Clinical cases
Ectopic spleen in testicular parenchyma: case report
Bazo ectópico en parénquima testicular: reporte de caso
Alessandro Vengjer, Conceptualization, Acquisition funds, Research, Project administration, Supervision, Validation, Writing-reviewing and editing1
 http://orcid.org/0000-0002-0990-2233
http://orcid.org/0000-0002-0990-2233
Angelo Sementilli, Conceptualization, Research, Writing-reviewing and editing1
 http://orcid.org/0000-0002-8025-1517
http://orcid.org/0000-0002-8025-1517
Fernando Oliveira dos Santos, Data curation, Research, Original writing-draft1
*
 http://orcid.org/0000-0002-8497-8086
http://orcid.org/0000-0002-8497-8086
Giulia Francis Delgado dos Santos, Methodology, Original writing-draft1
 http://orcid.org/0000-0002-4231-330X
http://orcid.org/0000-0002-4231-330X
Ana Carolina de Abreu Gomes, Formal Analysis, Software, Original writing-draft1
 http://orcid.org/0000-0002-3550-2444
http://orcid.org/0000-0002-3550-2444
Guilherme Ribeiro Nader, Visualization, Original writing-draft1
 http://orcid.org/0000-0002-8301-2976
http://orcid.org/0000-0002-8301-2976
1Universidade Metropolitana de Santos, Santos, Brasil
Abstract
Clinical case description:
This report presents the case of a 32-year-old man with palpable solid nodule in the left testicle with a diagnostic hypothesis of testicular cancer, which turned out to be splenic tissue through pathological anatomy analysis.
Relevance:
The splenogonadal fusion is a rare and benign congenital anomaly related to the presence of ectopic spleen tissue in the gonadal parenchyma, caused by fusion between these two tissues during the fifth or sixth week of embryonic development. This condition is of great importance because its diagnosis is difficult and often confused with other gonadal disorders such as testicular neoplasm.
Clinical implications:
The most common consequence of this testicular disorder is the unnecessary orchiectomy, in which a variety of cases are submitted. To avoid testicle removal, intraoperative pathological examination can be used in these cases.
Conclusions:
The ectopic spleen in testicular parenchyma is a rare condition and its diagnosis is difficult. It is important to consider this condition as a differential diagnosis in testicular disorders, especially in the case of diagnostic hypothesis of testicular cancer, so that testicle removal can be prevented by the use of intraoperative pathological exam.
Keywords: ectopic spleen; testicular mass; splenogonadal fusion; orchiectomy; testicular cancer
Resumen
Descripción del caso clínico:
En este reporte se presenta el caso de un hombre de 32 años con nódulo sólido palpable en testículo izquierdo con hipótesis diagnóstica de cáncer de testículo, que en realidad la anatomía patológica descubrió que se trataba de tejido esplénico.
Relevancia:
La fusión esplenogonadal es una anomalía congénita rara y benigna relacionada con la presencia de tejido esplénico ectópico en el parénquima gonadal, causada por la fusión entre estos dos tejidos durante la quinta o sexta semana de desarrollo embrionario. Esta condición es de gran importancia porque su diagnóstico es difícil y muchas veces se confunde con otros trastornos gonadales como la neoplasia testicular.
Implicaciones clínicas:
La consecuencia más frecuente de este trastorno testicular es la orquiectomía innecesaria, a la que se someten diversos casos. Para evitar la extirpación del testículo, en estos casos se puede utilizar el examen patológico intraoperatorio.
Conclusiones:
El bazo ectópico en parénquima testicular es una entidad rara y de difícil diagnóstico. Es importante considerar esta condición como un diagnóstico diferencial en los trastornos testiculares, especialmente en el caso de la hipótesis diagnóstica de cáncer testicular, para que la extracción del testículo pueda ser evitada mediante el examen patológico intraoperatorio.
Palabras clave: Bazo ectópico; masa testicular; fusión esplenogonadal; orquiectomía; cáncer testicular
Introduction
Splenogonadal fusion is a rare and benign congenital anomaly, related to an abnormal association between splenic and gonadal tissues, or with mesonephric remains during the embryonic period.1,2 The first case was described by Boestrom in 1883 and since then less than 200 cases have been published in the literature.2
The condition occurs predominantly on the left side and in young men, with an average of 14.3 for them, against 1 for women. However, the difficulty of identifying ovarian cases based on their location can distort this prevalence.1,3
The exact cause of this pathology is not yet known, but fusion is believed to occur between the fifth and sixth weeks of gestation, before testicular descent. It is usually an accidental finding during a search for inguinal hernias or cryptorchidism.1
Its treatment is controversial, because for some authors, surgery is mandatory to confirm the diagnosis and exclude the possibility, even if rare, of a neoplasm. For others, abstention may be the ideal choice if the anomaly is detected and does not manifest clinically.2
Case report
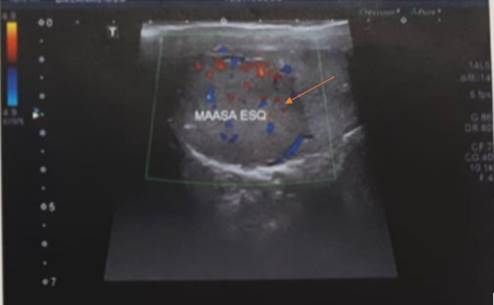
A 32-year-old male patient, white, without comorbidities or history of previous surgeries, who noticed a palpable solid nodule in the left testicle, without scrotal enlargement, looked for a urologist who performed color Doppler ultrasound of the testes, confirming the mass (Figure 1).
Beta-hCG, alpha-fetoprotein and lactic dehydrogenase tests were normal. With the hypothesis of seminomatous testicular cancer without signs of metastases established, he underwent a left orchiectomy without complications (Figure 2).
The anatomopathological examination showed that the nodule was actually splenic tissue (Figure 3).
Discussion
According to Putschar and Manion, there are two possible classifications for gonadal fusion: continuous and discontinuous (as occurred in this case). In the first type, a cord connects the spleen to the gonad and corresponds to 55% of cases, is associated with cryptorchidism and malformations such as micrognathia, heart defects and fivefold increase in the concomitant limb. In the second there is no connection, so the spleen is in a separate capsule and is not associated with other malformations. Clinically there are no significant differences between them.4-6
Splenogonadal fusion can affect both sexes, but is more common in males. In this case, a common symptom is testicular swelling, and there may be a scrotal mass, as in the patient reported, and intestinal obstruction.7
Around 37% of the cases reviewed by Karaman and Gonzales underwent unnecessary orchiectomy, due to the suspicion of a primary testicular neoplasm, as in the case reported.3 In this way, fusion may present similarly to testicular cancer, and the diagnosis before performing a surgical and histological procedure is difficult, especially in discontinuous cases.6
Imaging exams are inconclusive, because the findings of splenogonadal fusion and testicular tumors are very similar.6 Scrotal ultrasound is not sufficiently accurate in the preoperative period, as well as magnetic resonance imaging.4 On the other hand, splenic scintigraphy with technetium-99m is a good option when there is suspicion of fusion, as there is fixation of the radioisotope in the spleen and in the ectopic tissue, confirming the suspected origin.2,4 Another option that can be considered in order not to miss this diagnosis is intraoperative frozen section when the lesion is not so characteristic of a neoplasm.
So, the diagnosis of splenogonadal fusion prior to a surgical and histological procedure is difficult, as it typically presents as an asymptomatic or acutely painful testicular mass and edema.4 Thus, the anomaly is usually an accidental finding, established during a search for inguinal hernias or cryptorchidism.1 Therefore, it is important that this condition is also remembered in the diagnosis of testicular masses, so that intraoperative pathological examination can be performed in order to avoid unnecessary orchiectomy.7
The treatment of this condition is controversial, as for some authors surgery is mandatory to confirm the diagnosis.2 If surgery is chosen, orchiectomy is not indicated, since the splenic tissue is easily removed from the gonads, and usually takes the complete cure of the patient.2,7 For other authors, abstention may be the ideal choice if the anomaly is detected and does not manifest itself clinically.2
Conclusions
The ectopic spleen in testicular parenchyma is a rare condition and its diagnosis is difficult since it appears as an asymptomatic mass or with unespecific symptoms, such as testicular edema. Thus, it is important to consider this condition as a differential diagnosis in testicular disorders, especially in the case of diagnostic hypothesis of testicular cancer, so the testicle removal can be prevented by the use of intraoperative pathological exam with frozen section. Regarding the exposed, this case report might be helpful in future urologic investigations.
References
1 Chen G, Wang X, Zhao Y, Zhu L, Tang D. Splenogonadal fusion: a case report and review of the literature. BMC Urology. 2021;21(1):16. doi: https://doi.org/10.1186/s12894-021-00781-z
[ Links ]
2 Kadouri Y, Carnicelli D, Sayegh HE, Benslimane L, Nouini Y. Pathogenesis, Diagnosis, and Management of Splenogonadal Fusion: A Literature Review. Case Reports in Urology. 2020;2020:1-7. doi: https://doi.org/10.1155/2020/8876219
[ Links ]
3 Khairat ABM, Ismail AM. Splenogonadal fusion: case presentation and literature review. Journal of Pediatric Surgery. 2005;40(8):1357-60. doi: https://doi.org/10.1016/j.jpedsurg.2005.05.027
[ Links ]
4 Karray O, Oueslati A, Chakroun M, Ayed H, Bouzouita A, Cherif M, et al. Splenogonadal fusion - a rare cause of scrotal swelling: a case report. Journal of Medical Case Reports. 2018;12(1):172. doi: https://doi.org/10.1186/s13256-018-1712-1
[ Links ]
5 Li W-F, Luan M-X, Ma Z, Chen Y-J. Splenogonadal fusion: Report of four cases and review of the literature. Experimental and Therapeutic Medicine. 2013;6(3):816-8. doi: https://doi.org/10.3892/etm.2013.1207
[ Links ]
6 Hartman NC, Trabzonlu L, Barkan GA, Quek ML. Splenogonadal Fusion: A Rare Mimicker of Malignancy. Case Reports in Surgery. 2022;2022:e2791305. doi: https://doi.org/10.1155/2022/2791305
[ Links ]
7 Bekar E, Yalta T, Yarici H, Dogdas A, Tuncer Y. Ectopic splenic tissue in the testis: A case report. Afr J Urol. 2009;15(3):180-2. doi: https://doi.org/10.1007/s12301-009-0032-5
[ Links ]











 nueva página del texto (beta)
nueva página del texto (beta)





