscletic coronary lesions documented and a coronary calcium score of zero (low risk) (Fig. 1). Cardiac magnetic resonance imaging (MRI) confirmed the anomalous origin of LCA from the pulmonary trunk (ALCAPA) or Bland-White-Garland syndrome. MRI was also instrumental in planning the surgical approach1. It allowed for reconstruction of data in any imaging plane, giving complete visualization of complex cardiac anomalies, such as this case. The assessment in this case must involve a variety of imaging modalities that can be used in a complementary way and to increase sensitive, specificity, and predictive values.
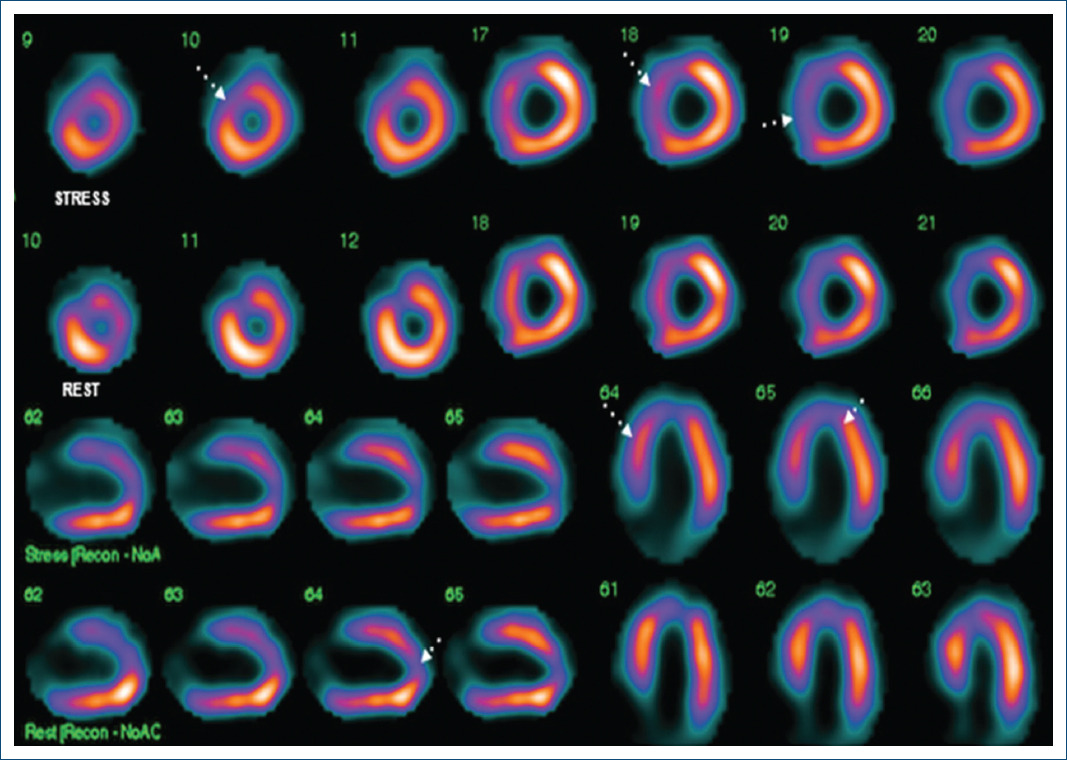
Figure 1 Protocol stress-rest with 99mTc-methoxy-isobutyl-isonitrile (99mTc-MIBI) myocardial perfusion SPECT images pre-operative of the short-axis slices, horizontal, and vertical long axis. The images show a defect in the apex, apical anterior, and septal wall, which during stress increases the defect. Non-transmural infarction of the apex and anteroapical with mild ischemia.
In addition, significant angulation of the left main coronary artery and LAD and dilation of the left chambers were noted by the study. Protocol stress-rest with 99mTc-methoxy-isobutyl-isonitrile (99mTc-MIBI) myocardial perfusion SPECT showed anteroseptal and apical non-transmural infarction with mild residual ischemia (Fig. 2). Surgical correction with reimplantation of the LCA to the aorta was performed. The procedure was uneventful, there were no post-operative complications, and the patient fully recovered. The patient has been asymptomatic since the surgical procedure. Cardiac MRI after the procedure showed post-surgical reimplantation of the left main coronary artery to the aorta, no significant changes in the other cardiac structures were noted.
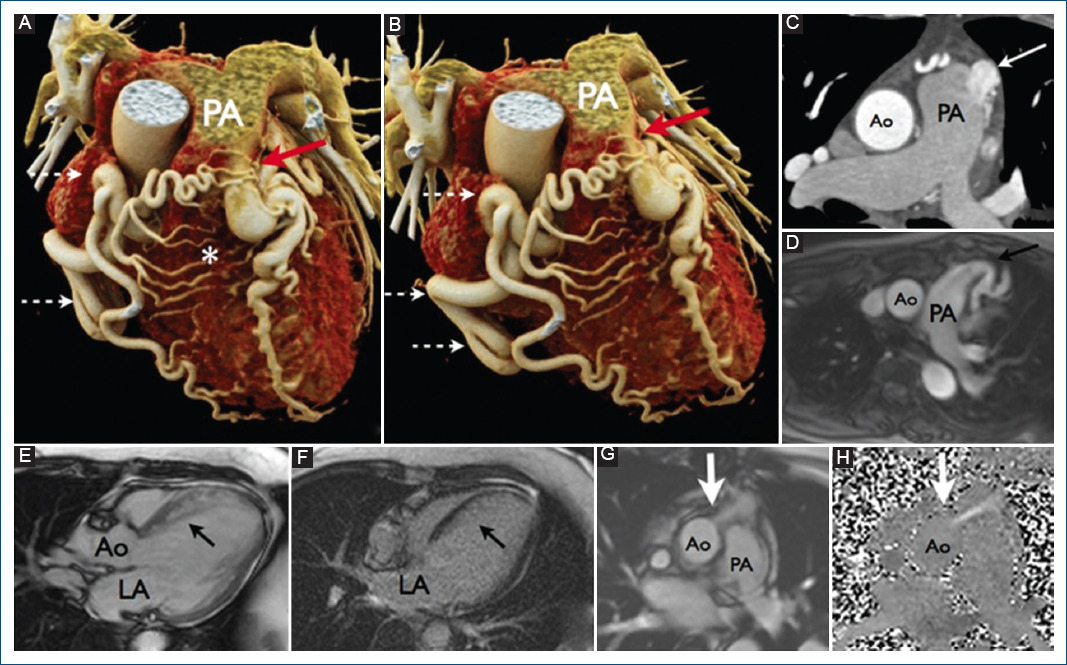
Figure 2 Coronary computed tomography angiography. A, B: volumetric reconstruction the origin of the left coronary trunk from the pulmonary trunk (red arrow), and a significant dilation of the right coronary artery (discontinuous arrows), with multiple collaterals between right and left circulation (*). C: axial section at the level of pulmonary trunk in which the arrow indicates the passage of contrast from the left main coronary artery to the pulmonary artery. D-H: magnetic resonance. D: the left main coronary artery from the pulmonary artery, with posterior angulation of the same (black arrow). E: three-chamber image in diastole where an increase in septum thickness is observed (black arrow). F: with an increased signal intensity in the investment recovery sequence this in relation to collateral circulation. G, H: axial section at the level of the site of reinsertion of the LMCA to the anterior wall of the ascending.
Discussion
Bland-White-Garland syndrome refers to the anomalous origin of the LCA from the pulmonary artery instead of the aorta (ALCAPA). It accounts for 0.25-0.5% of congenital heart disease2. It was first described in 1911 by Abrikossoff, who reported the finding in the autopsy of a 5-month-old infant, who had a left ventricular aneurysm. In 1933, Edward Bland, Paul Dudley White, and Joseph Garland, from the Massachusetts General Hospital, published the first clinical description of the syndrome3.
Malrotation of the septum, in the embryonic period, generates a malposition of the coronary buds causing the anomaly. Accordingly, the anomaly is associated with ventricular septum defects, ductus arteriosus, and tetralogy of Fallot3.
Clinical presentation can range from sudden death at birth, to dyspnea, pallor, and failure to thrive in infants. Adults present with chest pain, angina, syncope, heart failure, or sudden death. Adults who develop heterocoronary collateral vessels can be asymptomatic. In the absence of collateral circulation, mortality is approximately 90% without prompt diagnosis and surgical repair2,4. Perfusion of the anterior wall depends on the collateral circulation of the RCA. This can cause perfusion defects leading to ischemia. In fact, our patient presented with a non-transmural infarction of the anteroseptal and apical wall5.
Several surgical techniques to repair the anomaly have been proposed, nevertheless, the current treatment, proposed by Neches, et al. (1974), consists in the reimplantation of the anomalous LCA ostium to the aortic sinus1. If this procedure cannot be done, the approach proposed by Takeuchi in 1979 consists in creating a tunnel between the pulmonary artery coming from the aorta to the ostium of the coronary artery1.
Hence, it is an extremely rare pathology in adulthood. The formation of collateral circulation plays a critical role in survival, as noted above. This was the case in our patient, who developed symptoms in her fifth decade of life2,3.
Our patient had a high pre-test probability of obstructive coronary disease, 66-85% according to the European guidelines, given her comorbidities, thus the indication for angiotomography which eventually showed the anomalous origin of the LCA1; this is the reason why an angiography was not performed as the initial study to know the coronary anatomy of our patient. The purpose of performing a MRI, despite having coronary artery angiotomography, was to have a baseline study, to opt for that same study as a follow-up and avoid the use of contrast and generate acute renal injury. As stated above, this pathology is uncommon in older adults because of its high mortality at young age, our patient is one of the oldest reported in the literature who survived with this anomaly until surgical correction was performed2,3.
Cardiovascular imaging is at a crossroad with respect to technological advances, with a shift in focus from single modality-based diagnosis to an integrated multimodality approach to comprehensive assessment of morphology, pathophysiology, and biology of disease phenotype, risk stratification, and guidance of therapy.
Finally, it is important to mention that the prompt recognition of this syndrome, as well as its appropriate evaluation and management, has a major impact on the life expectancy and quality of life of patients affected.











 nueva página del texto (beta)
nueva página del texto (beta)


