Introduction
Stroke is the second leading cause of both disability and death worldwide, with a higher prevalence in low- and middle-income countries1. Ischemic stroke and other thromboembolic events represent well-known complications of chronic myeloproliferative neoplasms2,3. However, the diagnosis of this hematological disorder in the emergency setting of a stroke represents a challenge2. We present a case report based on first-ever ischemic stroke secondary to embolization from aortic thrombosis. This article highlights the importance of an adequate multi-imaging and multidisciplinary approach in the diagnosis and treatment of ischemic stroke due to aortic thrombosis in myeloproliferative neoplasms patients.
Case presentation
We present the case of a 51-year-old woman with history of obesity (BMI = 39 kg/m2), hypertension, ex-smoker, and chronic oral contraceptive use, who attended the central emergency room of our hospital due to dizziness associated with sudden nausea and vomiting.
On hospital admission (7 h after symptom onset), the patient was hemodynamically stable, evidencing as main positive physical examination signs: hypertension (190/100 mmHg), positive sensitized Romberg sign to the left and left dysmetria. The rest of the physical examination was normal. No relevant abnormalities were found in the admission electrocardiogram and laboratory tests.
Brain diffusion magnetic resonance imaging performed due to presumptive stroke, revealed multiple recent ischemic lesions on both cerebellum hemispheres and at the right parietal lobe level. Given these findings, the event was interpreted as ischemic stroke of probable embolic etiology, so the following studies were carried out to detect the "emboligenic source:" a computed tomography-angiography of the neck and intracranial vessels that showed mild, uncomplicated atheromatosis at the level of the left carotid bulb and brachiocephalic artery, a cardiac 24 h Holter monitoring that did not exhibit significant arrhythmias, and a transesophageal echocardiogram revealing preserved biventricular systolic function, left ventricular wall hypertrophy, mild left atrial dilation, and absence of significant valve abnormalities. At the level of the descending thoracic aorta, 30 cm from the dental arch, a mobile, pedunculated isoechogenic image, 11.8 mm in length and 4.2 mm in anteroposterior diameter, was observed attached to the anterior aortic wall, consistent with thrombus, as no complicated atherosclerotic lesions were observed in the aorta that might lead to suspect a differential diagnosis such as that of debris (Fig. 1). A computed tomography-angiography of the thoracoabdominal aorta performed for presumptive aortic thrombosis evidenced preserved diameter throughout its course and the presence of four pedunculated images attached to the thoracoabdominal aortic wall, compatible with thrombi. In addition, isolated, mild, and uncomplicated atherosclerotic plaques were observed and malignant or infiltrative processes of the aorta were ruled out (Fig. 2A and B).

Figure 1 Transesophageal echocardiogram. Descending thoracic aorta long axis mid-high esophageal view (30 cm from the dental arch) at 12 0 degrees displays isoechogenic, pedunculated image attached to the anterior aortic wall, 11.8 mm in length and 4.2 mm in anteroposterior diameter.
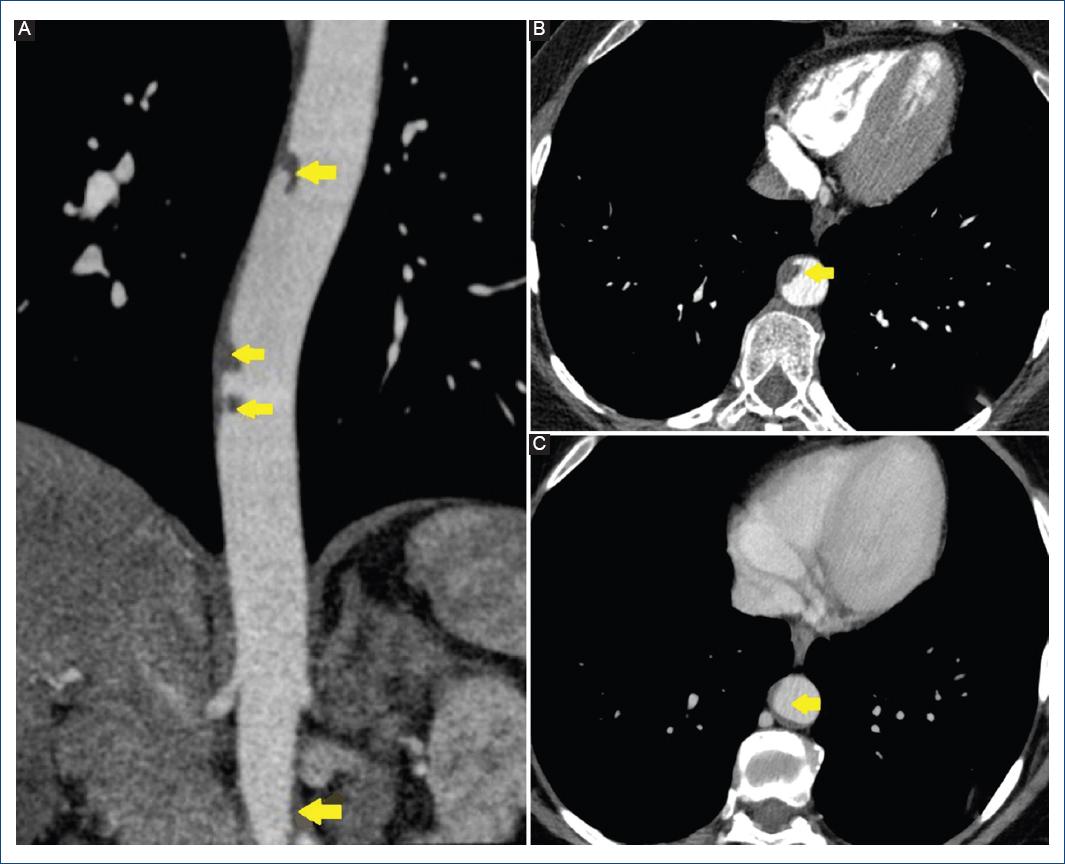
Figure 2 Computed tomography angiography. A: pre-treatment. Multiple luminal thrombi are seen attached to the wall of the thoracic aorta and in visible portions of the abdominal aorta, occupying less than 50% of the vessel lumen (coronal plane). B: pre-treatment. Luminal thrombi attached to the wall of the descending thoracic aorta (axial plane). C: post-treatment. Slight peripheral mural thrombosis, 3.3 mm in thickness, is observed in mid segment of the descending thoracic aorta (axial plane).
The patient started anticoagulant treatment with apixaban at a dose of 5 mg every 12 h, oral contraceptive agents were discontinued and a hematological evaluation was carried out to detect a prothrombotic etiology that might justify the clinical condition. Statins were also indicated, but were not tolerated by the patient.
Thrombophilia studies were all negative (lupus anticoagulant, B2 glycoprotein, anticardiolipin and antinuclear antibodies, antithrombin, protein C and S, prothrombin G20210A mutation, factor V Leiden, and activated protein C resistance). However, a mutation was detected in the tyrosine kinase JAK2 gene (JAK2V617F mutation), so a bone marrow biopsy was performed. Cellular morphological analysis evidenced a chronic myeloproliferative neoplasm, without indication for cytoreductive treatment. In light of this clinical scenario (aortic thrombosis with thromboembolic event and chronic myeloproliferative neoplasm), chronic anticoagulation was indicated. The patient evolved favorably and did not present bleeding complications or any other thromboembolic event after a 2-year follow-up. Subsequent computed tomography controls showed mural small thrombi without free-intraluminal component (Fig. 2C).
Discussion
Chronic myeloproliferative neoplasms are characterized by the clonal expansion of abnormal hematopoietic stem cells. Its pathophysiology shows recurrent molecular defects, mainly represented by JAK2V617F mutation in exon 144. Thrombosis is a complication that frequently has a negative impact on the morbidity and mortality of these patients. The rate of fatal and non-fatal thrombotic events is between 2-4% patient-years and the incidence of arterial events is 2-3 times greater than venous ones3. In these cases, the pathogenesis of thrombosis is the result of a complex interaction between clinical factors (age over 60 years, previous thrombotic event, obesity and atherosclerotic risk factors as hypertension, diabetes, dyslipidemia, and smoking) and disease-related factors (erythrocytosis, leukocytosis and thrombocytosis, as well as the influence of JAK2V617F mutational status and its allele burden)3. In our case, the diagnosis of chronic myeloproliferative neoplasm was obtained from the study of thrombosis in an aorta with preserved diameter and without evidence of complicated atherosclerotic plaques. The patient presented prothrombotic risk factors in the clinical scenario of this hematologic neoplasm: obesity, hypertension, JAK2V617F mutation, as well as oral contraceptive use3.
Few reports and case series of thromboembolism originating in a thoracic, non-aneurysmal aorta have been published since the first case described in 1967 by Oliver et al.5 As in our patient, peripheral embolism was the initial clinical manifestation in most cases6. In our case, although thrombi were found in the descending thoracic and abdominal aorta, which theoretically would not justify a cerebral embolism, we could not rule out thrombosis in the aortic arch that could not be detected after embolization. The etiology involved in thrombus formation in a macroscopically normal aorta is not clearly understood. However, in these cases, genetic and thrombophilic factors have been associated with thrombus formation7. In the past 10 years, the incidence of aortic thrombosis has increased due to the growing development of different techniques in the field of multimodality cardiovascular imaging. Both transesophageal echocardiography, as computed tomography and magnetic resonance angiography have adequate diagnostic sensitivity, considering that the former has as limitation hindering the evaluation between the distal ascending aorta and the proximal aortic arch due to tracheobronchial interposition6. Due to the low number of cases, the treatment of aortic thrombosis is controversial, and different strategies are postulated7. In general, optimum management depends on thrombus morphology and location, symptoms, presence of procoagulant factors, and the general condition of the patient. According to Tsilimparis et al., conservative treatment with anticoagulation is preferred in patients with oncologic pathologies, coagulation disorders and sessile thrombi, reserving surgical, or endovascular intervention for cases with mobile thrombi or sessile ones with recurrent embolism despite optimal anticoagulant treatment6. In the present case, although the patient presented a cerebral embolic event due to multiple mobile thrombi, the fact that she was the carrier of a chronic myeloproliferative syndrome with risk of recurrent thrombosis, motivated the decision of a conservative treatment, which was successful, as no further thromboembolic events were repeated, and subsequent computed tomography controls demonstrated thrombus size regression and disappearance of their intraluminal component. Regarding anticoagulant treatment with direct oral anticoagulants (DOACs) in myeloproliferative neoplasms patients, evidence-based literature is scarce. Although the use of vitamin K antagonists (VKAs) is most common in this population, DOACs may be a reasonable alternative. Observational studies that have compared DOACs versus VKAs in myeloproliferative neoplasms patients have found no differences in recurrent thrombotic events and bleeding rates8,9. In conclusion, aortic thrombosis must be suspected in every embolic event, being uncommon in the absence of aneurysm or atherosclerosis. In this clinical setting, malignancy and hypercoagulability disorder must be ruled out as possible underlying pathology. A multi-imaging and multidisciplinary approach is essential for an accurate diagnosis and an adequate choice of the best treatment for each patient.











 nueva página del texto (beta)
nueva página del texto (beta)


