1 Introduction
The Coronavirus Disease-2019 (COVID-19) [1] as per in Fig. 1 seems to be a breathing disorder triggered by some severe respiratory syndromes coronavirus 2 (SARS-CoV-2), an infectious infection upon the single stranded RNA class of coronaviridae.
SARS-CoV-2 targets the immune function, identical towards the pathogen, inducing illnesses namely coughing, exhaustion, tiredness and immune issues. Whilst not accurately identified as the point of origin of the pathogen, researchers also explored its SARSCoV 2 genetic code and defined that it must be part of the coronavirus genealogy’s β-coV breeding, that commonly borrows its mutation evidences from bat and rodent [1].
The COVID-19 pathogen primarily migrates via droplets from the mouth or nasal release whether an illness is sternutation therefore they would also do have a coughing strategy such as cough with a bent forearm. This is why the current COVID-19 epidemic was considered here by the the world health organization (WHO) seems to be an immediate global epidemic. This typically requires a significant duration by using conventional approaches for creating a medicine.
However, a variety of clinical studies on alternative treatments are being carried out. Until the clinical findings are available, WHO may keep updated information. The Basic testing benchmark is really the microbial diagnostic examination, which requires hours for critical false negative results. For all emerging and unstable nations, the comprehensive implementation of COVID-19 studies, that have become extremely expensive, is not feasible.
The WHO claims the world’s total coronavirus counts is 4,396,392, although the mortality rate was 300,441 [2] and the number is increasing day by day. The exponential growth of COVID-19 accidents across the globe has ensured that urgent safeguards are required to reduce the devastating consequences of COVID-19.
The identification of a significant amount of confirmed patients with effective isolation and prevention procedures plays a very important role to regulate the transmission of the infection. Owing to the elevated amount of incidents every day, a small proportion of COVID-19 testing packages are accessible in hospitals. COVID-19 is a deadliest disease that has taken a toll on thousand’s of precious human lives world-wide.
Each and every country is battling it in their own way by social distancing, masks,etc. But, the COVID-19 pandemic is here to stay with us for long time.
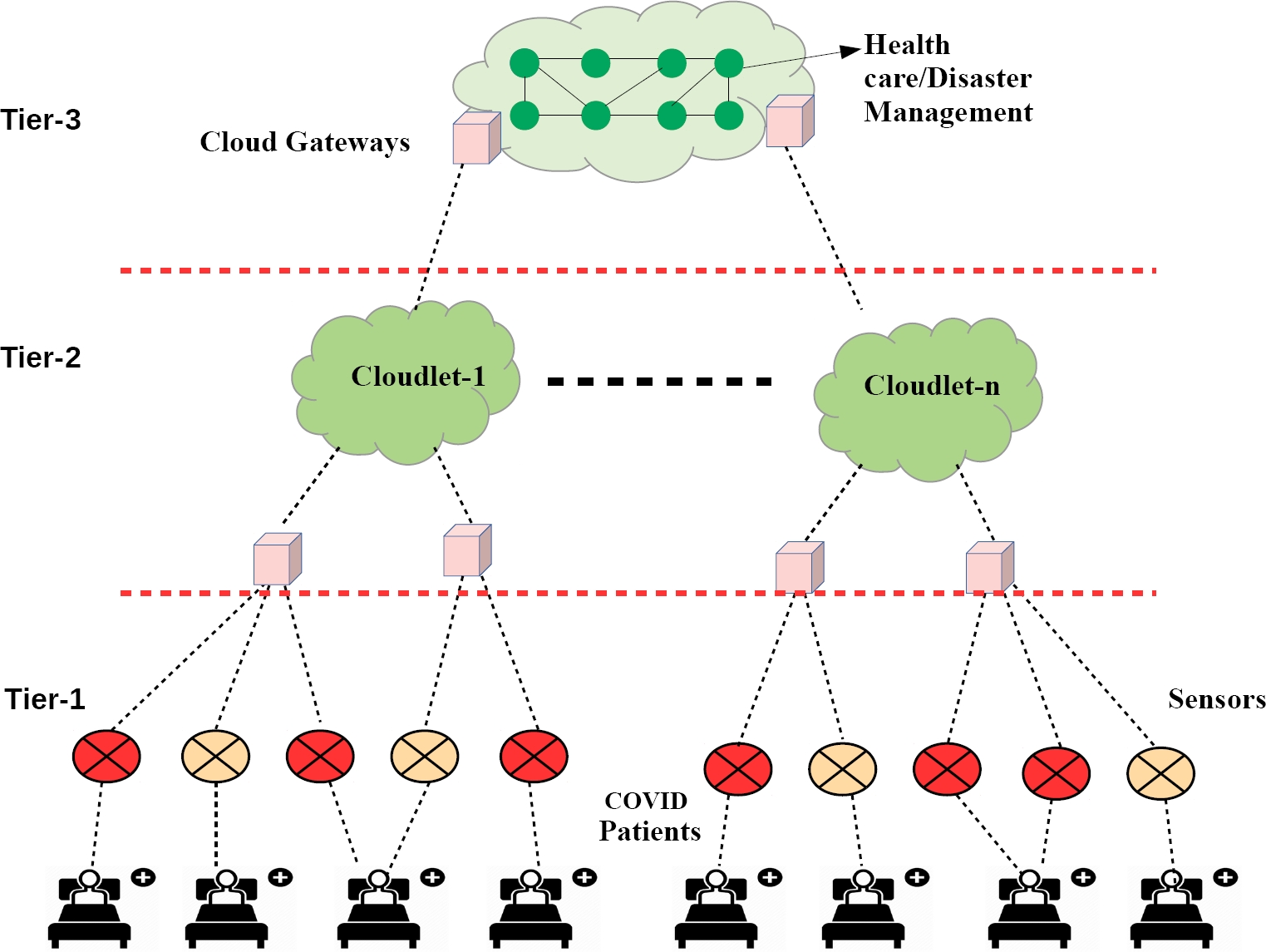
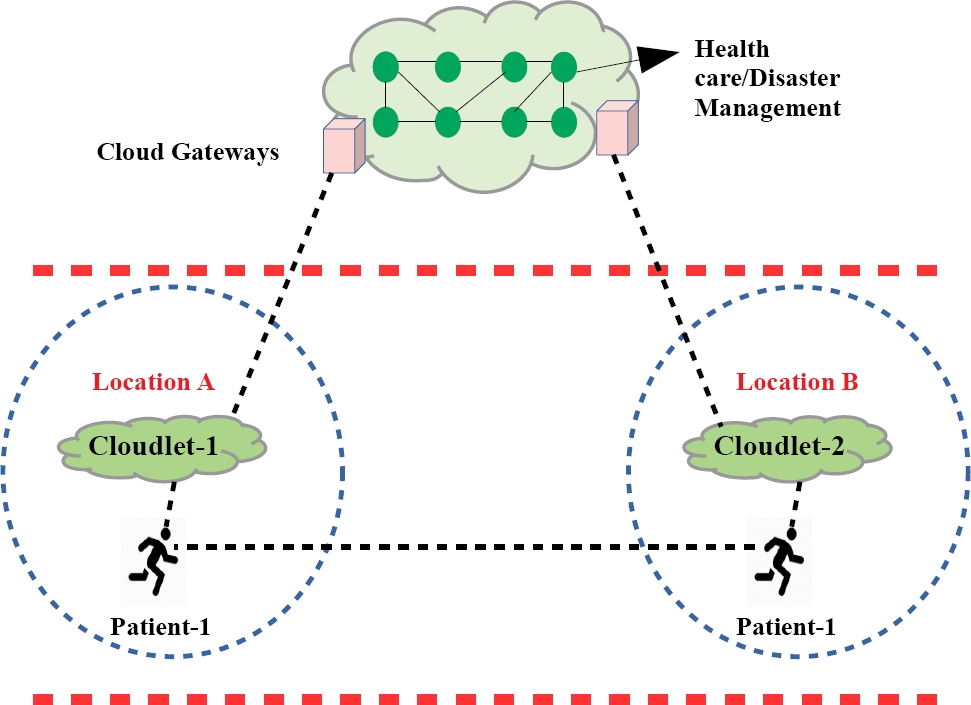
To keep everyone safe, we have come up with an architecture as per in Fig. 2 such that everyone is safe and we can easily detect the COVID-19 patient amoungst us.
The paper is structured accordingly. Related work is provided in Section II. Section III outlines the proposed strategy. Section IV presents the result and analysis. Section V concludes the paper.
2 Related Work
The primary purpose behind this Body Sensor Network (BSN) aimed to use the innovation associated to support the advancement of ubiqui-tous detecting in wellness program, athletics and various scenarios, which would involve ’ubiquitous’ or ’pervasive’ tracking in outpatient and outpatient fields of the biological, anatomical and biomedical criterion [21]. BSN thus aims primarily at customized tracking systems, that serves a variety of uses including serious illness prevention and treatment of aged adults along with competing sports success assessment.
The Internet of Things (IoT) is projected that provide transformative consequences throughout business as well as environment, with IoT linked systems predicting 20.8 billion by 2020 [9]. In order to enable the collecting and sharing of data, the IoT aims to link several specific entities like cars, consumables, houses, ecological detectors etc.
The scale for total IoT industry has been expected to expand between 157.05 billions USD in 2016 to 661.74 billion USD by 2021, a development led towards the expansion of cleverer, yet cost-efficient sensors , cloud computing, and fast broadband convergence and expansion [10]. Latest research in Wireless Sensor networks (WSNs) [31, 32, 33, 34, 35] along with the creation of effective network typologies as well as numerous uses, inclusive of clinical scanning [12, 11]. is substantially important. Digital supervisions having often gained attention [13] the innovation has increasingly expanded the ability to track patients within the region.
Intelligent households including a set of sensors will constantly track critically ill [14, 23] but even these costly equipment does not necessary to control patients at homes. The remote control program for health care enabled by IoT provides several advantages than traditional surveillance model [15]. IoT systems will perhaps utilized for remote medical surveillance for persistent illnesses and cardiovascular (CVD) patients [16], whereas long-duration electrocardiogram ( ECG) tracking was introduced in the housing environment [17]. Present issues require a comprehensive redesign for the public health infrastructure [17], with a view to provide a realistic dream of a pervasive healthcare IoT WSN [36, 37, 38, 39] the economical feasibility of these networks is being investigated and tested [19].
In the Guangdong clinical assistance units a report by the Guangdong Region Welfare Committee revealed details about the operation of 2431 medicare staff [24]. Within their units, nurses accounted for ( 60%), led by skilled practitioners for ( 30%). 50 percent of the clinics with workplace credentials are deputy chief doctors and a expert in ventilation and vital medication (27.6) of 25%. During 2003, 5.8% (140/2431) of healthcare staff were implicated in the epidemic of serious acute breathing illness [24]. Previously Wu et. al. has told in medicare environments that issues subject to COVID-19 IPC illustrate medicare employees’ personal security [25].
However the new coronavirus remains its attacks worldwide, the entire country faces the collapsing markets and plummeting victims. Tragically, thousands of individuals continue to be threatened with disease, and the condition will not improve over the next few weeks. Nevertheless, several scientific solutions have arisen to counter the consequences following the COVID-19 outbreak. New innovations such as IoT, AI, block-chain, and innovative broadband technologies [30], [8] such as 5G were among-st it towards the cutting edge [3]. Digital technology could have a crucial part in strengthening the medical health care system for the COVID-19 outbreak, as per the who as well as the Centers for Disease Control and Prevention (CDC) [4].
The Internet of Medical Things (IoMT) is a mixture of clinical equipment and technological programs which provides comprehensive clinical facilities related towards the IT processes of medicare. IoMT has seen an improvement with the amount of certain possible implementations in modern history close to IoT [5]. The said rise is because a growing amount of smartphone phones is currently fitted with Near Field Communication (NFC) persons that enable such technology to connect to IT Scenarios [6]. IoMT implementations involve: (1) medical control through distant venue, (2) drug monitoring requests; and (3) wearable devices to the healthcare provider associated. The medical field has recognized a revolutionary power of IoMT technology [7] as it is capable of effectively gathering, processing, and distributing medical information.
In the midst of the current pandemic COVID-19, many technologists, medical agencies, policy departments and other institutions are seeking to use IoMT resources and minimize the health service workload. COVID-19 is a deadliest disease that has taken a toll on thousand’s of precious human lives world-wide.
Each and every country is battling it in their own way by social distancing, masks,etc. But, the COVID-19 pandemic is here to stay with us for long time. To keep everyone safe, we have come up with an architecture such that everyone is safe and we can easily detect the COVID-19 patient amoungst us. An intelligent mask which is used in this proposed work can support to the COVID-19 patients/doctors/nurses when they are supposed to close each other.
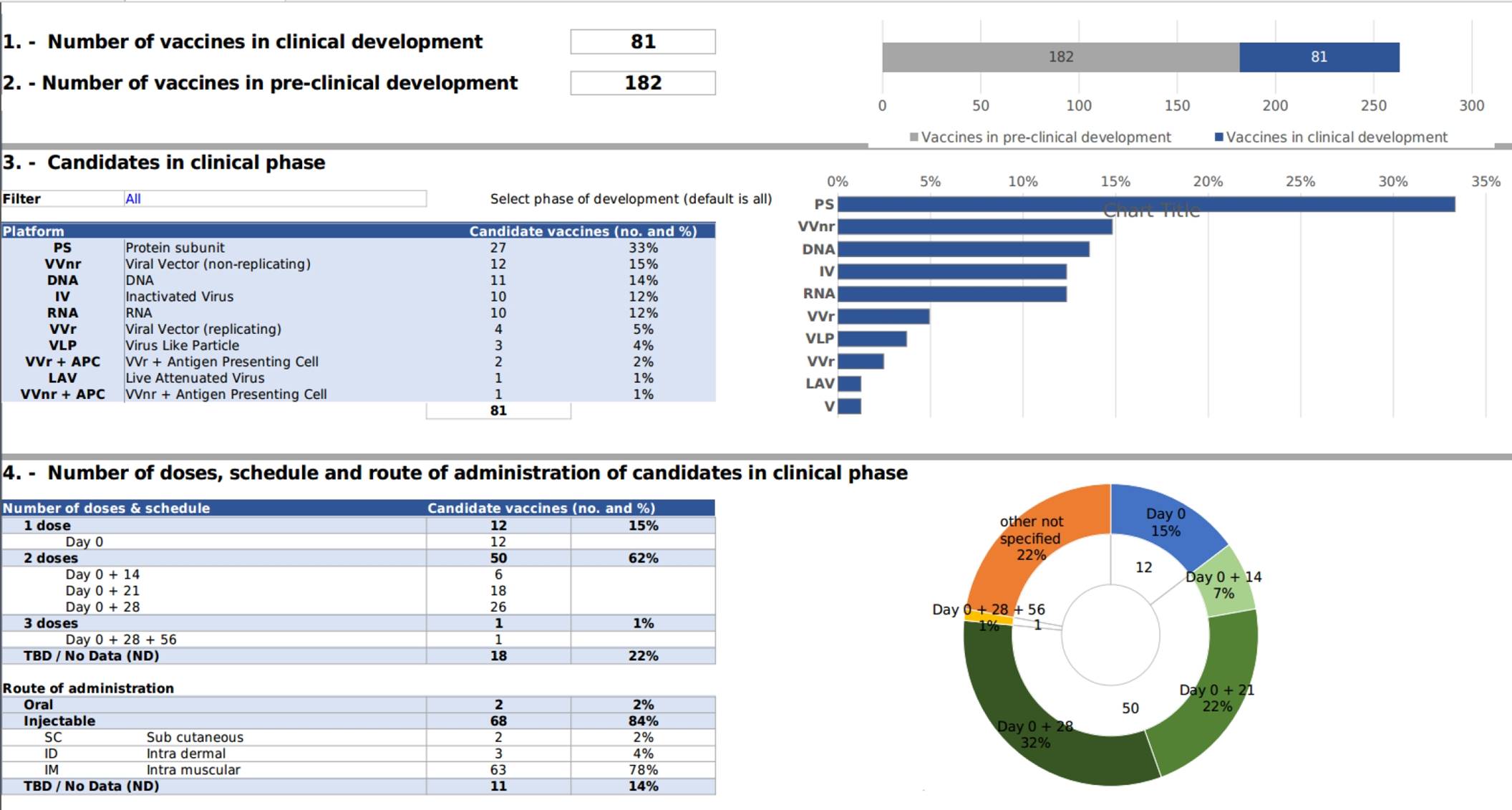
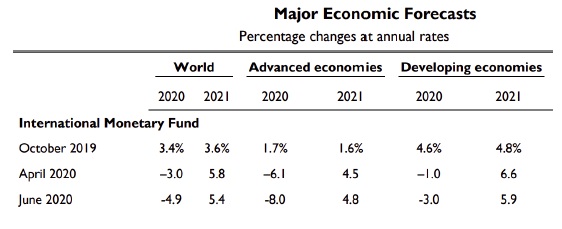
As per Fig. 4, the complete vaccination is not done throuhout the world. So there is a need of propoer social distancing and innovative mask for everyone to protect from covid-19. As per Fig. 5, the world economic also hugely affected due covid 19.
3 Proposed Approach
Day by day, COVID-19 patients are increasing all over the world. The virus often spreads rapidly by highly contagious respiratory droplets from persons with respiratory symptoms while beyond the 1-meter physical distance of infected citizens. However, because physicians and nurses interact with patients constantly in order to monitor health details such as body temperature, cholesterol, blood pressure (BP), and so on whereas there is a chance that the infection may easily get infected.
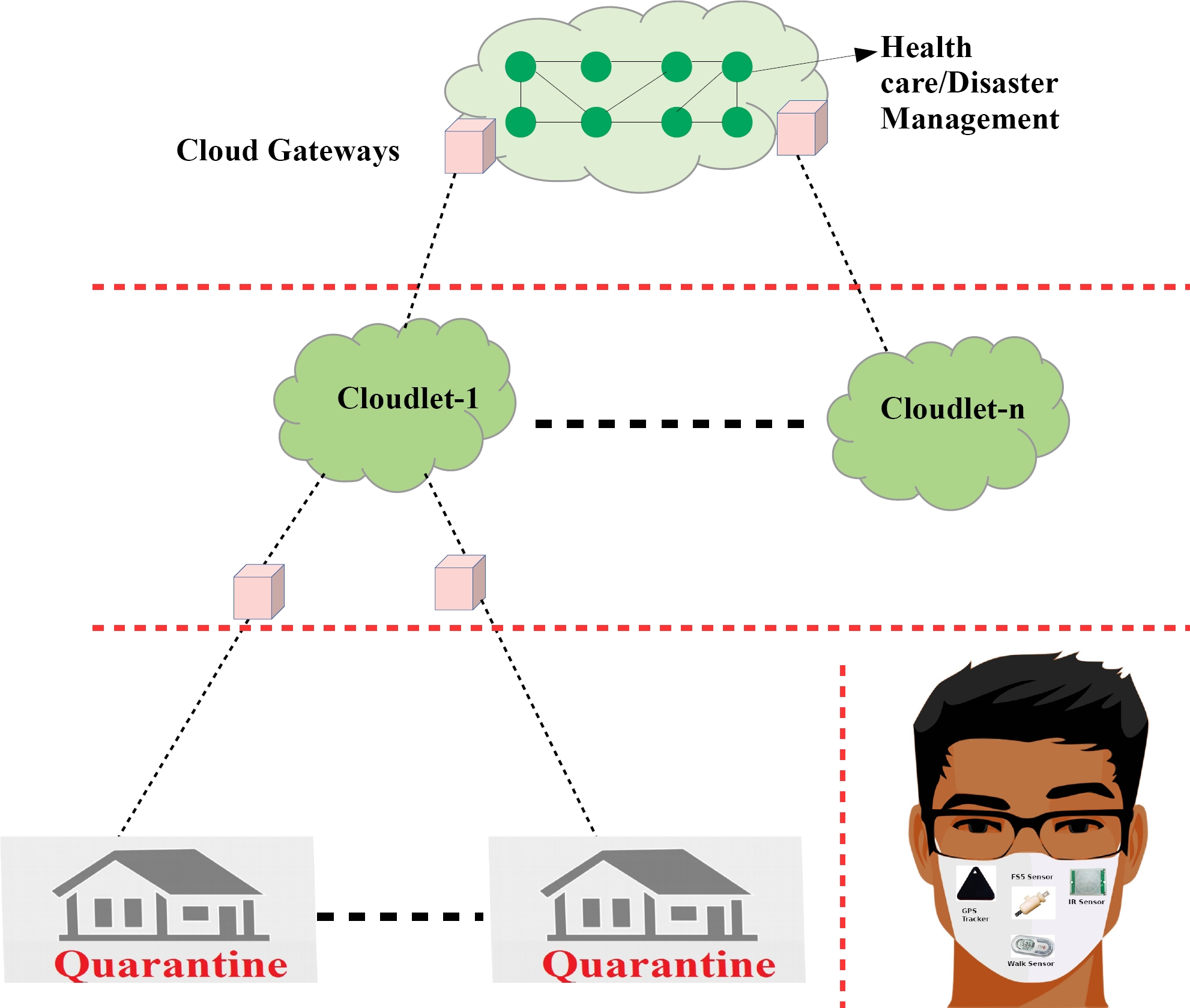
Because of the extremely low number of hospital rooms, physicians and nurses available relative to patients, the patients cannot be assisted for a long period if they are infected. To solve this problem, the proposed approach as shown in Figs. 2 and 3 uses intelligent masks. In this work, we consider two scenarios i.e. scenario A (patients are quarantined at home/hospital) and scenario B (patients travel outside). The architecture is designed in terms of 3 tiers: Tier-1, Tier-2 and Tier-3.
In Tier-1, the patients use SensMask, which consists of multiple sensors as shown in Fig. 3, to assess the health details. Tier 2 includes the local cloudlets in the home/hospital itself. In Tier-3, the cloud with healthcare and disaster management module is available.
Cloud gateways are connected to all three tiers. According to our proposed method, health information for the COVID-19 patient has also been captured by SensMask and transmitted to the local cloudlet through cloud gateways. The cloudlet performs basic operations and transmits to the cloud through cloud gateways. The healthcare and disaster management module in the cloud analyses the data gathered and makes the decisions required to take appropriate steps.
The doctors will even look at the health details from cloudlet obtained by SensMask and initiate required rescue operations. In accordance with our proposed approach, the regular contact between doctors and nurses with patients is decreased which helps to protect them.
The people in home/hospital quarantine need to obey guidelines provided by WHO during COVID-19 pandemics. The rules given by WHO are as follows: (i) everybody should maintain a physical distance of 1 m from each other, (ii) everybody at all occasions will wear the mask, (iii) They shouldn’t travel away from home/hospital.
This is not regulated by the government everywhere in country because of its large population. In order to track everybody, an appropriate model is required. As shown in Fig. 3 we suggest a SensMask for all who are quarantined at home/hospital. This mask is made up of the FS5 thermal mass flow sensor [27] which uses thermal transfer technique to determine the air flow.
The sensor is extremely responsive between 0.2 and 3 m/s, an benefit for low breathing detection [27].
This mask often includes an IR proximity sensor, to decide whether or not a individual is following 1m of social distance [28]. If not, alarm will be produced. After 3 alert warnings, a notification is also sent to the nearest police station. For this, a GPS tracker sensor is mounted in the mask. This GPS sensor often monitors whether the individual is at home/hospital or without permission going outside. The distance travelled by person/day is measured by a walkway sensor. Such person health data are regularly recorded and stored in the nearby local home/hospital cloudlet accessible by the mask.
In the cloudlet itself the data has been processed if it is small enough to process it, otherwise the information is sent to the cloud if the home/hospital cloudlet is not adequate. As shown in Fig. 6, when the people are roaming outside, it checks any cloudlet available nearby or not.
It transmits to the cloudlet if it is there. All trans-missions are carried out through gateways. The cloud will process the data and produce reports to take necessary steps by the authority. On the basis of the report processed, the government will place these people under quarantine check if they are infected.
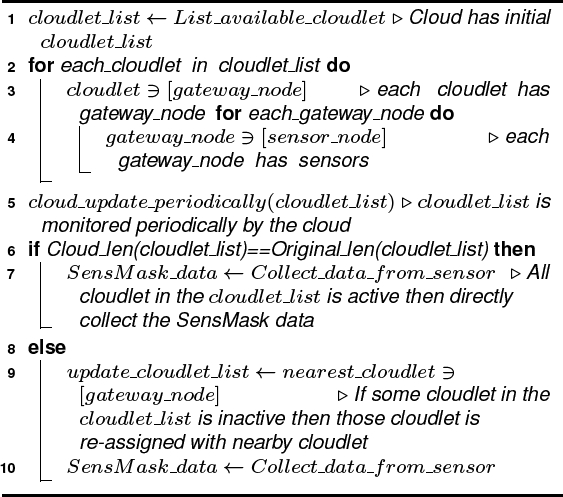
SensMask Algorithm
The proposed SensMask Algorithm is presented in algorithm 1. The cloud periodically collects the available cloudlets and stored in cloudlet list (Line 1). The cloud gateways are assigned for each cloudlet in the cloudlet list (Line 3). As well as for each gateway node, the sensor nodes are assigned (Line 5). The cloud checks the cloudlet list periodically (Line 6) and if all the cloulets are active then it collects the pateints health data from various sensors using intelligent mask (Line 8). If any of the cloudlet is inactive then nearby cloudlet is assigned by cloud (Line 10) and the corresponding gateways are re-assigned. After reassignment, the different sensors in the intelligent mask gather patient health details through the new cloudlet (Line 11).
4 Result and Analysis
We simulated the proposed approach in Python 3.7 with Anaconda 5.3.1 in Ubuntu 18.04 LTS system. The system also has 16GB RAM and 1TB hard disk.
We have considered 50 sensors and sensed information transmitted to the cloud via 15 gateways and ten cloudlets. The cloudlet would immediately be reassigned with the nearest cloudlet if it fails.
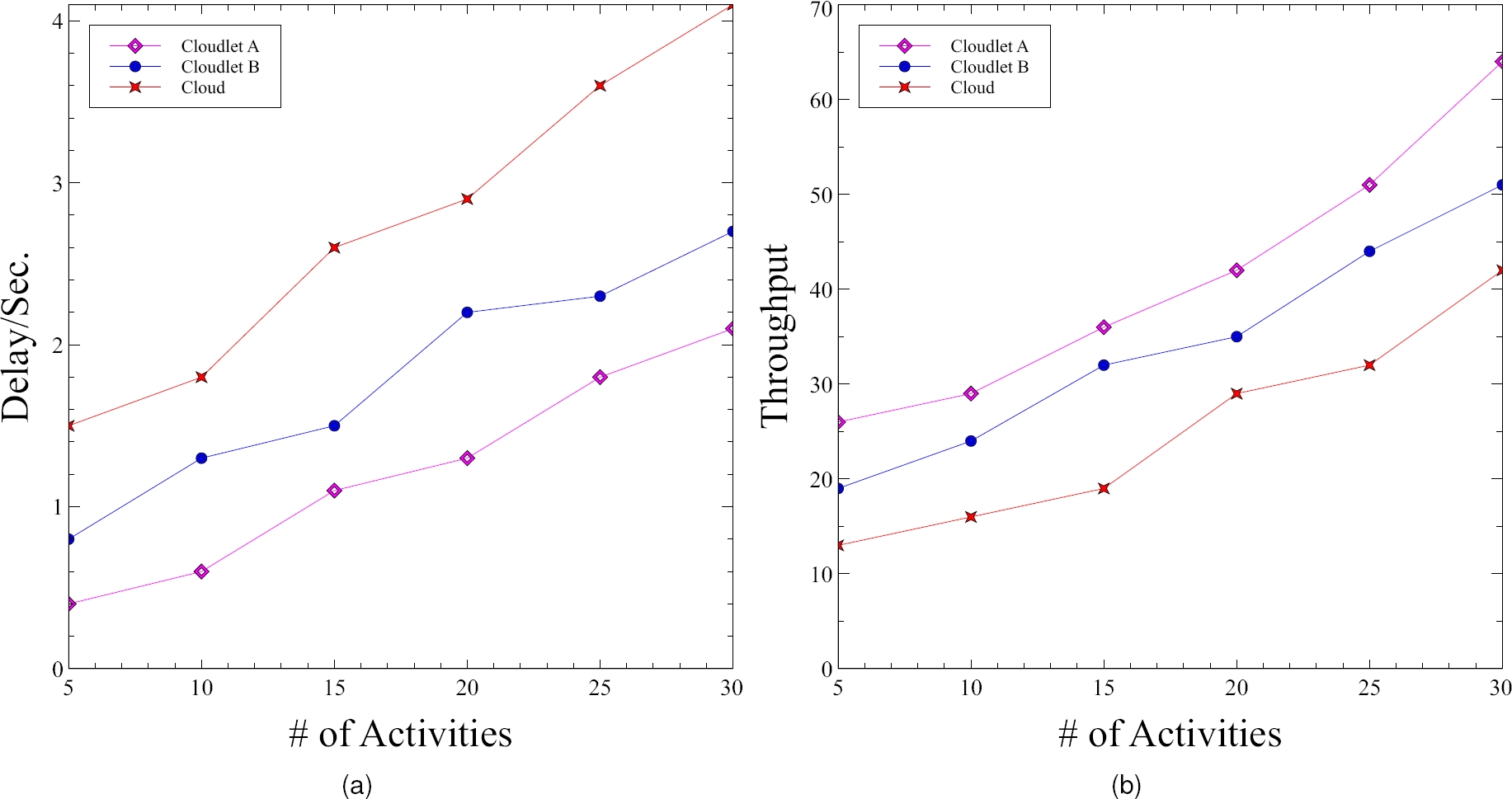
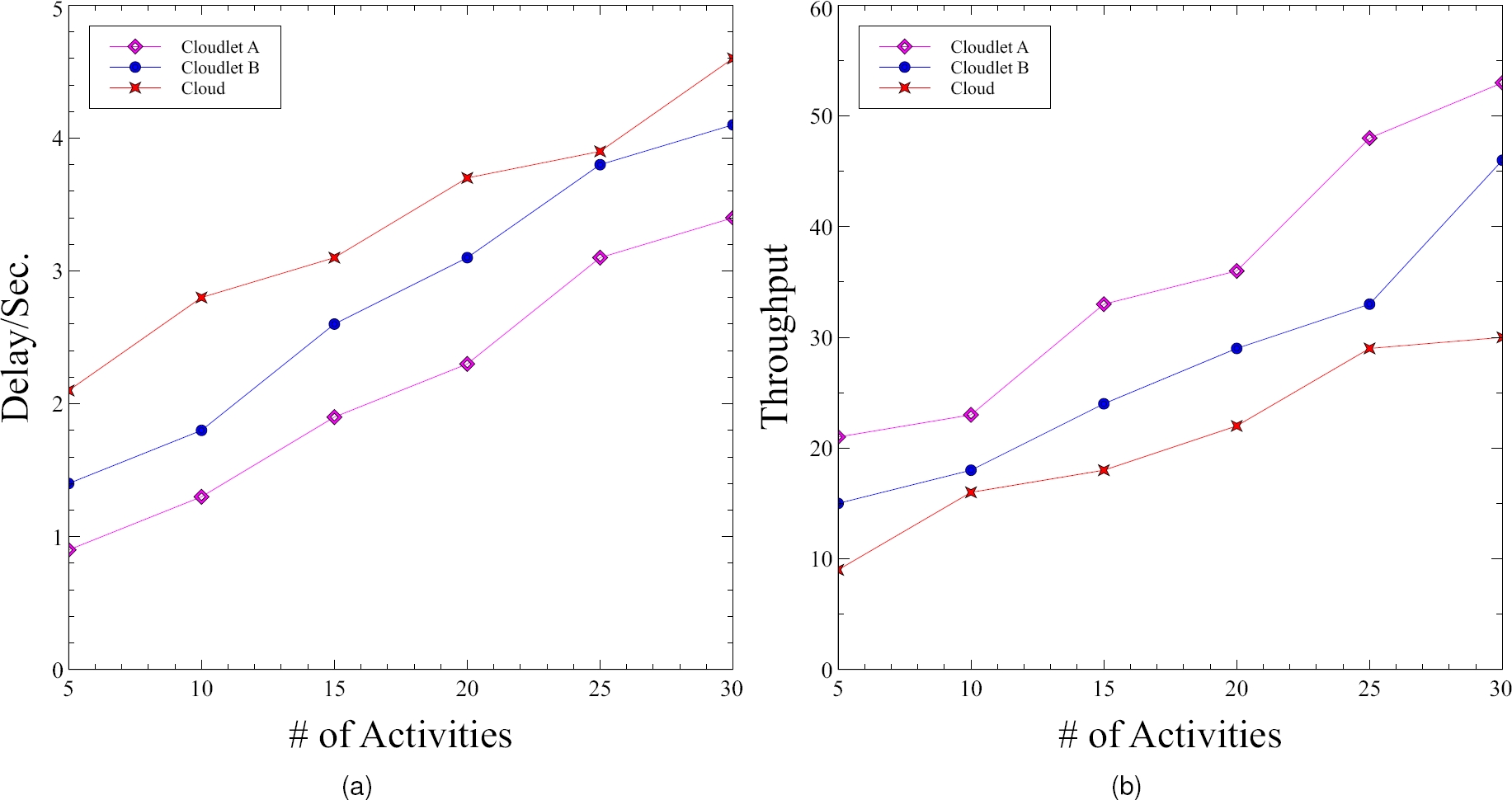
The experimental findings for scenarios A and B are shown in Fig. 7 and Fig. 8 respectively. The connectivity delay and throughput effects of scenario A are shown in Fig. 7a. and Fig. 7b.
The connectivity delay and the throughput effects of Scenario B are shown in Fig. 8a. and Fig. 8b respectively.
The delay is calculated on the basis of time spent to send sensed data from various sensors to cloudlet and a dedicated cloud.
The throughput is measured as the amount of data received per second by the cloudlet and the cloud from the sensors available in the mask.
In scenario B, the measured delay is greater than in scenario A. This is because, the patients travel outside unexpectedly in scenario B as shown in Fig. 6. The network becomes subjected to elevated traffic when the nearby cloud has to be identified. Similarly, the throughput of scenario A is often higher than that of scenario B.
5 Conclusion
The physicians and nurses, consult patients very closely to assess the health conditions of affected patients and hence there may be the high chance of being affected.
For this, in this work we propose the use of an intelligent mask named as SensMask to solve this issue. This mask contains GPS sensor, IR proximity sensor, walk sensor and FS5 sensor. All patients need to wear this mask to obtain data about their health details. An alarm will be generated if the patients are within 1m distance. Such sensors monitor health data from patients and send it to the cloud through the home/hospital-based local cloudlet.
The cloudlet information is used by physicians for further diagnosis of patients. This eliminates and prevents close interaction between doctors and nurses to patients. From the simulation results it has been observed that the proposed scheme performs significantly well with respect to throughput and delay.











 nueva página del texto (beta)
nueva página del texto (beta)