INTRODUCTION
Acute kidney injury (AKI) is common in severe coronavirus disease 2019 (COVID-19). The reported incidence of AKI in subjects hospitalized for COVID-19 varies from 20% to 46%1-3 with variations between institutions. At our center, we previously reported that 30% of the population with severe COVID-19 developed AKI during their hospitalization, 19% corresponding to community-acquired AKI, and 11% to hospital-acquired AKI4. In critically ill patients, the incidence of AKI is higher, reported between 50% and 90%, with variations in accordance to the population included and the temporality relative to the pandemic evolution1-3,5. In most reports, the critically ill population is composed of patients who are managed in the intensive care unit (ICU) with invasive mechanical ventilation (IMV) as well as patients managed with non-invasive oxygen delivery devices. When limited to patients under IMV, the incidence of AKI may reach up to 90%1. Moreover, a decrement in AKI has been reported as the pandemic evolved and there is better knowledge of the disease3.
The pathophysiology of AKI in critically ill COVID-19 patients is not fully known. Several mechanisms are possibly involved, including direct parenchymal invasion by the SARS-CoV-2, microthrombosis, an imbalance in the renin-angiotensin-aldosterone system, hemodynamic instability, inflammatory cytokines, and the indirect effects of therapeutic maneuvers (nephrotoxic drugs and high positive-pressure IMV), among others6,7.
The RECOVERY trial demonstrated that the use of dexamethasone (DXM) 6 mg per day for 10 days improved the 28-day mortality and decreased the need for kidney replacement therapy (KRT) in severe COVID-19 patients requiring supplementary oxygen8. The previous reports have suggested a potential decrease in the incidence and severity of AKI with the use of glucocorticoids9-12. Most of these reports preceded the standardized use of glucocorticoids as employed in the RECOVERY trial.
This study aimed to evaluate the association between the standardized DXM therapy and the incidence of AKI in severe COVID-19 patients treated with IMV in the ICU.
MATERIALS AND METHODS
This is a single-center, prospective, and observational cohort study performed at a referral center in Mexico City. The study was approved by the Local Human Research and Ethics Boards (reference NMM-3325-20-20-1). Due to the health contingency, on admission to the hospital, patients signed a generic informed consent to participate in observational studies. This study is reported in accordance to the STROBE guidelines.
We included all consecutive adult patients, with a positive polymerase chain reaction test for SARS-CoV-2, who were admitted to the ICU and managed with IMV from March 2020 to January 2021. We excluded patients who were transferred to another hospital, those with previous history of advanced chronic kidney disease (eGFR below 30mL/min/1.73m2), prior kidney transplantation, patients who already had clinically evident AKI at admission, and patients who remained hospitalized by January 31, 2021. All data were obtained from a local COVID-19 database that included prospectively collected data from the first COVID-19 patient admission to the date of finalization of the study. All patients were followed up to their discharge. Those patients who required KRT during their hospitalization were contacted to define if they recovered their kidney function by January 31, 2021.
The collected variables included demographic data, comorbidities, home medications, clinical findings at presentation, the laboratory parameters at presentation and at the start of the IMV in the ICU, chest CT-scan findings, use of vasopressors, AKI development, and medications administered during the ICU stay, and patient outcomes. DXM administration was standardized at 6 mg intravenously per day for a total of 10 days and started from the 1st day of patient admission. DXM administration was based on the treating physician decision before August 2020, and to all hypoxemic subjects thereafter, unless contraindicated.
Variable definitions
AKI was defined and staged according to the Kidney Disease Improving Global Outcomes (KDIGO) guidelines by the serum creatinine (SCr) criteria, urine output was not registered13. Patients were staged according to the highest AKI degree attained during their hospitalization. Severe AKI was defined as AKI KDIGO stage 2 or 313. AKI of the early development was defined as AKI diagnosed in the first 48 h of hospitalization (also known as "community-acquired" AKI). AKI of late development was defined as AKI diagnosed after 48 h of hospitalization (also known as "hospital-acquired" AKI). Baseline SCr was defined as the mean SCr value in the 6 months before hospitalization, or the minimum SCr value obtained during hospitalization if the previous values were unavailable14. For the latter, most SCr values corresponded to SCr at admission. As potential factors contributing to AKI, we registered the strategy of ventilation in prone position, the use and dose of vasopressors, concomitant antibiotic and antifungal therapy, and exposure to intravenous contrast. The Charlson Comorbidity Index was calculated to synthesize comorbidities information15.
Outcomes
The primary outcome was to evaluate the association of DXM treatment with the incidence of AKI, and that of severe AKI13. Considering a 60% incidence of severe AKI, a study power of 90% and 95% confidence, we estimated that 231 patients with and without DXM therapy would be required to detect a 15% difference in the incidence of severe AKI between groups. As secondary outcomes, we explored the association of DXM treatment with patient mortality, length of hospitalization, and AKI recovery. The length of hospitalization and AKI recovery is reported for surviving patients. Recovery from AKI was operationally defined as a reduction in peak AKI stage to a SCr level below 1.5 times the baseline16.
Statistical analysis
For continuous variables, their distribution was assessed by the Kolmogorov–Smirnov test. Descriptive statistics are expressed as number (percentage) and median (interquartile range) as appropriate. Baseline patient characteristics between those were or were not managed with DXM, those with or without AKI, and among AKI stages, were analyzed using the U-Mann–Whitney or Kruskal–Wallis test, as appropriate. Chi-square or Fisher’s exact test was used for categorical variables.
To determine the factors associated with AKI and severe AKI development, including DXM treatment, all the collected variables were evaluated by univariate logistic regression. All variables with p < 0.05 as well as all factors previously reported to be associated with AKI17 were selected for a multivariable analysis. After detecting variable collinearity and interactions, we determined the best parsimonious model by comparing each model by the log-likelihood ratio test. As a subgroup analysis, we performed a stratified analysis in the groups of the early- and late-development AKI.
The factors associated with patient survival were evaluated by a univariate and multivariable Cox regression analysis. The date of death were available in all cases, the rest of patients were censored at the time of discharge from hospitalization. All variables with p < 0.05 in the univariate analysis and other factors with known association with mortality18 were included in the multivariable Cox regression analysis. As a sensitivity analysis, we evaluated the effect of the interaction between DXM treatment and severe AKI in patient mortality. The best predictive models were selected using the log-likelihood ratio test.
For all variables, there were <1% missing values, and for missing data, variables were imputed using multiple imputations (randomness was verified and imputed according to corresponding to mean or median). All statistical tests were two-sided, and p-value below 0.05 was considered statistically significant. All analyses were performed using SPSS 24.0 (IBM, Armonk, NY, USA) and GraphPad Prism 6.0 (GraphPad Software, San Diego, CA, USA).
RESULTS
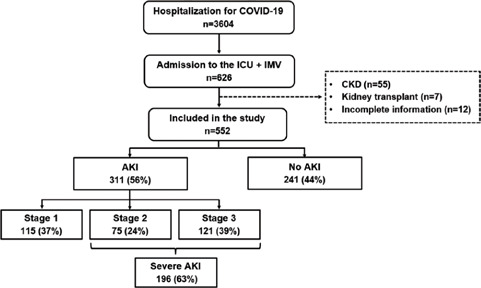
From March 1, 2020, to January 31, 2021 a total of 3604 patients were admitted to our institution for severe COVID-19. Among them, 552 patients were admitted to the ICU and managed with IMV (Fig. 1). The baseline characteristics of all the patients included in this study are provided in table 1 and supplementary table S1. The median age was 53 years (IQR 44-63), 388 (74%) of the population was male, the median Charlson index was 1 point (IQR 0-2), and the median days with COVID-19 symptoms before admission to hospitalization was 8 (IQR 6-10). The median SCr at admission to hospitalization was 0.73 mg/dL (IQR 0.60-0.90). All patients were admitted to the ICU an initiated on mechanical ventilation at a median of 1 day (IQR 1-39) after admission to hospitalization, with a median SOFA score of four points (IQR 4-6) and PaO2/FiO2 (P/F) ratio of 107 (82-147). A total of 371 (71%) were ventilated in prone position, 462 (86%) received vasopressor support, with a peak dose of norepinephrine >0.1 ug/kg/min in 139 (27%). Among the 552 patients included in this study, 267 (48%) received treatment with a standardized DXM regimen, which was started at a median of 0 days (IQR 0-1) after the initiation of IMV. Of those who did not receive DXM, 121 (42%) were included before the change in the institutional protocol to include DXM as therapy for COVID-19. The median follow-up of this cohort was 20 days (IQR 13-30).
Table 1 Clinical characteristics of the total cohort and according to dexamethasone exposure
| Variable | Total (n = 522) | Dexamethasone (n = 267) | No dexamethasone (n = 285) |
|---|---|---|---|
| Demographics | |||
| Age, years | 53 (44-63) | 55 (46-64) | 52 (43-61) |
| Male, n (%) | 388 (74) | 187 (70) | 201 (71) |
| Previous medical history | |||
| Diabetes, n (%) | 151 (27) | 71 (27) | 80 (28) |
| Hypertension, n (%) | 152 (28) | 76 (29) | 76 (27) |
| Obesity, n (%) | 252 (48) | 120 (45) | 132 (46) |
| Chronic kidney disease, n (%) | 13 (2) | 4 (2) | 9 (3) |
| Charlson index, points | 1 (0-2) | 1 (0-2) | 1 (0-2) |
| Use of RAAS inhibitors, n (%) | 115 (21) | 58 (22) | 57 (20) |
| Baseline serum creatinine, mg/dL | 0.73 (0.60-0.90) | 0.71 (0.60-0.85) | 0.77 (0.60-0.95) |
| Admission to emergency room | |||
| Days with symptoms | 8 (6-10) | 8 (5-10) | 8 (6-10) |
| Mean arterial pressure, mmHg | 90 (82-100) | 90 (82-99) | 91 (82-100) |
| Respiratory rate, bpm | 32 (26-40) | 32 (25-38) | 32 (26-40) |
| Oxygen saturation, % | 74 (60-85) | 74 (60-84) | 74 (58-85) |
| NEWS score, points | 8 (7-9) | 8 (7-9) | 8 (7-10) |
| Initiation of mechanical ventilation | |||
| Days admission to IMV | 1 (1-3) | 1 (1-3) | 2 (1-3) |
| SOFA score at IMV initiation | 4 (4-6) | 4 (4-6) | 4 (3-7) |
| Leukocytes, ×1000/mm3 | 10.9 (8.4-14.4) | 10.9 (8.4-15.1) | 10.9 (8.5-13.9) |
| Lymphocytes, × 1000/mm3 | 6.3 (3.7-9.3) | 5.3 (3.2-8.1) | 7.0 (4.3-10.3) |
| N/L ratio | 13.9 (8.9-24.4) | 16.6 (10.5-28.5) | 12.5 (8.0-21.4) |
| Hemoglobin, g/dL | 14.6 (13.2-15.8) | 14.8 (13.3-16.0) | 14.5 (13.1-15.7) |
| Platelets, ×100/mm3 | 265 (205-343) | 273 (208-359) | 256 (205-332) |
| Serum glucose, mg/dL | 142 (113-194) | 154 (122-203) | 133 (102-185) |
| Initiation of mechanical ventilation | |||
| Serum creatinine, mg/dL | 0.87 (0.70-1.22) | 0.86 (0.68-1.10) | 0.89 (0.76-1.20) |
| Serum albumin, g/dL | 3.0 (2.7-3.3) | 3.0 (2.7-3.4) | 3.0 (2.8-3.2) |
| Total bilirubin, µmol/L | 0.70 (0.54-0.92) | 0.69 (0.54-0.93) | 0.70 (0.54-0.89) |
| ALT, UI/dL | 34 (24-56) | 33 (23-53) | 35 (26-58) |
| AST, UI/dL | 39 (28-59) | 36 (26-52) | 44 (32-66) |
| Sodium, mEq/L | 138 (135-141) | 138 (135-140) | 138 (135-141) |
| Potassium, mEq/L | 4.3 (3.9-4.6) | 4.4 (4.0-4.7) | 4.2 (3.9-4.5) |
| C-reactive protein, mg/dL | 17.8 (10.9-26.9) | 17.6 (10.8-26.4) | 18.0 (11.4-27.9) |
| Creatine kinase, U/L | 98 (50-215) | 89 (46-204) | 102 (59-257) |
| Lactate dehydrogenase, U/L | 429 (343-580) | 426 (341-564) | 431 (344-591) |
| Ferritin, ng/mL | 794 (458-1300) | 716 (434-1285) | 861 (500-1300) |
| D-dimer, µg/L | 1513 (841-4340) | 1520 (756-4772) | 1506 (874-3642) |
| Troponin I, pg/mL | 10.7 (5.4-40.4) | 10.6 (4.8-38.7) | 10.8 (6.4-41.7) |
| Abnormal TnI, n (%) | 154 (28) | 78 (29) | 76 (27) |
| Blood pH | 7.36 (7.29-7.44) | 7.38 (7.30-7.45) | 7.35 (7.27-7.42) |
| PaO2/FiO2 ratio | 107 (82-147) | 103 (78-135) | 109 (75-145) |
| Interventions in the ICU | |||
| Mechanical ventilation | 522 (100) | 267 (100) | 285 (100) |
| Prone position | 371 (71) | 187 (70) | 184 (65) |
| Vasopressor | 462 (89) | 221 (83) | 241 (85) |
| Norepinephrine >0.1 µ g/kg/min | 139 (27) | 67 (25) | 72 (25) |
| Days to dexamethasone initiation | – | 0 (0-1) | – |
| Antibiotics | 267 (51) | 126 (47) | 141 (50) |
| Antifungal therapy | 52 (10) | 28 (11) | 24 (8) |
| Intravenous contrast | 50 (10) | 35 (13) | 15 (5) |
RAAS: renin angiotensin aldosterone system; IMV: invasive mechanical ventilation; N/L: neutrophil-to-lymphocyte ratio; ALT: alanine aminotransferase; AST: aspartate transferase.
AKI in critical care COVID-19 patients
AKI was diagnosed in 311 (57%) patients. The AKI stage was Stage 1 AKI in 115 (37%), Stage 2 AKI in 75 (24%), and Stage 3 AKI in 121 (39%) (Table 2). Most AKI developed early during the admission to the ICU and the start of the IMV, with a median 1 day (IQR 0-4) within IMV initiation. The laboratory studies at IMV initiation are also shown in tables 1 and 2. The therapeutic interventions and exposures in the ICU and the outcomes including mortality are shown in table 3.
Table 2 Clinical characteristics of the patients included in this study by AKI development and AKI staging
| Variable | No AKI (n = 241) | AKI (n = 311) | p-Value (AKI vs. no AKI) | Stage 1 AKI (n = 115) | Stage 2 AKI (n = 75) | Stage 3 AKI (n = 121) | p-value (among AKI stages) |
|---|---|---|---|---|---|---|---|
| Age, years | 53 (41-62) | 54 (45-68) | 0.069 | 54 (47-62) | 52 (40-66) | 55 (46-64) | 0.667 |
| Male, n (%) | 167 (69) | 230 (74) | 0.227 | 92 (80) | 51 (68) | 87 (72) | 0.148 |
| Body mass index, kg/m2 | 29.4 (26.6-33.2) | 30.5 (27.6-34.6) | 0.017 | 30.2 (27.9-33.2) | 30.9 (27.6-35.1) | 31.2 (27.3-36.5) | 0.348 |
| Charlson index, n (%) | 1 (0-2) | 1 (0-2) | 0.012 | 1 (0-2) | 1 (0-2) | 1 (0-3) | 0.233 |
| Comorbidities, n (%) | 181 (75) | 256 (82) | 0.039 | 92 (80) | 58 (77) | 106 (88) | 0.134 |
| Diabetes, n (%) | 58 (24) | 93 (30) | 0.127 | 35 (30) | 17 (23) | 41 (34) | 0.246 |
| Hypertension, n (%) | 58 (24) | 94 (30) | 0.108 | 32 (28) | 20 (27) | 42 (35) | 0.383 |
| Chronic kidney disease, n (%) | 3 (1) | 10 (3) | 0.130 | 1 (1) | 4 (5) | 5 (4) | 0.179 |
| SOFA score at ICU admission | 4 (4-6) | 5 (4-6) | 0.024 | 4 (4-5) | 5 (4-6) | 6 (4-7) | 0.002 |
| Kidney function | |||||||
| Baseline SCr, mg/dL | 0.70 (0.60-0.84) | 0.80 (0.60-0.95) | < 0.001 | 0.73 (0.60-0.89) | 0.78 (0.60-0.93) | 0.89 (0.66-1.12) | < 0.001 |
| SCr at IMV initiation, mg/dL | 0.75 (0.65-0.88) | 1.03 (0.86-1.45) | < 0.001 | 1.01 (0.77-1-25) | 1.13 (0.82-1.48) | 1.22 (0.97-1.87) | < 0.001 |
| Peak SCr, mg/dL | 0.88 (0.75-1.06) | 1.92 (1.38-3.25) | < 0.001 | 1.34 (1.18-1.54) | 1.80 (1.42-2.36) | 3.95 (2.82-5.77) | < 0.001 |
| Laboratory at ICU admission | |||||||
| Leukocytes, ×1000/mm3 | 10.5 (8.4-13.5) | 11.4 (8.5-15.2) | 0.049 | 11.4 (8.5-14.7) | 11.3 (8.9-15.9) | 11.4 (8.6-15.4) | 0.864 |
| C-reactive protein, mg/dL | 17.6 (10.8-25.6) | 20.4 (13.9-29.9) | 0.001 | 19.4 (13.2-28.8) | 18.9 (9.8-28.8) | 22.9 (17.1-31.2) | 0.010 |
| Creatine kinase, U/L | 88 (46-160) | 107 (55-283) | 0.002 | 128 (49-303) | 91 (50-276) | 99 (67-243) | 0.869 |
| Lactate dehydrogenase, U/L | 416 (313-557) | 488 (383-650) | < 0.001 | 430 (344-615) | 497 (411-660) | 542 (421-682) | 0.008 |
| Ferritin, ng/mL | 669 (411-1169) | 850 (503-1343) | 0.020 | 912 (535-1381) | 761 (463-1293) | 866 (481-1408) | 0.564 |
| PaO2/FiO2 ratio | 103 (82-145) | 107 (81-147) | 0.812 | 109 (89-150) | 107 (77-146) | 107 (74-145) | 0.309 |
All continuous variables are expressed as median (interquartile range).
AKI: acute kidney injury; ICU: intensive care unit; SOFA: Sequential Organ Failure Assessment score; SCr: serum creatinine.
Table 3 Management in the ICU and patient outcomes by AKI development and AKI staging
| Variable | No AKI (n = 241) | AKI (n = 311) | p-value (AKI vs. no AKI) | Stage 1 AKI (n = 115) | Stage 2 AKI (n = 75) | Stage 3 AKI (n = 121) | p-value (among AKI stages) |
|---|---|---|---|---|---|---|---|
| Mechanical ventilation | 241 (100) | 311 (100) | 1.000 | 115 (100) | 75 (100) | 121 (100) | 1.000 |
| Prone position | 165 (69) | 206 (66) | 0.580 | 70 (61) | 48 (64) | 88 (73) | 0.140 |
| Vasopressor | 205 (85) | 267 (86) | 0.794 | 91 /79) | 64 (85) | 112 (93) | 0.012 |
| Norepinephrine >0.1 µg/kg/min | 83 (34) | 93 (30) | 0.257 | 24 (21) | 20 (27) | 49 (41) | 0.003 |
| Dexamethasone | 149 (62) | 118 (38) | < 0.001 | 52 (45) | 26 (35) | 40 (33) | 0.128 |
| Days admission to start | 0 (0-1) | 0 (0-1) | 0.974 | 0 (0-1) | 0 (0-1) | 0 (0-1) | 0.212 |
| Antibiotics | 136 (56) | 131 (42) | 0.001 | 51 (44) | 24 (32) | 57 (47) | 0.083 |
| Antifungal therapy | 28 (12) | 24 (8) | 0.120 | 10 (9) | 6 (8) | 8 (7) | 0.831 |
| Intravenous contrast | 28 (12) | 22 (7) | 0.065 | 8 (7) | 5 (7) | 9 (7) | 0.977 |
| Outcomes | |||||||
| Length of ICU stay (days) | 13 (9-19) | 15 (11-21) | 0.042 | 12 (10-18) | 12 (10-20) | 20 (15-27) | < 0.001 |
| Length of hospitalization* (days) | 22 (16-31) | 25 (19-36) | 0.003 | 23 (17-32) | 22 (18-31) | 34 (24-43) | < 0.001 |
| Creatinine at discharge, mg/dL | 0.6 (0.5-0.7) | 0.7 (0.6-0.9) | < 0.001 | 0.7 (0.5-0.8) | 0.7 (0.6-0.9) | 0.7 (0.5-1.6) | 0.466 |
| Mortality | 67 (28) | 148 (48) | < 0.001 | 40 (35) | 40 (53) | 68 (56) | 0.002 |
*In patients who were discharged alive after improvement, categorical variables are expressed as number of patients (percentage). Continuous variables are expressed as median (interquartile range).
Forty-six (8.3% of all patients, and 15% of those with AKI) of the 311 patients with AKI received dialytic support at some point during their ICU stay. KRT was administered as prolonged intermittent KRT in 22 (47.8%) subjects, as intermittent hemodialysis (IHD) in 15 (32.6%), and as continuous KRT (CKRT) in 9 (19.6%). The median days from the AKI diagnosis to dialysis initiation were 2 (IQR 1-4). Of those patients who developed AKI and survived to hospital discharge, the median peak SCr was 1.9 mg/dL (IQR 1.4-3.3), with a median SCr at hospital discharge of 0.7 mg/dL (IQR 0.6-0.9).
Factors associated with AKI in critical care COVID-19 patients
The factors associated with AKI development (any stage) were evaluated by logistic regression (Table 4). Age, body mass index (BMI), blood glucose and lactate dehydrogenase at the start of IMV, the SOFA score at IMV initiation, and treatment with DXM were associated with AKI development in the univariate analysis (Supplementary Table 2). In the multivariate analysis, age (Odds Radio [OR] 1.03, 95% Confidence interval [CI] 1.02-1.05), BMI (OR 1.07, 95%CI 1.03-1.10), glucose (OR 1.57, 95%CI 1.21-2.05) and lactate dehydrogenase (OR 1.31, 95%CI 1.17-1.46) at IMV initiation, the SOFA score at IMV initiation (OR 1.10, 95%CI 1.00-1.22), and DXM treatment (OR 0.29, 95%CI 0.20-0.43) were associated with AKI development. We performed a subgroup analysis to evaluate the effect of DXM therapy on AKI of the early development (<48 h from admission, also known as "community-acquired" AKI) and AKI of late development (>48 h from admission, also known as "hospital-acquired" AKI). As shown in supplementary table 3, the effect of DXM was observed in both types of AKI, with a numerically lower OR in AKI of late development (HR 0.35, 95%CI 0.16-0.75 versus HR 0.42, 95%CI 0.25-0.73). The number necessary to treat (NNT) with DXM to prevent one episode of AKI was 4 (95%CI 3-6).
Table 4 Univariate and multivariable logistic regression analysis for AKI and KDIGO stage 2-3 (severe AKI) AKI development
| Variable | Univariate | Multivariable | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | |
| AKI (All stages) | ||||||
| Age, per year | 1.021 | 1.007-1.034 | 0.002 | 1.033 | 1.018-1.050 | < 0.001 |
| Male versus female | 0.795 | 0.547-1.154 | 0.795 | 0.848 | 0.557-1.292 | 0.442 |
| BMI, per kg/m2 | 1.056 | 1.025-1.089 | < 0.001 | 1.066 | 1.030-1.103 | < 0.001 |
| Glucose at ICU admission, per 100mg/dL | 1.480 | 1.179-1.858 | 0.001 | 1.574 | 1.211-2.048 | 0.001 |
| LDH at ICU admission, er 100 UI/dL | 1.251 | 1.132-1.382 | < 0.001 | 1.308 | 1.174-1.458 | < 0.001 |
| SOFA at ICU admission, per point | 1.132 | 1.036-1.236 | 0.006 | 1.101 | 1.003-1.215 | 0.049 |
| Dexamethasone, versus not | 0.378 | 0.267-0.534 | < 0.001 | 0.292 | 0.196-0.433 | < 0.001 |
| AKI KDIGO stage 2 or 3 (severe) | ||||||
| Age, per year | 1.019 | 1.005-1.033 | 0.007 | 1.026 | 1.003-1.049 | 0.029 |
| Male, vs female | 0.891 | 0.606-1.310 | 0.558 | 0.834 | 0.530-1.311 | 0.431 |
| BMI, per kg/m2 | 1.065 | 1.033-1.097 | < 0.001 | 1.078 | 1.040-1.116 | < 0.001 |
| Charlson index, per point | 1.228 | 1.086-1.388 | 0.001 | 1.107 | 0.907-1.350 | 0.318 |
| History of CKD, versus not | 4.235 | 1.287-13.93 | 0.018 | 3.260 | 0.843-12.60 | 0.087 |
| Glucose at ICU admission, per mg/dL | 1.309 | 1.081-1.586 | 0.006 | 1.324 | 1.050-1.669 | 0.019 |
| LDH at ICU admission, per 100 UI/dL | 1.239 | 1.128-1.361 | < 0.001 | 1.335 | 1.202-1.481 | < 0.001 |
| SOFA at ICU admission, per point | 1.220 | 1.115-1.335 | < 0.001 | 1.198 | 1.083-1.326 | < 0.001 |
| Vasopressor, versus not | 1.784 | 1.040-3.059 | 0.035 | 1.762 | 1.014-3.201 | 0.043 |
| Dexamethasone, versus not | 0.392 | 0.272-0.563 | < 0.001 | 0.341 | 0.224-0.522 | < 0.001 |
OR: ods ratio; 95%CI: confidence interval at 95%; BMI: Body Mass Index; CKD: chronic kidney disease; ICU: intensive care unit; LDH: lactate dehydrogenase; SOFA: Sequential organ failure assessment score.
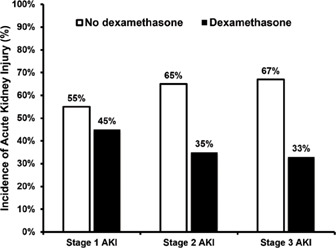
As severe AKI (stage 2 or 3) has been largely associated with an increased mortality, this outcome was also explored by logistic regression (Table 4). Age, BMI, the Charlson comorbidity index, a previous history of chronic kidney disease, blood glucose and lactate dehydrogenase at the start of IMV, the SOFA score at IMV initiation, and the need for vasopressor support were associated with the occurrence of severe AKI in the univariate analysis (Supplementary Table 4). In the multivariate analysis, age (OR 1.03, 95% CI 1.00-1.05), BMI (OR 1.08, 95%CI 1.04-1.12), glucose at IMV initiation (OR 1.32, 1.05-1.67), SOFA score at IMV initiation (OR 1.20, 95%CI 1.08-1.33), use of any vasopressor (OR 1.76, 1.01-3.20), and DXM treatment (OR 0.34, 0.22-0.52) were associated with the occurrence of severe AKI. The incidence of severe AKI was 34% in patients treated with DXM and 66% in those without DXM. Treatment with DXM was associated with a reduced risk of severe AKI development. The NNT with DXM to prevent one episode of severe AKI was 5 (95%CI 3-7). As shown in figure 2, DXM treatment significantly decreased the risk for each stage of AKI. The incidence of stage 1, 2, or 3 AKI was 55%, 65%, and 67% in patients without DXM treatment; and 45%, 35%, and 33% in those who received DXM, respectively. There was no association between the days from admission to the start of DXM treatment and AKI or severe AKI development. As observed for AKI of any stage, the OR for DXM treatment was numerically lower for severe AKI of late development ("hospital-acquired" AKI) than for severe AKI of the early development (OR 0.15, 95% CI 0.07-0.35 versus OR 0.37, 95%CI 0.23-0.39) (Supplementary Table 3).
Factors associated with survival in critically-ill COVID-19 patients
A total of 215 (39%) patients died during the study (Table 3). Of them, 148 (69%) developed AKI during their hospitalization (40 [27%] Stage 1 AKI, 40 [27%] Stage 2 AKI, and 68 [46%] Stage 3 AKI). Among the 46 patients who were managed with KRT, 21 (46%) patients died.
The factors associated with mortality were evaluated by Cox regression analysis. Age, male gender, laboratory parameters at IMV initiation (including serum glucose, albumin, lactate dehydrogenase, and C-reactive protein), the PaO2/FiO2 ratio at IMV initiation, AKI development, use of vasopressor medications, and treatment with DXM were significantly associated with mortality in the univariate analysis (Supplementary Table 5). After adjustment in the multivariate analysis, the occurrence of severe AKI was associated with increased mortality (HR 1.52, 95%CI 1.14-2.02, p = 0.004), while treatment with DXM was associated with lower mortality (HR 0.63, 95%CI 0.48-0.83, p = 0.008). As shown in figure 3A, Stage 1 AKI was not associated with mortality, while severe AKI (Stages 2 and 3) were associated with mortality after adjustment for other covariates.

Figure 3 (A) Adjusted Cox regression plots showing the association between different AKI stages and mortality, and (B) the combined effect of severe AKI and dexamethasone treatment in mortality. Cox regression analysis adjusted for age, sex, serum glucose, albumin, and lactate dehydrogenase levels; PaO2/FiO2 ratio, SOFA at IMV initiation, and use of vasopressors.
The effects of severe AKI development and no DXM treatment in patient mortality were independent and additive in the adjusted survival analysis (Figure 3B). The highest mortality was observed in patients with severe AKI and no DXM treatment. In patients with severe AKI treated with DXM, mortality was significantly reduced (HR 0.63, 95%CI 0.43-0.91) and equivalent to the group without severe AKI and no DXM treatment (HR 0.62, 95%CI 0.41-0.93). The lowest mortality was observed in patients without severe AKI treated with DXM (HR 0.45, 95%CI 0.31-0.64).
Length of hospitalization and recovery of kidney function
In survivor patients, the total days of hospitalization and ICU stay were significantly greater (p < 0.001) in those who developed severe AKI (median 28 days [IQR 20-41] and 16 days [IQR 11-25], respectively) than in those without AKI (median 22 days [IQR 16-31] and 13 days [IQR 9-19], respectively). There was no difference (p = 0.265) in the length of hospitalization between those survivors treated with DXM (23 days, IQR 17-32) and those without DXM (25 days, IQR 18-35).
Among 46 patients who were managed with KRT, 21 (45.7%) died. From the 25 patients who survived, 24 recovered their kidney function by 28 days and 1 by 90 days after hospital discharge. Recovery was observed in patients with and without DXM treatment.
DISCUSSION
COVID-19-associated AKI is a sepsis-induced AKI with high prevalence and treatment is directed to sepsis with no specific protective measures for the kidneys. In this study, we found an AKI prevalence of 56% in COVID-19 patients undergoing IMV, with 36% corresponding to severe AKI. Importantly, DXM treatment was associated with 71% and 66% reduced incidence of AKI and severe AKI, respectively. As previously described, the development of AKI is associated with increased mortality. We found that DXM therapy was associated with a reduction of patient mortality, with mortality rates equivalent to the group of patients without severe AKI and no DXM therapy. The lowest mortality rates corresponded to the group of patients without severe AKI who received DXM consistent with previous studies. This is one of the first large cohorts of COVID-19 patients on IMV to show this significant reduction in AKI episodes and their severity with the use of DXM.
Several studies from multiple centers have reported an elevated incidence of AKI in COVID-19 patients admitted to the ICU, ranging from 30 to 75% for AKI of any stage, 21 to 56% for severe AKI (Stages 2 or 3), and 6 to 39% for AKI requiring KRT19-24. In this study, AKI incidence was well between these ranges: 56% AKI of any stage, 36% severe AKI, and 8% for AKI requiring KRT. An important factor that has been associated with AKI development is the use of IMV22,25,26. For example, in the previous reports from critically ill COVID-19 patients were all patients received IMV5,21, the incidence of AKI was 52-75% and 18-20% for AKI with the need for KRT. AKI in COVID-19 has been associated with the use of high positive pressure ventilation27, although it is not known if this observation is explained by a direct effect of positive pressure ventilation (which can reduce kidney perfusion and glomerular filtration28), or the fact that high-pressure ventilation may be a marker for sicker patients. The high variability in these numbers is explained by the well-reported variation between hospitals23, the different criteria for ICU admission, the timing of the study relative to the pandemic waves5,19, and characteristics of the population admitted to the ICU, among other factors. Several risk factors are associated with AKI in COVID-19, including age, laboratory parameters, interventions such as vasopressors and IMV, and severity scores (SOFA, APACHE-II)22,23,25,29-31. Consistent with the previous reports, we observed an association between increasing age and BMI, laboratory parameters as glucose and LDH, and vasopressor use with the development of AKI and severe AKI.
Noteworthy, we observed that a protocolized DXM regimen was associated with lower development of AKI in mechanically ventilated COVID-19 patients after adjustment for the risk factors described above. Although glucocorticoids are recommended for use in sepsis and septic shock32, their effect in mortality is not consistent among major clinical trials and has not shown an effect in the incidence of AKI33-35. In animal models, administration of hydrocortisone or DXM attenuates kidney damage36-38. Glucocorticoids may improve kidney function through improving cardiovascular function, attenuation of inflammation, and lowering cytokine production, among others39,40.
The timing of administration of glucocorticoids may be critical. A study of sepsis-induced AKI in rodents showed that the effect was better when administered early in the development of sepsis38. In the RECOVERY trial8, DXM was started during the 2nd week of the clinical course of COVID-19, a stage where inflammation plays a determinant role and where the SARS-CoV-2 viral replication may be less relevant. Several cytokines have been associated with AKI in COVID-19, including interleukins (IL) 1 and 6, interferon-gamma, tumor necrosis factor-alpha, and inflammatory pathways such as the complement pathway have been linked to kidney damage41. Therefore, a direct effect of glucocorticoids on inflammation and the consequent improvement in kidney microcirculatory function may aid prevent the development and progression of AKI in COVID-19.
The previous small reports suggested an effect of glucocorticoid treatment on AKI in COVID-19. Lowe et al.,9 described a lower incidence of AKI in a cohort of 81 critically ill COVID-19 patients treated with glucocorticoids. Moreover, Lumlertgul et al.10 observed less AKI progression in subjects treated with glucocorticoids in adjusted analyses. Piñeiro et al.11 reported less AKI with KRT requirement in those treated with glucocorticoids. These initial reports suggested a potential beneficial effect of glucocorticoid treatment in AKI development; however, they were limited by the small number of patients included and the non-protocolized use of glucocorticoids. In the RECOVERY trial8, the number of patients who received KRT was lower in those treated with a protocolized DXM regimen. A recent report from France12 included 100 critically ill COVID-19 patients and where DXM was administered to all patients during the second COVID-19 wave, DXM use was associated with less AKI in the adjusted analysis (OR = 0.31, 95%CI 0.09-0.99). Here, in a larger population and a protocolized DXM regimen, we ascertained that DXM treatment is associated with a 66% (95% CI 48-88%) lower incidence of severe AKI.
AKI is a well-recognized factor associated with mortality in critically ill COVID-19 patients5,23,29,42; therefore, any intervention that decreases AKI incidence would be expected to also decrease patient mortality. As previously demonstrated in the RECOVERY trial and verified in subsequent studies8,43,44, DXM treatment reduces mortality in COVID-19 patients with oxygen requirement, including those undergoing IMV. In this study, we showed that DXM treatment is associated with a reduced mortality in patients with severe AKI, as well as in the group of patients without severe AKI, after adjustment for other risk factors.
Finally, it has also been reported that DXM treatment reduces the length of days under IMV and the length of hospitalization11,20,21,45. We also observed a reduction in these parameters consistent with these studies, although they were not affected by DXM treatment. Kidney recovery was observed in most surviving patients after KRT, with or without DXM treatment. This high percentage is higher than that observed in other series23,45,46 and possibly influenced by the exclusion of patients with advanced previous kidney damage. Still, the SCr-based definition for recovery of kidney function does not account for the loss of the kidney reserve and should be taken cautiously as it has been reported that COVID-19 survivors have a higher risk of eGFR decline, end-stage kidney disease, and major adverse kidney events47.
The strengths of this study include the prospective collection of variables, including the development of AKI and the use of a standardized DXM regimen, which allowed us to isolate a potential role of DXM in modifying AKI severity. There are limitations to this study. As an observational study, some confounding factors associated with AKI development may have not been registered. Therefore, the association between DXM treatment and AKI prevention may be overestimated and it is not possible to establish a causal role. The study did not account for differences in AKI incidence and mortality according to the COVID-19 pandemic waves at our center and the time from the start of the pandemic. We did not register adverse events of DXM therapy to balance the benefit to risk ratio of this therapy. The results from this study should be considered hypothesis-generating and need to be tested in future studies.
SUPPLEMENTARY MATERIAL
Supplementary data are available at Revista de Investigación Clínica online (DOI: 10.24875/RIC.23000034). These data are provided by the corresponding author and published online for the benefit of the reader. The contents of supplementary data are the sole responsibility of the authors.











 nueva página del texto (beta)
nueva página del texto (beta)