Introduction
The laxity of the tissues that delimit the mediastinum allows to harbor large tumors before generating symptoms by compressing neighboring structures such as the tracheobronchial tree, vascular structures and esophagus, producing dyspnea, dysphonia, chest pain and dysphagia. The most common neoplasms of the mediastinum in children are lymphoma, neurogenic tumors, and germ cell tumors. In both asymptomatic and symptomatic patients with mediastinal masses, imaging studies that identify the location to the anterior, middle, or posterior mediastinum will be essential for the initial diagnostic approach.1
Soft tissue sarcomas are rare malignant tumors, representing less than 1% of all malignant neoplasms and specifically in the thorax less than 0.01%. Mediastinal sarcoma accounts for less than 10% of mediastinal tumors and is usually metastatic from sarcomas originating in the extremities, retroperitoneum, head, and neck.2
The average age of diagnosis of sarcomas in the mediastinum is 40 to 50 years, the prevalence in pediatric age is not exactly known due to its infrequency. 70% are spontaneous onset, 13% have a history of radiation to the chest and mediastinum, and 10% have associated hereditary syndromes, such as Li-Fraumeni, Gardner’s syndrome, retinoblastoma, and neurofibromatosis (Von Recklinhausen’s disease).3 Liposarcoma is the most common histological type in the anterior mediastinum, but there are limited data on differences in clinical presentation and treatment outcome between adult and pediatric patients. The objective of this work is to present a case of mediastinal liposarcoma in a pediatric patient.
Case report
A 15-year-old adolescent with a history of cutaneous lupus was admitted with a five-month evolution of asthenia, adynamia, dyspnea on medium efforts and pleuritic chest pain in the right hemithorax, without B symptom. In the study of dyspnea, a contrasted chest computed tomography (CT) was performed: anterior mediastinal mass of 124 × 90 × 87 mm with various areas of soft tissue density and fatty tissue elements, extending posteriorly until compromising the mediastinal fat of the junction between the superior mediastinum and inferior, in contact, without infiltrating the walls of the left venous brachiocephalic trunk, the arch of the azygos vein, the right brachiocephalic artery, the dorsal and middle ventral aspect of the superior vena cava as well as the ventral aspect of the ascending segment of the aorta a level of the arch and the right anterior and medial aspect of the pulmonary artery infundibulum and exerting extrinsic compression without infiltration of the wall at the level of the right atrium, without evidence of metastatic lesions (Figure 1). A biopsy was performed by mediastinoscopy that reports myxoid liposarcoma without a round cell component.

Figure 1: Contrast-enhanced chest computed tomography. Arrow points the mass in anterior mediastinum. A) Coronal plane, B) sagittal plane, C) axial plane.
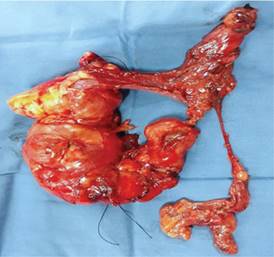
She is taken to surgery for resection of the mass with a sternotomy approach where a solid tumor is identified, lobulated 10.5 × 7.5 × 6.0 cm of yellow and orange color that extended to the anterosuperior and middle mediastinum, firmly adhered to the right pleura, medial mediastinal tract, involving the left venous brachiocephalic trunk, right subclavian vein, superior cava in contact with the anterior and lateral wall of the trachea and around the right main bronchus, without evidence of pulmonary or pleural metastases, no pleural effusion, or mediastinal lymphadenopathy, with adequate plane of separation of the pericardium. Complete resection is achieved macroscopically by resecting the thymus (Figure 2). The surgical bed is marked with titanium clips. Right and left mediastinal drainage catheter was left.
Adequate postoperative evolution, she was extubated and transferred to the ICU for surveillance, analgesic management with opioid, control radiography with adequate position of chest drainage and pulmonary expansion, without the need for transfusion support or vasopressor. On the fourth day she was discharged.
Pathology report: neoplasm composed of adipose tissue with abundant type II and multivacuolated lipoblasts with hyperchromatic nucleolus with less than one mitosis per field distributed in myxoid stroma with spindle cells with minimal atypia which are accompanied by curvilinear vessels. Fragments of lymph node and brown fat can be seen on one side. Immunohistochemical studies are performed S100, CK, CDK4, AML negative, Desmin negative, CD34 positive, p16 focally positive, Ki67 8%. Suggests myxoid liposarcoma without round cell component, mitosis up to 1 × 10 high power fields. Histological grade I, negative margins for compromise, unidentified lymphovascular invasion, no compromised lymph nodes identified.
Patient with stage IB T3N0M0 liposarcoma grade I, R0 resection. Postoperative radiotherapy was offered at a dose of 45 in 1.8 Gy fractions (anterior mediastinum). Follow-up at the institution with chest contrasted tomography every six months, last control was in December 2020, the patient was asymptomatic and without evidence of relapse in images.
Discussion
Mediastinal sarcomas are very uncommon in pediatric age, the most common soft tissue sarcoma is malignant fibrous hyosthiocytoma (24%), followed by liposarcoma (14%).4
Primary intrathoracic liposarcoma only represents 0.1 to 0.75% of all mediastinal tumors, it does not have a predisposition based on sex, and the diagnosis is more frequent in those over 40 years of age.5 Less than 25 cases have been reported in children under 18 years since 1939 (Table 1), with more frequent locations in the anterior and posterior wall of the thorax, all of them undergoing surgical management.6
Table 1: Liposarcoma cases reported in patients under 18 years.
| Author (year) | Age/sex | Location | Treatment | Recurrence | Follow-up |
|---|---|---|---|---|---|
| Perkins (1939) | 18/F | Posterior | Surgery | – | Alive 3 years |
| Joske (1944) | 18/M | Posterior | Surgery | – | – |
| Kauffman (1959) | 2/F | Superior | Surgery | 2 years | Alive 4 years |
| Wilson (1964) | 1/F | Anterior | Surgery | – | Alive 8 months |
| Cicciarelli (1964) | 13/F | Right thorax | Surgery + radiotherapy | 9 months | Died 2 years |
| Cicciarelli (1964) | 15/F | Posterior | 2 Surgery’s | Yes | – |
| Aldor (1979) | 12/M | – | Surgery | – | – |
| Castelberry (1984) | 14/M | Anterior | Chemo/radiotherapy+ surgery | – | Alive 14 months |
| Koster (1985) | 14/M | – | Surgery | – | – |
| Plucker (1988) | 5/M | Anterior | Surgery + chemotherapy + surgery | 10 months | Died 7 months |
| La Quaglia (1993) | 18/M | Posterior | Surgery + chemotherapy + brachytherapy | – | Died |
| Mikkilineni (1994) | 17/M | Posterior | Surgery + chemotherapy | 9 months | Died 9 months |
| Klimstra (1995) | 14/- | Anterior | – | – | – |
| Klimstra (1995) | < 18/- | – | – | – | – |
| Chiyo (2001) | 13/F | Anterior | Surgery | – | Alive 35 months |
| Tian (2002) | 12/M | Left anterior superior | Surgery | – | Died 5 months |
| Hahn (2007) | 14/F | Posterior | Surgery | No | Alive 53 months |
| Hahn (2007) | 3/M | Anterior | Surgery | No | Alive 36 months |
| Hahn (2007) | 7/F | – | Surgery | – | – |
| Rajan (2010) | 11/F | Posterior superior | Surgery | No | Alive 20 months |
| Saeed (2010) | 17/F | Anterior | Surgery + chemo/radiotherapy | – | – |
| Chen (2014) | 16/F | – | Surgery | No | Alive 36 months |
| Zheng (2021) | 14/F | Left thorax | Surgery | – | – |
| Romero (present case) | 15/F | Right anterior superior | Surgery + radiotherapy | No | 3 years |
M = masculine. F = female.
Modified from: Anand Rajan KD, et al.6
Mediastinal liposarcomas can present with rapid growth leading to compression of adjacent structures with typical symptoms such as those presented by the patient. Dyspnea, tachypnea and chest pain, are the most common symptoms, but non-specific, which is why there is a delay in the diagnosis, as in the reported patient who had been experiencing these symptoms for five months. Dysphonia, superior vena cava syndrome, wheezing, arrhythmias and heart failure have been described; 85% of patients have symptoms and 15% are incidental imaging findings.5,7 When the growth is massive, a distinctive clinical entity known as «giant mediastinal liposarcomas» appears, a term that should be used as proposed by Nguyen et al, when the liposarcoma reaches a size greater than 10 cm and is associated with compressive symptoms.5
Histologically, liposarcoma is divided into four large subtypes: well differentiated, myxoid/round cells, dedifferentiated and pleomorphic; 40% to 50% are myxoid liposarcomas as in the reported case. The histological types are correlated with the potential for metastasis, this subtype being the least aggressive and the pleomorphic one having the worst prognosis.4,8
Depending on the degree of differentiation, in the tomography, a mass of fatty tissue with a variable soft tissue component may be evidenced, however these characteristics are not sufficient for diagnosis and a histological study is always required. Various techniques have been used for biopsy of mediastinal masses, ultrasound or tomography-guided biopsy, mediastinoscopy, mediastinotomy and open surgery.9 The most used are image-guided and the decision for that choice is based on tumor size, location and the clinical characteristics of the patient, as reported by Tanaka et al that in order to evaluate safe diagnostic strategies for pediatric patients with respiratory distress caused by mediastinal tumors, they analyzed the records of 12 patients and report different strategies as cytology and flow cytometry of the pleural effusion, if present, core needle biopsy under local anesthesia and tumor markers.7
An R0 (macroscopic and microscopic negative margins) resection is the main independent prognostic factor for disease-free survival and overall survival.3 If the liposarcoma is small, minimally invasive approaches can be considered. The usual management is resection by open surgery, depending on the location the approach can be by sternotomy, anterolateral or posterolateral thoracotomy, clamshell.3 In the cases reported in adults by Jimenez et al, the approach of choice was posterolateral thoracotomy; in our patient, due to the location of the lesion, the best exposure was achieved with a sternotomy. To carry out a complete resection, 34% of cases require resection with reconstruction of larger structures.3
Postoperative radiation therapy is considered the ideal management for almost all intermediate-grade and high-grade soft tissue sarcomas. The recommended radiation dose is 60-66 Gy in fractions of 1.8-2 Gy. Local recurrence develops in approximately 13% of patients with 5-year, 10-year, and 15-year survival rates after surgery and radiation therapy of 79, 69, and 61%, respectively.10 The patient in the present case in a 3-year follow-up after treatment with radiotherapy has not presented relapse.
Conclusion
Mediastinal liposarcoma is a rare entity and more so in the pediatric population, usually at the time of its presentation they are large tumors that require open surgical approaches and the need for resection of infiltrated adjacent structures. The main prognostic factor for disease-free survival is an R0 resection, for which surgical planning and interdisciplinary management are essential for the management of these patients.











 nueva página del texto (beta)
nueva página del texto (beta)